行政院國家科學委員會專題研究計畫 期末報告
市場競爭,醫療選擇,和醫療品質:以透析治療為例(第 2
年)
計 畫 類 別 : 個別型
計 畫 編 號 : NSC 99-2410-H-004-052-MY2
執 行 期 間 : 100 年 08 月 01 日至 101 年 10 月 31 日
執 行 單 位 : 國立政治大學財政系
計 畫 主 持 人 : 連賢明
報 告 附 件 : 出席國際會議研究心得報告及發表論文
公 開 資 訊 : 本計畫可公開查詢
中 華 民 國 102 年 02 月 11 日
中 文 摘 要 : 近年來末期腎臟病治療(俗稱洗腎)的健保費用逐年攀高。
為了降低逐年攀升洗腎治療費用,健保局於 2006 年起採用
一系列政策鼓勵腹膜透析治療。但即使經健保局大力推廣
後,腹膜透析比例也僅從 2006 的 7.5%上升至 2007 的
8.5%,絕大多數還是採用血液透析,顯示台灣洗腎病患對腹
膜透析的接受程度有限。
本計畫主要目的在於瞭解台灣腹膜透析使用比例為何如此
低。在第一年計畫討論兩種透析方式是否存在療效上差異。
現有文獻普遍認為這兩種透析治療療效大致相同,但這些研
究多半以病患選擇後結果做比較。由於腹膜透析病患需在家
進行治療,平均個人健康上較血液透析病為佳,直接分析可
能存在偏誤。估計結果顯示在迴歸分析中,腹膜透析病患的
存活年數稍較血液透析為佳,但這成效差距在使用工具變數
估計後並消失。在第二年的計畫中討論這差異是否來自於醫
療供給端。台灣在 2008 年共有 517 院所提供血液透析,其
中僅有 99 家提供腹膜透析,即使是在激烈競爭下,願意提
供腹膜透析院所仍相當有限。我們先檢驗供給院所數目是否
對病患醫療品質造成影響,發現每多增加一家洗腎院所,病
患死亡率會顯著下降約 0.4%。然而,這些競爭並沒有刺激供
給者提供不同治療方式(腹膜透析)。
中文關鍵詞: 末期腎臟病、血液透析、腹膜透析、技術採用、工具變數
英 文 摘 要 : In recent years, dialysis treatment has become one of
the fast-growing expenditure components in national
health insurance. To contain the rising expenditure
of dialysis treatment, Bureau of National Health
Insurance (BNHI) since 2006 has initiated a series of
policies to encourage end-stage renal disease (ESRD)
patients to adopt peritoneal dialysis (PD). In spite
of their efforts, the take up rate of peritoneal
dialysis (PD) within ESRD patients continues to be in
the low ends, rising only slightly from 7.5% in 2006
to 8.5% in 2007, showing the vast majority of ESRD
patients still favoring hemodialysis (HD) over PD.
The purpose of this project is to understand why the
take-up rate of PD is so low in Taiwan. One
explanation is that the treatment effect of HD is
superior to that of PD. Although many researches have
argued that the survival of HD and PD patients are
approximately the same, those findings are based on
the observations of patients who had various
treatment methods. Given that HD patients on average
are younger and by the large employed, it is
plausible that the regression estimates are biased.
In the first year of this project, we employ
instrument variable method to compare the treatment
effect between HD and PD. Our regression results
indicate PD patients on average have slightly better
years of survival than HD patients, but the
difference disappeared when employing IV estimates.
Another explanation is that the health providers
simply are unwilling to offer PD treatment. In 2008,
there are 517 clinics or hospitals providing HD
services, while only 99 offering PD services. Even in
the urban area, there are only very few suppliers
willing to provide PD services. In the second year,
we examine how the market competition affects the
quality of care, as well as the availability of
treatment choices. Results indicate that the number
of health providers is positively associated with the
patient's survival---an increase of one health
provider reduces the 5-year mortality rate of ESRD
patients by 0.4%. Nonetheless, there is no evidence
showing market competition leads to the availability
of PD treatment.
英文關鍵詞: end-stage renal disease, peritoneal dialysis,
hemodialysis, technology adoption, instrumental
variable method
1
1.
前言
近年來,末期腎臟病(End-Stage Renal Disease,ESRD)治療(即俗稱洗腎)的健保費
用逐年攀高。根據健保局全民健保統計,洗腎醫療費用在 2002 年及 2003 年分別為 245 及
265億元,位居當年度單一治療項目中支出最高者。隨著洗腎費用逐年攀升,洗腎費用對基
層總額造成莫大壓力。為了舒緩基層總額點值壓力,2006 年起健保局將洗腎費用獨立為單
一總額,協商金額為 287 億元,佔當年健保支出之6.83%(全民健康保險醫療費用協定委員
會,2005);2008 年末期腎臟病透析治療醫療費用申報點數為318 億點
1,佔當年度總點數
7.89%(中央健保局,2007)。
洗腎治療費用逐年攀升的主要原因有二。第一,台灣的末期腎臟病患,不論在疾病盛行
率或發生率,均高居全球之冠
2。以 2006 年為例,台灣末期腎臟病患的發生率則為每百萬
人中有 418 人,在國際比較位居首位(見圖一)。若將發生率轉算成洗腎人口數,每年約
新增8000~8500 名的洗腎病患
3。由於末期腎臟病患的腎功能具有不可逆性質
4,一旦病患需
透過洗腎維持腎臟功能,該病患須持續接受透析治療;再加上台灣透析照護品質不錯,病患
平均的存活率較許多國家為佳,反導致台灣洗腎盛行率居高不下
5,截至今年年底,洗腎人
口已達 5 萬 8 千餘名(台灣腎臟基金會,2008)。
第二個原因在於末期腎臟病患的透析治療費用相當昂貴。病患一旦腎功能衰竭後,除接
受換腎外,便須持續接受透析治療。以目前台灣最普遍血液透析治療為例,健保局單次給付
4100 元,每個病人每月平均需進行 13 次血液透析,每人每年必須花費57.8 萬元的醫療費
用(中央健保局,2005)。這也是雖然洗腎人口僅佔台灣總人口的0.2%,卻需花費約8%健
保預算的主要原因。事實上,研究指出只要新進病患延緩一年進入洗腎療程,健保局一年可
省下 42.75 億透析治療費和近 60 億元的門住診費用(雷秀麗,2001),透析治療對健保財
務壓力不言而喻。
基於末期腎臟病的高發生率,不少研究試圖解釋台灣洗腎病患發生率為何偏高。傳統醫
界看法,認為人口老化和濫服西藥(如止痛劑或消炎藥)
6是末期腎臟病發生率偏高主因(台
灣腎臟醫學會,2005)。近年來研究指出台灣國民常自行購買中藥(草藥或藥丸)服用,或
透過地下電台購買中藥成藥,這些中藥未經醫師核可,可能不當加重腎臟負擔;特別是當這
些中藥含馬兜鈴酸成分
7,容易導致腎臟病變(Lord et al, 1999;Takana et al,2001;Yang Et
1 有關重大傷病範圍,請參閱健保局網頁(http://www.nhi.gov.tw/information/bulletin_file/466_bbs0830-1-1.doc) 2
根據美國 USRDS 協調中心(USRDS Coordinating Center)所出版年度報告,2006 年盛行率前三名國家分別為台灣,日 本,和德國;發生率前三名國家則為台灣,美國與墨西哥。也就是說,台灣洗腎人口,不論是發生率與盛行率,均列名世 界第一。 3 參見台灣腎臟基金會網頁所公佈之台灣歷年洗腎人口圖(http://www.kidney.org.tw) 4 此處指慢性腎衰竭病患。急性腎衰竭而病患有些需須接受短期洗腎,但這些治療通常不超過三個月。 5 台灣 2006 年末期腎臟病盛行率為每百萬人中 2226 人(見圖一) 6
文獻已證實四十種類西藥(Palmer et al. 2004),包括非類固醇消炎藥(NSAIDs)(Elseviersand De Broe,1995), aminoglycoside(Leehey et al.,1993), 以及 cisplatin(Kim et al,1993),有較大腎臟毒性。參見王榮德(2008)。 7 1991 年,比利時醫師 Vanherweghem 發現兩個特殊案例(Vanherweghem et al,1993)。兩名婦女從布魯塞爾的某減肥診 所服用減肥中草藥後,發現有快速進行性纖維化間質腎炎,近乎末期腎衰竭的情形。這些婦女過去並未有腎臟病的病史, 她們在第一次就醫後很快就接受血液透析治療。在進一步的流行病調查後又發現另外七名女性病例,年齡皆小於 50 歲, 她們都在同一家診所接受某種減肥藥。這些患者的腎臟切片檢查發現有廣泛性的腎間質纖維化病變,並無腎絲球病變。調 查發現這間診所在 1990 年 5 月處方改變,醫師在原來處方中加入漢防己( Stephania tetrandra ) 厚朴( Magnolia officinalis ) 兩種含有馬兜鈴酸成分之中藥,而腎病變似乎是在新藥添加以後才開始發生,因而 Vanherweghem 推測這些病例的腎間質 纖維化與中草藥有關,隨後遂有學者命名為中草藥腎病變( Chinese herb nephropathy, CHNP )。
2
al.,2000;Arlt et al.,2002;Cosyns,2003;IARC,2002;Hsieh et al.,2008;王榮德,2008)
8
,但至今仍無研究能清楚刻畫中草藥成分與腎臟疾病間的因果關係;另有研究指出健保透
析治療給付過高和市場高度競爭,是造成洗腎病患發生率偏高原因(謝武吉,1999:張雁尊,
2002)
9。許績天與連賢明(2007)利用健保資料庫,從供給者誘發性需求(supplier- or
physician-induced demand, SID)角度,分析台灣洗腎醫療院是否會因為自身的利益,鼓勵末
期腎臟病患提早採用透析治療。但結果發現因供給者所誘發透析病人不高於整體的 2%,仍
不足以解釋台灣末期腎臟病的高發生率。
既然現有研究仍無法解釋慢性腎衰竭的高盛行率,在龐大洗腎費用壓力下,另一個途徑
是採用較便宜透析治療方式
10。現有透析治療方式有兩種:血液透析與腹膜透析。所謂血液
透析,指透過『動靜脈瘻管術』(利用手術將手臂上動脈和靜脈接合),將血液引流經過『人
工腎臟器』洗淨,排除代謝廢物,再將洗過血液流回體內;所謂腹膜透析是利用人體天然的
半透膜---腹膜來進行淨化
11,以腹膜代替腎臟功能,經由透析藥水使用移除體內水分與廢物。
由於血液透析需透過機器進行體外血液引流,只能在有醫師監護下進行;腹膜透析治療法相
對較溫和,患者可獨自在家操作,不需一星期到院所三次進行治療,且每月花費約為血液透
析 8-9 成。因此,倘若洗腎病患採用腹膜透析,每位健保洗腎支出可節省一成以上。
基於此,健保局自 2006 年開始,採取一系列政策鼓勵腹膜透析治療。2006 年將腹膜
透析藥水使用袋數放寬;2007 年和2008 年則直接於門診透析總額中,提撥10﹪品質保證款
用於「腹膜透析推廣獎勵計畫」,透過提高財務誘因,來獎勵醫師鼓勵病患選擇腹膜透析
12;
2008 年5 月起,另外補助腹膜透析病患每月兩千元的全自動腹膜透析儀租金,期望降低腹
膜透析病患的自費金額。但即使如此,台灣洗腎病患使用腹膜透析的比例相當低,表一列出
世界各國洗腎病患中使用血液透析和腹膜透析的比例。台灣腹膜透析比例在 2006 年前僅約
7%左右,在世界各國中位居末段,在亞洲國家中,鄰近的香港使用腹膜透析為 8 成,韓國
為 2 成,台灣可說是除日本外,亞洲開發國家中最低的。即使在 2006 年健保局大力推廣
後,也僅從 7.5%上升至 8.5%,增加幅度相當有限,顯示台灣洗腎病患對腹膜透析的接受程
度相當有限(楊五常,2009)。
基於此,本計畫的主要目在於瞭解腹膜透析為何在台灣洗腎病患間接受程度如此低。我
們考慮兩個可能性,第一是治療成效的差異。相較於血液透析,腹膜透析治療效果有可能較
差,以致病患不願意採用腹膜透析。現有文獻普遍認為腹膜透析因能保留部分腎功能,採用
腹膜透析病患在存活上不遜於血液透析病患。楊五常(2009)以台灣資料比較腹膜透析和血
液透析病患存活率,發現在第一年到第二年半期間,存活甚至高過血液透析,以後則相同
13。
8 Hsieh et al.(2008)利用健保資料庫 20 萬人歸人檔分析,發現 1997 至 2003 年間。台灣高達 1/3 人口曾服用含馬兜鈴 酸中草藥方。王榮德(2008)發現這些含馬兜鈴酸中草藥方,和某些族群(如女性,30-50 歲男性等)罹患腎臟相關疾病 關連性較高。 9 張雁尊(2002)發現市場競爭因素(如醫師密度,洗腎病床數)會顯著增加台灣洗腎醫療費用及次數。 10 除透析治療外,另一個治療方式是透過腎臟移植手術換腎。但由於台灣民眾有全屍習俗,活體腎臟取得相當不易,手術 換腎每年僅約百例,很難應付每年新增約八千例的洗腎病患。 11 腹膜是一層覆蓋在腹腔內壁及臟層上(包括胃肺脾臟及腸子)的薄膜。 12 依據全民健康保險醫療費用協定委員會 96 年 1 月 22 日費協字第 0965900116 號公告,門診透析服務品質保留款實施 目的有四個:1,降低末期腎臟疾病發生率:2,提升醫療品質,減少門診透析治療病人之併發症、病患之住院率、死亡率 及腹膜炎發生率等;3,加強推動 PRE-ESRD 預防性計畫及病人衛教計畫:4,推廣腹膜透析治療。其中推廣「腹膜透析推 廣獎勵計畫」分配本方案預算之 10%經費。 13 楊五常(2009)指出這結果主因是腹膜透析比較容易保留殘餘腎功能,仍可排出一些尿液,有助把毒素排出體外,體內
3
另外,由於腹膜透析病患可在家自行操作,不需一週三次前往洗腎院所治療,對有工作病患
在就業上有相當助益。但現有資料均以病患「自行選擇」後結果做比較,由於選擇腹膜透析
病患需自行在家進行透析治療,選擇腹膜透析病患應具備相當洗腎知識,且對自己身體狀況
較有信心
14,是否能從選擇後結果推論兩種透析的治療效果一致,仍是一個待回答問題。因
此,本計畫採用工具變數法(instrumental variable estimation, IV),來探求這兩種透析方法
對洗腎病患在存活時間上影響。
第二個則是市場競爭對醫療選擇影響。在醫療經濟研究中,許多討論 聚焦於市場競爭
如何影響醫療品質和費用(Dranove and Satterthwaite,1992;Dranove and Satterthwaite,2000;
Dranove,Shanley and White,1993;Dranove and White,1994;Gaynor and Vogt,2000)。
其中最有名假說,應屬 Robinson 和 Luft(1985)所提出的 Medical Arm Race(MAR)假
設。MAR 認為醫療保險扭曲了醫療價格,再加上醫療品質相當複雜,消費者會傾向以是否
具備先進技術來判定供給者品質,當醫院競爭越激烈時,昂貴儀器使用越多,反 增加無謂
資源使用。也因為 MAR 的假設,許多研究均針對市場競爭對醫療費用和品質進行 探討,
所得結果也相當分歧
(Baker,2001;Dranove,Shanley and Simon,1992;Kessler and McClellan,
2000;Lien,Chou and Liu,2006;Propper,Burgess and Green,2004;Robinson,Granick and
McPhee,1987;Robinson and Luft,1985;Robinson and Luft,1987;Shortell and Hughes,
1988;Town and Vistnes,2001)。相較這些研究,透析治療中,不論是血液或腹膜 透析,
是相當成熟技術,而非所謂昂貴檢查儀器,較少研究著重討論市場競爭對透析治療影 響;
更重要的,由於增加醫療選擇對消費者而言有利無弊,透過醫療選擇這個指標,可協助 我
們對醫療市場競爭結果,有更進一步瞭解。為了排除競爭指標內生性可能,我們計畫使用
Kessler and McClellan(2000)所設計的競爭指標,以分析市場競爭對醫療選擇的影響。
水份調節也比較穩定,不易水腫。病患維持殘餘腎功能,未來有機會接受腎臟移植手術時,存活率也會提高。 14 楊五常表示,病患選擇腹膜透析或血液透析,通常取決於醫療及病患本身。如果病患無合適的靜脈可做廔管、 交感神經功能不好,或有心臟衰竭毛病,容易在接受血液透析時出現低血壓,也容易因水分累積過多造成心臟 衰竭,就應考慮採腹膜透析。洗腎病患如有出血傾向,也不適合平均每兩天就扎一次針的血液透析,應以腹膜 透析為優先考量。
4 資料來源:USRD (2010)
5
6
表ㄧ:世界各國血液透析與腹膜透析比例 (續)
國名 2008 2009 2010 2008 2009 2010 2008 2009 2010 Argentina 96.0 96.0 95.8 0.0 0.0 0.0 4.0 4.0 4.2 Australia 68.6 69.6 71.4 9.4 9.3 9.1 22.1 21.1 19.5 Austria 91.0 91.0 91.0 0.0 0.0 0.0 8.9 8.9 9.0 Bangladesh 98.3 98.3 98.3 0.0 0.0 0.0 1.7 1.7 1.7 Belg/Dutch sp. 89.7 89.6 90.4 0.3 0.4 0.4 10.1 10.0 9.2 Belgium, Fr. Sp. 90.8 90.3 90.0 1.3 1.2 1.4 7.9 8.5 8.6 Bosnia/Herzegov. 95.1 94.9 95.2 0.0 0.0 0.0 4.9 5.0 4.8 Brazil 89.6 92.3 90.6 0.0 0.0 0.0 10.4 7.7 9.4 Canada 78.4 78.4 78.4 3.3 3.5 3.7 18.3 18.1 17.9 Chile 95.3 95.3 95.1 0.0 0.0 0.0 4.7 4.7 4.9 Colombia 68.0 68.2 68.7 0.0 0.0 0.0 32.0 31.8 31.3 Croatia 91.8 91.0 91.5 0.0 0.0 0.0 8.2 9.0 8.5 Czech Republic 91.8 92.0 92.1 0.0 0.0 0.0 8.2 8.0 7.9 Denmark 72.9 73.7 74.0 4.1 4.4 4.7 23.0 21.9 21.3 Finland 74.4 75.0 77.5 3.9 3.7 4.0 21.7 21.3 18.5 France 87.8 88.5 88.5 1.3 1.2 1.0 10.8 10.3 10.5 Greece 91.7 92.0 92.3 0.0 0.0 0.0 8.3 7.9 7.7 Hong Kong 20.4 21.5 23.5 0.4 0.6 0.9 79.2 77.9 75.6 Iceland 76.2 86.9 81.7 1.6 0.0 1.4 22.2 13.1 16.9 Israel 93.6 93.3 93.8 0.0 0.0 0.0 6.4 6.7 6.2 Jalisco (Mexico) 40.4 41.5 48.7 0.0 0.0 0.0 59.6 58.5 51.3 Japan 96.8 96.7 96.7 0.1 0.1 0.1 3.1 3.2 3.2 Rep. of Korea 81.0 83.1 84.4 0.0 0.0 0.0 19.0 16.9 15.6 Malaysia 90.0 90.3 90.6 1.0 1.0 1.0 9.1 8.7 8.4 Morelos (Mexico) 43.2 42.4 . 0.0 0.0 . 56.8 57.6 . Netherlands 77.4 79.1 79.5 2.5 2.5 2.7 20.1 18.4 17.9 New Zealand 48.1 48.4 47.2 15.7 16.5 17.7 36.2 35.0 35.0 Norway 83.4 80.7 81.3 0.3 0.5 0.7 16.4 18.8 18.0 Portugal 94.8 94.4 93.9 0.0 0.0 0.0 5.2 5.6 6.1 Romania 82.9 84.5 86.4 0.0 0.0 0.0 17.1 15.5 13.6 Russia 91.0 91.3 91.4 0.0 0.0 0.0 9.0 8.7 8.6 Scotland 82.4 83.5 84.3 2.3 2.5 2.4 15.4 14.0 13.3 Singapore 85.6 86.3 . 0.1 0.1 . 14.4 13.6 . Spain 90.6 90.6 89.8 0.3 0.2 0.2 9.2 9.2 10.0 Sweden 73.3 73.6 74.8 2.8 2.7 2.8 23.9 23.6 22.4 Taiwan 90.8 89.7 89.6 0.0 0.0 0.0 9.2 10.3 10.4 Thailand 90.5 84.1 81.9 0.0 0.0 0.0 9.5 15.9 18.1 Turkey 87.4 89.6 90.4 0.0 0.0 0.0 12.5 10.4 9.6 UK^ 81.2 82.2 82.3 2.1 2.5 3.0 16.6 15.3 14.7 United States 92.0 91.9 91.5 1.0 1.2 1.3 6.9 6.9 7.2 Uruguay 91.1 90.8 90.1 0.0 0.0 0.0 8.9 9.2 9.9 資料來源:http://www.usrds.org/ 血液透析 在家血液透析 腹膜透析7
第一年計畫
估計方法
本計畫在於評估腹膜和血液透析對病患存活影響。雖說國內外研究普遍認為腹膜透析,
不論以病患存活或就業來評估,療效均不亞於血液透析(楊五常,2009)。但由於比較基礎
是以病患透析治療選擇後樣本作基準,一般來說,自行選擇腹膜透析病患,通常身體狀況較
佳,且具備相當洗腎知識,在個人特性上和選擇血液透析病患存在基本差異。在這個情況下,
以兩組透析病患患者治療後結果比較,可能無法排除「選擇性偏誤」(selection bias)。基
於此,我們考慮下列估計模型:
(1)
O
it
0
X
it
1
H
it
2
3D
it
it其中
O 為病患透析治療效果。我們以病患
iti 在 t 期是否存活和是否就業,作為透析治療品質
指標;
X 為洗腎病患透析治療個人特性變量,包括病患年紀,性別,是否有糖尿病、高血
it壓、心臟病等;
H 為洗腎診所特性,包括院所規模(床數)、院所權屬(公立、私立、法
it人)、院所評鑑(醫學中心、區域醫院、地區醫院和診所);
D 為病患治療選擇(1為腹膜
it透析,0為血液透析)。由於台灣腹膜透析使用比例相當低(2007 年僅約8%),我們採較
寬鬆認定,將混合使用血液透析和腹膜透析的病患視為腹膜透析;最後,
it為一個不隨時間
和病患變動的隨機變數。
估計式(1)需解決下列幾點問題,涵蓋使用資料和估計方法。在使用資料方面,健保
資料並無法和其他外部資料串連,如此一來無法直接觀察到洗腎病患的存活時間;其次,我
們需從健保資料中取得病患個人特性(包括過去病史)、並串連院所特性,甚至醫師特性,
來協助分析。這些特性在分析醫療品質時不可或缺。最後,我們需判斷洗腎病人選擇腹膜透
析或血液透析進行透析治療。
我們採取下列方式來解決使用資料的問題。不同於許績天和連賢明(2007)利用重大傷
病門診費用檔中所記錄費用,來認定洗腎病患採用血液透析或腹膜透析。本計畫透過國衛院
健保資料特殊需求,選取洗腎病患歸人檔資料(包括門診費用檔、以及所對應門診醫令檔)。
這一方面能確實掌握病患透析治療方式,另一方面也避免使用重大傷病門診費用檔中僅涵蓋
透析治療相關服務,缺乏病患其他非洗腎醫療利用。這些其他醫療利用,可協助我們判斷病
患是否有其他併發症(如心臟病、高血壓、糖尿病)
。其次,我們採取Lien, Chon 和Liu(2008)
的方式,以健保保險的退保日期作為洗腎病患的死亡日期。
另一個問題在於估計方法。由於透析治療選擇是洗腎病患內生決定的,直接比較選擇腹
膜透析或和血液透析病患的醫療品質,會有內生性偏誤的疑慮;舉例來說,身體狀況比較好
的,選擇繼續工作的,可能在個人時間考量下,以腹膜透析來降低治療時所衍伸成本(如交
通成本);相反的,患有心臟病、高血壓、糖尿病等併發症的洗腎病患,在自身健康考量下,
會傾向選擇有醫師在旁監督的血液透析治療,直接比較治療後存活或就業狀況,無法瞭解兩
治療方式的療效差異。
為了解決這個內生性所引發的估計偏誤,本研究採工具變數法(Instrumental Variable
Method, IV)。透過IV 估計法,消除因內生性所引發的選擇性偏誤(selection bias)。但使
8
關,卻沒有影響洗腎病患的醫療結果。也就是說,
0
)
,
(
D
itZ
it
Cov
and
Cov
O
it,
it
0
自 McClellan et al(1994)後,病患距離院所的最近距離已普遍被當作工具變數使用,
由於透析治療中,提供透析治療的院所數目遠小於血液透析院所(見表二),這些可供腹膜、
血液透析院所的距離差距,應會影響使用腹膜透析治療的機率,協助我們分析不同治療下的
洗腎病患存活和就業影響。另外,由於這些距離工具變數不只一個:最近腹膜透析診所距離,
最近血液透析診所距離,以及這些距離的平方項等,可採過度認定檢定(over-identification
test),檢驗這些工具變數的有效性。
表二:2005年到2009年透析治療院所數
年 血液透析 腹膜透析 血液透析 腹膜透析 血液透析 腹膜透析 血液透析 腹膜透析 血液透析 腹膜透析 醫學中心 台北分局 9 6 9 8 9 8 9 8 9 8 北區分局 3 1 2 1 2 1 2 1 2 1 中區分局 4 4 3 3 3 3 3 3 3 3 南區分局 2 2 2 2 2 2 2 2 2 2 高屏分局 3 3 3 3 3 3 3 3 3 3 東區分局 1 1 1 1 1 1 1 1 1 1 小計 22 17 20 18 20 18 20 18 20 18 區域醫院 台北分局 20 11 18 10 18 14 18 14 19 15 北區分局 11 6 11 7 11 8 11 9 11 9 中區分局 14 6 15 8 15 10 15 11 15 12 南區分局 13 8 13 9 13 9 12 9 12 9 高屏分局 10 7 10 7 11 8 11 8 10 8 東區分局 5 1 4 2 4 2 5 2 5 2 小計 73 39 71 43 72 51 72 53 72 55 地區醫院 台北分局 37 1 38 1 39 4 40 5 39 9 北區分局 25 1 27 2 29 2 29 2 27 3 中區分局 37 0 40 0 40 5 40 6 40 10 南區分局 19 0 18 1 18 3 18 3 21 4 高屏分局 35 1 35 1 36 1 32 1 32 2 東區分局 3 0 3 0 4 1 5 1 5 1 小計 156 3 161 5 166 16 164 18 164 29 基層診所 台北分局 68 0 67 0 74 1 75 2 80 3 北區分局 19 0 25 0 26 1 29 1 33 1 中區分局 41 0 44 1 49 4 52 4 54 4 南區分局 43 0 48 0 51 2 54 4 57 3 高屏分局 35 0 37 0 42 0 48 0 54 0 東區分局 4 0 4 0 4 0 4 0 5 0 小計 210 0 225 1 246 8 262 11 283 11 總計 461 59 477 67 504 93 518 100 539 113 高屏分局轄區:高雄市、屏東縣、澎湖縣 東區分局轄區:花蓮縣、台東縣、綠島、蘭嶼 2005 2006 2007 2008 2009 資料來源:健保局96.98年門診透析總額品質報告(數據由台灣腎臟醫學會提供) 說明:台北分局轄區:臺北市、新北市、基隆市、宜蘭縣、金門縣、連江縣 北區分局轄區:桃園縣、新竹市、新竹縣、苗栗縣 中區分局轄區:台中市、彰化縣、南投縣 南區分局轄區:雲林縣、嘉義市、嘉義縣、台南市9
樣本特性
本研究使用國衛院發行健保資料庫,透過特殊申請方式取得洗腎病患自健保開辦後透析
治療利用(包括門診費用檔和門診醫令檔),並據此認定洗腎病患所使用的透析治療(血液
透析或腹膜透析或兩者金兼有)。為方便認定透析治療方式,我們將一年內使用申報超過兩
次腹膜透析病患認定為採腹膜透析病患,其餘則為血液透析病患。表三為 1997 至 2009 年
新增透析病患中,第一年治療選用血液透析和腹膜透析人數。由表三可知,台灣透析病患由
1997 年的五千餘人,成長到 2001 年約七千人,並於 2005 年突破八千人,顯示台灣的末
期尿毒症病患發生率的確逐年升高。而這些新增病患中,在 2006 年以前超過九成以上選用
血液透析治療。自從健保局於 2006 年採一系列政策鼓勵腹膜透析治療後,新增病患選用腹
膜透析比例開始有上升趨勢,但仍在全部新增病患的一成五以下。
除醫療利用資料外,目前已將醫療利用資料串連醫院基本檔資料(醫院資料基本檔,醫
事人員基本資料檔、與專科醫師證書主檔),來取得醫院特性(包括醫院權屬,醫院層級,
以及醫院規模);並串連病患基本資料檔(承保檔)取得病患投保類別(公、勞保),和退
保日期來推估其就業與否和死亡日期。由於本研究擬使用距離當作工具變數,需知道病患居
住鄉鎮和透析治療鄉鎮來計算病患的就醫距離。礙於健保資料中沒有紀錄病患居住鄉鎮,目
前選用投保類別為地區人口和農保兩個投保類別病患作為分析樣本,以取得可靠居住鄉鎮資
料來計算就醫距離。目前正以廻歸分析和工具變數法兩種估計方法,分析不同治療方法對存
活和就業的影響。
表三:台灣1997年到2009年新增透析治療病患數
血液透析
腹膜透析
全部人數
1997
4,930
465
5,395
1998
5,516
290
5,806
1999
5,744
400
6,144
2000
6,182
463
6,645
2001
6,455
516
6,971
2002
6,907
514
7,421
2003
6,904
598
7,502
2004
7,089
647
7,736
2005
7,597
667
8,264
2006
7,127
839
7,966
2007
7,282
1,119
8,401
2008
5,093
884
5,977
說明:2008 新增病患僅計算至 2008 年九月前10
表四可看出腹膜透析新增病患所花費平均費用較血液透析新增病患低一萬元左右,在龐
大健保支出缺口壓力下,健保局推廣腹膜透析的動機應該不低。各年腹膜透析洗腎新增病患
中,年齡分布的部分可以看出,45 歲以下的比例較高。以 2002-2004 年的腹膜透析新增病患
為例 45 歲以下佔 31.81%,最高,其次,為 45-55 歲佔 25.29%,55-65 歲佔 16.81%,65-75
歲佔 15.55%,75 歲以上 10.53%。再則這些病患以台北、北部及中部就醫較多。以 2002-2004
年的腹膜透析新增病患為例,台北區域就醫佔 38.18%,北部醫院就醫 12.25%,中部醫院就
醫 30.95%,南部醫院就醫 10.05%,高屏醫院就醫 6.76%,東部醫院就醫 1.81%‧再由表中
可以看出,新增病患在台北就醫的人數一直增加由第三多的就醫區域晉升為第一,北部醫院
則由第一降至第三,中部區域雖比例變動不大,但是幅度不及台北的增加幅度。最後,也是
最重要的,在存活率的部分並不容易區分血液透析還是腹膜透析新增病患較高,因為差距皆
不大。
估計結果
本研究以每年新增透析病患來檢驗透析治療品質。表五為用 probit 模型的估計結果。在
病患特性變數的年齡方面,我們可以發現四組年齡在三個迴歸式下的係數均為負且顯著,表
示當樣本為 45 歲以上時,相對樣本在 45 歲以下的病患其一年存活率較低,且其對三年存活
率和五年存活率相較 45 歲以下病患亦較低。一般來說,年紀愈大的病患身體狀況可能愈差,
因此此結果符合我們的預期。而性別變數在三個迴歸式下的係數也都為負,代表當樣本為男
性時,相對樣本為女性來說其一年、三年及五年的存活率都較低。
在醫療院所特性變數的院所權屬方面:法人和私立院所相較於公立院所而言,其一年存
活率及三年存活率都是較低的,但並不顯著;在院所評鑑方面:區域醫院及地區醫院相較於
醫學中心來說其五年的存活率是較高的;而基層診所的三個迴歸係數都為正值且顯著,表示
基層診所相對醫學中心而言,其一年、三年及五年的存活率都較高,這也可能歸因於診所的
透析病患通常病況較輕,因此有相對較高的存活率。至於以病床數衡量醫院規模方面,可以
發現 500 至 1000 及 1000 張床數以上院所,相對於 500 張床數以下院所有較高的五年存活率。
最後,關鍵的透析方式係數在三個迴歸式中都為正且顯著,表示當樣本為採用腹膜透析時其
相對採用血液透析樣本的各年存活率都較高。
最後,表六為使用工具變數後的估計結果。我們選用病患距離院所的(血液、腹膜透析
院所)最近距離為相關工具變數。在使用工具變數後,不論是一年、三年及五年的存活機率,
在不同透析方式差距均呈現不顯著,顯示不同透析方式對醫療成效並沒有太大影響。
11
表四:透析新增病人敘述統計
腹膜透析新增病人
血液透析新增病人
1997-1998 1999-2000 2001-2002 2003-2004
1997-1998 1999-2000 2001-2002 2003-2004
每月平均費用
28,183.5
28,154.5
29,837.2
29,120.6
40,589.0
38,884.2
39,552.9
39,331.0
[17,738.7] [17,738.7]
[10,653.8]
[12,406.8]
[19,594]
[17,924.5]
[17,176]
[17,181.0]
年紀
45 以下
40.36%
38.21%
37.01%
31.81%
22.73%
17.47%
14.87%
12.78%
45-55
17.29%
18.17%
24.15%
25.29%
18.73%
18.12%
19.72%
19.57%
55-65
18.87%
21.12%
16.99%
16.81%
25.94%
24.88%
23.53%
22.87%
65-75
16.88%
13.75%
13.50%
15.55%
23.43%
25.93%
27.23%
27.17%
75 以上
6.60%
8.74%
8.36%
10.53%
9.17%
13.60%
14.64%
17.61%
性別
女性
54.64%
54.70%
58.09%
56.96%
51.72%
52.56%
52.12%
51.20%
男性
45.36%
45.30%
41.91%
43.04%
48.28%
47.44%
47.88%
48.80%
就醫醫院區域
台北
21.04%
25.64%
32.14%
38.18%
29.16%
29.03%
27.94%
27.77%
北部
30.43%
28.29%
12.21%
12.25%
13.78%
14.05%
14.26%
13.34%
中部
31.56%
29.57%
36.91%
30.95%
18.15%
17.68%
17.56%
18.47%
南部
7.13%
3.93%
7.35%
10.05%
17.30%
17.81%
17.50%
18.43%
高屏
9.16%
10.61%
9.55%
6.76%
19.14%
19.25%
20.37%
19.23%
東部
0.68%
1.96%
1.84%
1.81%
2.47%
2.18%
2.37%
2.76%
五年存活率
92.41%
95.97%
95.32%
97.41%
91.29%
94.42%
95.80%
96.59%
病人數
884
1,018
1,089
1,273
12,215
13,832
15,230
15,963
說明:[ ]內為平均費用標準差。
12
表五:存活率迴歸分析
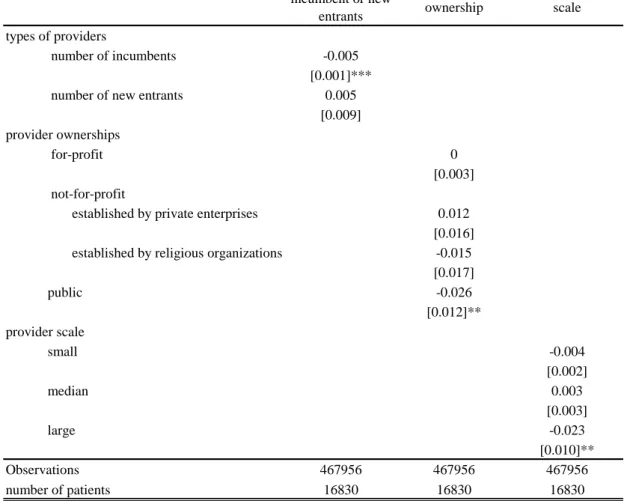
一年存活率 三年存活率 五年存活率 年紀 45-55 -0.174*** -0.195*** -0.200*** [0.036] [0.028] [0.025] 55-65 -0.409*** -0.411*** -0.410*** [0.033] [0.026] [0.024] 65-75 -0.564*** -0.574*** -0.573*** [0.032] [0.025] [0.023] 75以上 -0.800*** -0.739*** -0.689*** [0.032] [0.026] [0.024] 性別 -0.080*** -0.060*** -0.063*** [0.015] [0.012] [0.012] 院所權屬 法人 -0.011 -0.007 0.01 [0.022] [0.019] [0.017] 私立 -0.022 -0.012 -0.011 [0.026] [0.022] [0.020] 院所評鑑 區域醫院 -0.011 0.007 0.051** [0.029] [0.024] [0.023] 地區醫院 -0.024 0.002 0.059* [0.040] [0.034] [0.032] 基層診所 0.097** 0.118*** 0.177*** [0.044] [0.037] [0.035] 病床數 500-1000 0.002 0.022 0.041* [0.027] [0.023] [0.021] 1000以上 -0.018 0.047 0.088*** [0.035] [0.029] [0.028] 就醫醫院區域 北部 -0.002 0.018 0.029 [0.024] [0.020] [0.019] 中部 0.006 0.024 0.039** [0.023] [0.019] [0.018] 南部 0.026 0.032* 0.030* [0.023] [0.019] [0.018] 高屏 0.017 0.032* 0.042** [0.023] [0.019] [0.018] 東部 -0.045 -0.055 -0.032 [0.048] [0.039] [0.037] 透析方式 0.134*** 0.092*** 0.125*** [0.033] [0.026] [0.025] 常數項 2.318*** 1.982*** 1.787*** [0.050] [0.041] [0.037] Observations 108361 108361 108361 說明:括號內為標準差 *,** 與***:為在10%, 5%與1% 的顯著水準下, 估計係數顯著異於0第二年計畫
1
Introduction
Recently, there is an increasing pattern on both prevalence and incidence rate of
end-stage renal disease (ESRD) in developed countries (Dor et al., 2007). Possible reasons for this increasing pattern include the aging of the population, increasing diabetes rate, improved survival from heart disease, and greater acceptance to dialysis therapy (Dor et al., 2007). Furthermore, since ESRD refers to an irreversible kidney failure and a patient can not stop his dialysis treatments for his resting of life, this leads ESRD be a costly and debilitating medical
condition15. This feature attracts significant amount of attentions of researchers.
There are several dimensions in the existing related studies. The first dimension is to estimate medical costs ( Escarce and Feldman, 1999; Manns et al., 2003; Jang, 2003;
Chodicket al., 2005). Some of studies in this line focus on the estimation of costs for the most related illness that leads to chronic kidney failure, such as diabetes. For example, Chodick et al. (2005) and Jang(2003). Some of them discuss its future treatment costs based on the irreversibility of ESRD (Manns et al., 2003). In addition, due to its feature of irreversibility, the treatment outcome is directly related to a patient’s quality of life. The second dimension of studies emphasizes on the treatment qualities (Irvin, 1998; Escarce and Feldman, 1999; Dor et al., 2007) and survival rates after treatments (Mesler et al. 1999). The third dimension tries to investigate the efficiency of a dialysis center (Barnett et al., 1993; Ozgen and Ozgen, 2002). Lastly, the fourth and the newly dimension evaluates the economic incentives on various target variables, such as health outcome, expenditures, and utilizations (Ashton and Marshall, 2007; Dor et al., 2007; Durand-Zaleski et al., 2007; Fukuhara et al., 2007; Harris, 2007; Hirth, 2007; Kleophas and Reichel, 2007; Luño, 2007; Manns et al., 2007; P Nicholson and Roderick, 2007; ontoriero et al., 2007; Van Biesen et al., 2007; and Wikström et al., 2007). There are several incentives under investigation, such as incentives created by different payment methods, and incentives from different dialysis organizational forms. These incentives are mainly from provider sides. Actually, there is still one incentive from the
15
In the U.S., the expenditure of dialysis treatments for Medicare enrollees rises from $16.9 billions in 2002 to $20.1 billions in 2004 (USRDS, 2006), while in Taiwan, the expenditure increases 6.84% from $0.7 billions in 2002 to $0.9 billions in 2006 (NHIHCAC, 2006).
2
patient side. There are two kinds of patient incentives. The first is the incentives created by different level of co-payment, and the second is the patient incentive when a patient has more than one provider choice. Though there are great amount of attentions on the first part of patient incentives, none of these draws an analysis on the impact of incentives on the patient side when a patient has more choices of providers.
In this paper we analyze the impact of a patient’s choice feasibility on ESRD patients. We use Taiwan data because Taiwan implemented National Health Insurance (NHI) in 1995, the latest developed country to offer insurance coverage. Under Taiwan’s NHI scheme, all ESRD patients can receive related treatments without any co-payment. Therefore the utilization of medical cares will not be affected by a patient’s income situation which then reduces the potential selection bias when estimating a patient’s survival. We use longitudinal outpatient claims of NHI receipts diagnosed as new ESRD patients during 1997 and 2003. Since around 92.3% of Taiwan’s ESRD patients use hemodialysis as their therapy. In this paper we only focus on new ESRD patients with hemodialysis. For the patient’s death
information, the identification strategy is to use the features of irreversibility and continuity of ESRD dialysis treatments and a patient’s enrollment registry record. Because an ESRD patient’s kidney function is permanently damaged and irreversible and once the patient begins the treatment, it can not be stopped. Therefore a patient leaving the treatment process
permanently and losing tracks from the enrollment registry records is hypothetically died. By incorporating this information, we can then calculate a patient’s survival time. Lastly, the choice feasibility is measured by two variables: the number of dialysis facilities and beds located within 10 km in a patient’s residing area.
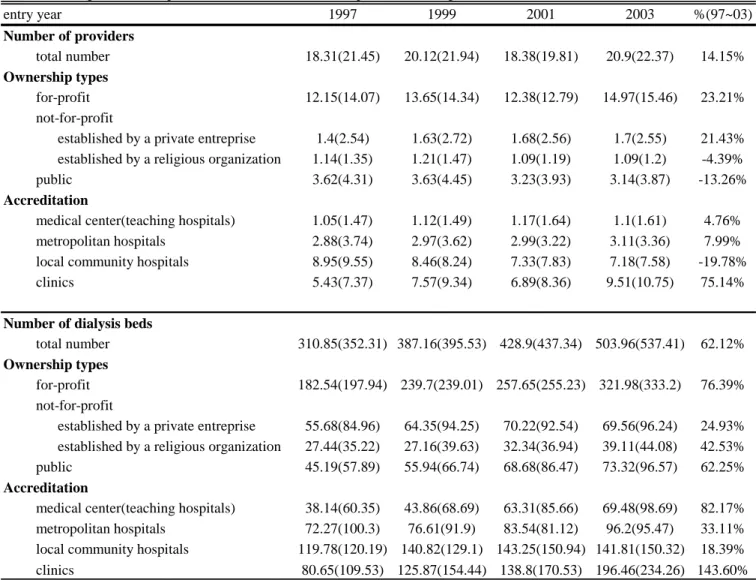
From our estimations, we found the following. First, a patient’s mortality is significantly lower when he has greater choice feasibilities. Specifically, when a patient resides in an area with one more dialysis facility, his mortality rate, on average, will be dropped by 0.4%. If the number of dialysis beds located nearby a patient’s residing area increases by 100 beds, his mortality rate will 1.78% lower. Second, patients do not gain from all choices of providers with different characteristics. Particularly, we found that a patient can
3
be better off when the number of incumbent dialysis facilities is higher. Third, providers with different ownership type have different impact on a patient’s survival. Specifically, only as the number of the public providers increases, a patient can then be better off. Lastly, we found that when an ESRD patient has more choice of large-scaled dialysis facilities, his mortality rate is significantly lower by 2.27%.
The main contribution of this paper is to add to the sparse literature providing empirical evidence as to the impact of the choice feasibility on a patient’s survival rate and the impact of a patient’s incentives on his survival rate. Secondly, it is long concerned in the existing literature that whether providers with different characteristics can benefit a patient or provide different health outcome. Though there are great amount of attention on this line of literature, these studies are usually subjected to the limitation of potential bias caused by the patient selection. Instead, this paper uses an exogenous variable, the number of providers located nearby a patient’s residing area, to investigate whether providers can affect a patient’s survival rate. This provides a better unbiased way for investigation of these impacts. We believe that our findings should be more robust. Lastly, we do find that providers with different
characteristics have different impact on a patient’s survival.
Our findings have important implications for both academic research and policy. For the research, our findings lead another further question - by what mechanism the choice
feasibility affect a patient’s survival?, and by what mechanism providers with different characteristics affect a patient’s survival? For the policy implication, our findings suggest that to enhance a patient’s choice feasibility can significantly increase an ESRD patient’s survival. Furthermore, the authority should encourage the establishment of dialysis facility especially for a market that there is initially only one provider.
The rest of this paper is organized in the following. We first describe the empirical models, and then introduce the data sets and the sample used for estimations. Descriptions of our basic Kaplan-Meier survival estimation results and Cox’s regression results are followed. Lastly, we discuss the results and then conclude our findings.
4
Estimation Methods
To examine the relationship between provider’s choice and treatment outcome, we estimate the survival function of end-stage hemodialysis patients using proportional hazard
model. Let h t x
; i be the hazard rates for patient i with characteristics x at time t, such that
; i 0
exp
ih t x h t x
(1)1 , 2 , ,
i i t i t i t i k t
x
nchoice
xpat
xaeaa
Z
(2)Equation (1) indicates that the hazard function is a multiple of the baseline hazard h t0
and
exp xi
, a patient’s relative hazard rate parameterized byx
i
. In equation(2),xpat
i t, is avariable vector capturing a patient’s personal characteristics, such as gender, age of onset, and
comorbidity16;
xarea
i t, contains characteristics of patient i’s residence, such the ratio ofelderly in the residing area;
Z
i captures all other influencing factors. In addition,
krepresents time-invariant unobservable factors of patient i’s residing area, and
t capturesthe time trend of the patient’s hazard rate.
The variable of interest,
nchoice
i t, , represents patient i’s feasibilities of choices ofhealth care providers. and is measured by the number of providers (and beds) located within 10 kilometers of the patient’s residing area. When a patient resides in an area with higher
level of
nchoice
i t, , s/he has more choices of health care providers. Therefore, if a patientreceives a better treatment quality when residing in an area with more choices of providers,
the estimated coefficient,
1, should be significantly negative.However, the above setup is subject to a selection bias. A severer patient may choose different type of providers for treatments. For example, in order to have better treatment, a
16
The existing literatures have confirmed that whether a patient is with diabetes has impact on a dialysis patient’s survival rate(USRDS, 1992; Churchill et al., 1996, Cheng and Young, 1999). Furthermore, the influence of hypertension on a dialysis patient’s survival is ambiguous. Some researches found that a dialysis patient has lower survival rate when s/he has comorbidity of
hypertension (Lin, 2002; Kuo, 1997). Some of them did not find this significant association (Zager et al., 1998; Salem, 1999; Port et al., 1999). In our estimation, we control patient’s clinic condition before his first treatment of hemodialysis, such as whether a patient is with diabetes, hypertension, or both.
5
severer patient may go to a teaching hospital, or a larger scale hospital for hemodialysis treatment. Furthermore, due to the financial incentive, different types of provider ownership may have different care quality. In order to reduce this potential bias, in equation (2), we add
a variable vector,
Z
i, for controlling characteristics of patient’s admitting provider, andrewrite the
Z
i
as following:
i h h
all h
Z
z
(3)where
z
h is the hth characteristic of a provider. We consider three categories of providercharacteristics. The first one is a provider’s ownership type including for-profit, not-for-profit, and public providers. As to the not-for-profit providers, since some of them in Taiwan are established by a private enterprise and some are by a religious organization. Though both are categorized as not-for-profit organizations, their financial incentive significantly differs. We therefore separate not-for-profit providers into two groups based on their sponsorship:
not-for-profit provider established by a private enterprise, and by a religious organization. The second category of provider characteristics we consider here is provider’s scale. We divide all
providers based on their bed size into three sizes: small(0bedsize15),
medium(15bedsize30), and large(bedsize30). The third category is provider
accreditation including teaching hospitals, metropolitan hospitals, local community hospitals, or dialysis centers.
Data, Variables, and Sample
Data sources
Three sets of information are needed for estimation: (1) patient information, including gender, age, comorbidity, and most importantly, their residing areas and death information; (2) characteristics of patient’s first admitted provider, including ownership types, bed sizes, and teaching status; and (3) number of providers in an area. For obtaining all of these information, we use four data sources obtained from Taiwan’ National Health Insurance Research Database
6
(NHIRD) maintained by National Health Research Institute. NHIRD contains all these information and all sub-files in NHIRD use the same patient ID, hospital ID, and area zip-code. These IDs enable us to link information of patients, providers, and areas from other sources. Furthermore, kidney failure is one of catastrophic illnesses announced by Taiwan’s
Department of Health17. Patients with kidney failure can apply for a catastrophic illness card
issued by Bureau of National Health Insurance. With this certificate, a patient can go for treatment without copayments. This assures us that income does not play an important role in a patient’s treatment decision. Therefore, we use the following four datasets in NHIRD from year 1996-2003.
The first is the longitudinal outpatient claims of NHI enrollees suffering catastrophic illnesses from 1996-2003, Ambulatory Care Expenditures by Visits for Catastrophic Illness
Patients (HV-CD)18. Because NHI covers almost the entire population, and kidney failure is
officially categorized as one of catastrophic illnesses, we essentially have every kidney failure case in Taiwan. These claims record diagnoses of diseases, detailed description of medical expenses, and most importantly the date for all visits of treatment. Therefore, by appending all year HV-CD data, we can trace patients’ first and last date of hemodialysis treatment. Most importantly, by combining a patient’s registry record, this provides us a strategy to identify a patient’s mortality information, which will be discussed in detail later.
The second source combines two different NHRID health provider datasets spanning from 1996-2003. Specifically, we use Registry for Contracted Medical Facilities (HOSB) and Registry for Contracted Beds (BED). From these two datasets, we obtain a health provider’s
location, accreditation19, ownership20, teaching status (for hospitals), and its number of
17
Initially, a kidney failure patient can be issued a catastrophic illness card if (1) s/he is a chronic renal failure patient, and (2) s/he has to obtain certificates from at least two nephrologists who has diagnosed and assert this patient’s renal failure condition. However, after April first of 2001, Taiwan health authority relaxed this regulation. A kidney failure patient can be issued a catastrophic illness card if s/he is diagnosed by only one nephrologist. Furthermore, patients can obtain a three-month temporary certificate of catastrophic illness if doctors are not sure whether the patient’s renal failure condition is irreversible.
18
There are 30 catastrophic illnesses in Taiwan that are announced by Department of Health. 19
There are four levels of provider accreditation: medical centers, metropolitan hospitals, local community hospitals and private clinics.
20
7
dialysis beds. Furthermore, we merge the provider’s location with a file containing the latitude and longitude of each zip-code in Taiwan. This enables us to calculate the distances among areas, and number of providers (and beds) located within certain distance for an area.
The third source is the Registry for Beneficiaries which is the eligibility file of all NHI enrollees covering between 1996 and 2003. This dataset contains all enrollee’s scramble ID, basic demographics (gender and age), group of enrollment, and zip-code of enrollment location. With the unique patient ID, we can merge a patient’s characteristics with the above claim data (HV-CD). Besides, the merged data can then merge with provider information using the unique hospital ID and we can then obtain the characteristics of the patient’s first admitted provider. Furthermore, with the help of zip-code information, we can calculate the number of providers (and beds) located within certain distance in a patients’ residing location.
The final analytic dataset is a longitudinal data with a format that each observation contains a patient’s monthly record. The entire observation periods range from January 1st, 1997 to December 31st, 2003. Though NHIRD spans from 1996 to 2004, we do not use all periods of data collected in NHIRD for the following reasons. Firstly, in order to identify a patient’s first treatment date, we exclude patients whose first visit record in NHIRD is in 1996. Secondly, from those patients starting their first dialysis in 2004, the observation period is too short. We then focus on a patient whose first treatment year is before 2004. Lastly, in order to identify a patient’s mortality status, we define December 31st of 2003 as our last date of observation. Since then we can define a patient is still alive if her/his last treatment date is before or after December 31st of 2003. Therefore, the entire period under observation is from January 1st , 1997 to December 31st, 2003.
Variable measures
Before introducing our analytic sample, we first classify two important measures:
providers. However, in Taiwan, some of not-for-profit hospitals are established by private enterprises, and some are by religious organizations. It is believed in Taiwan that these two types of not-for-profit hospitals have significantly different financial incentives. We therefore separate not-for-profit hospitals into two groups: a private enterprise established and a religious organization established not-for-profit provider.
8
mortality and choice feasibility. Because we do not directly observe a patient’s death record, we use the following strategies to identify a patient’s death information. Firstly, because chronic renal disease is irreversible and dialysis treatments can not be stopped, an ESRD patient losing traces from our claim records hypothetically is either dead or gets his kidney transplanted. Secondly, in order to exclude the cases of kidney transplantations, we
incorporate a patient’s insurance enrollment information from the file of Registry of
Beneficiary. A kidney transplanted ESRD patient’s record of enrollment can still be found as long as this patient is still alive and in Taiwan. Thirdly, we therefore identify whether an ESRD patient is dead after treatment if we lose trace of this patients from both sets of
datasets21. Because we can identify a patient’s death information, and HV-CD dataset records
all visits of dialysis treatment, with a patient’s first and last date of treatment, we can calculate his survival day.
As to the variable of choice feasibility, two measures are used. The first one is the number of dialysis facilities located within 10 kilometers in a patient’s residing area. This measure treats all size facilities equal and may bias our estimations. We therefore improve this measure by defining our second measure of the choice feasibility as the number of dialysis beds located within 10 kilometers in a patient’s residing area.
Sample
The patients under observation are those with end-stage renal disease (ESRD), a disease that refers to permanent damage to the kidneys that result in loss of normal kidney function. Generally speaking, these patients have to continuously receive dialysis treatments at least for three months, and must be chronic irreversible renal failure. When someone is diagnosed as an ESRD patient, there are three types of treatments: hemodialysis, peritoneal dialysis, and kidney transplantation. Because most of ESRD patients in Taiwan use hemodialysis therapy (around 92.3%, see Huang et al.(2007)), this study emphasizes on ESRD patients with
21
Hypothetically, patients losing tracks from our records may immigrant to foreign countries.
However, according to the statistics of Taiwan’s Ministry of the Interior, the percentage of immigration to countries outside of Taiwan is less than 0.3% from 1997-2006(MOI, 2008).
9
hemodialysis treatments. Lastly, in order to investigating patients’ survival, we focus on new ESRD patients after 1996. The method of identification of new hemodialysis ESRD patients
we employ is as Sheu and Lien (2007)22.
Though HV-CD contains claim records for almost all ESRD patients, about 60% of the sample is dropped to ascertain a patient’s residence information. The file of Registry for Beneficiaries records information on the zip-code of enrollment; however, there are several difficulties for applying them directly. Firstly, the zip-code of enrollment indicates the
location from which an enrollee obtains his coverage. This location may not be the same with his household registry. Especially for those elderly whose coverage is usually paid by their other family members that are not live with them. Secondly, even for enrollees whose
residences are identical to household registry, a substantial portion of them actually choose to
live at places different than their household registry23. We therefore use the following
strategies to ascertain a patient’s residence information. Firstly, we choose enrollees of two enrollment groups: obtaining coverage from office of household registry and farmer associations. Secondly, we exclude patients who have to travel more than 5 kilometers for their hemodialysis treatments. By using these two criteria of sample selection, the final number of patients under observations dramatically drops. As table 1 have shown, one can find that around 65% of ESRD patients were dropped due to the patient selection criteria. However, the percentage is slightly decreased from 66% in 1997 to 60% in 2003.
The dramatic drop on the number of patients under observation may cause our analysis problematic due to potential sample selection issues. In order to make sure that patients used in our analysis are representative, table 2 provides comparisons of basic patient characteristics between whole ESRD patients and samples selected by our criteria. One can see that patients
22
According to Sheu and Lien(2007), HV-CD provides two variables for identify hemodialysis patients. However, more than 40% of this information is missing. This restricts researchers to use this piece of information directly. However, since ESRD is one of catastrophic illnesses, patients can get treated without any costs. Furthermore, the amounts of reimbursement for both peritoneal dialysis and hemodialysis are flat in a fixed level at $4100 and $6940 for hemodialysis and peritoneal dialysis respectively before June 1st of 2004. We can then use the total amount of treatment claimed by a provider to identify whether an ESRD patient is treated by hemodialysis or peritoneal dialysis. 23
10
in our analytic tend to be older than those in the whole sample. In addition, the comorbidity condition prior to their first hemodialysis treatment is relatively severer. However, the difference is not significant.
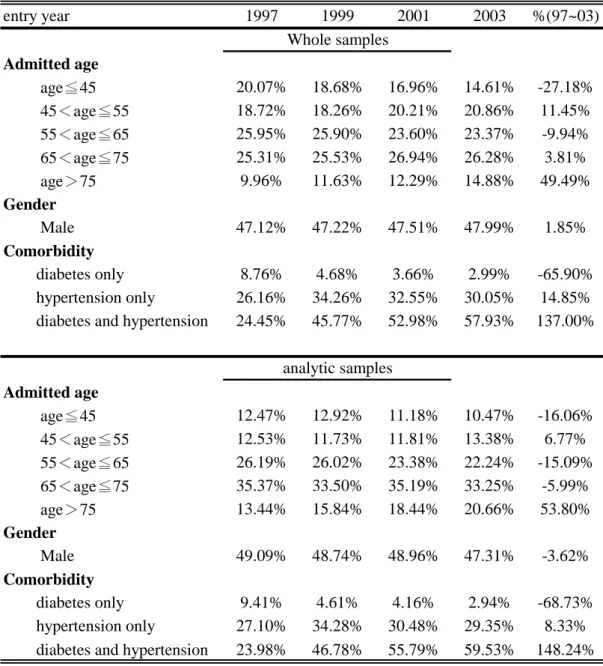
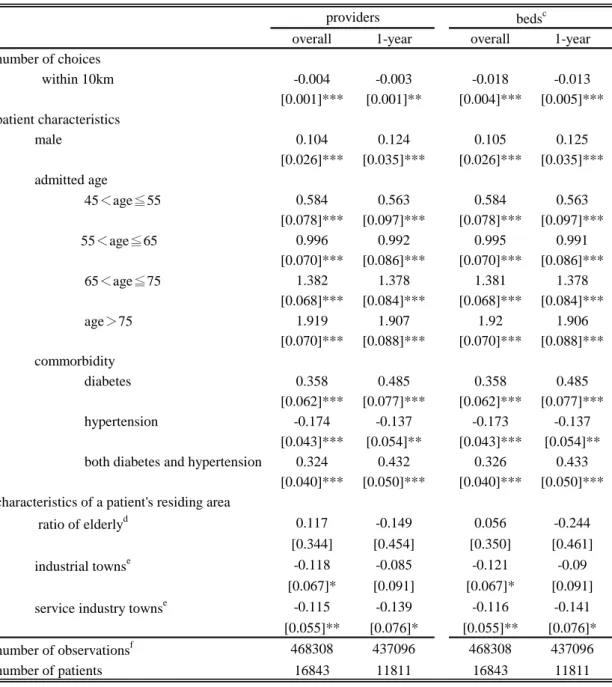
We then turn to introduce the sample used in our analysis. From the lower panel of table 2, generally speaking, the ratio of male new patients is around 49% and is relatively stable for the pattern in the long run. However, the health conditions of patients seem to be getting worse. Not only do the ratios of patients with hypertension or both hypertension and diabetes increases (from 24.45% in 1997 to 57.93% in 2003), but also the ratio of older patients (age>75) rises from 9.96% in 1997 to 14.88% in 2003 (49.69% increased). Actually the average age of a patient’s first treatment increases from 62.37 to 64.39 over these 7 years.
As to a patients’ first admitted provider, most of them are admitted initially in a for profit medical institution, though this ratio slightly decreases from 50.23% in 1997 to 47.53% in 2003. Around one fifth of new patents were first admitted in a not-for-profit provider established by a private enterprise. If we count both for-profit and private enterprise
established not-for providers, around 70% of patients go for their first hemodialysis treatment in a “private” medical facility. One-fifth of patients are admitted initially in a public provider, and rest of patients is in a religious organization established not-for-profit provider. However, the ratio of patients first admitted in this type of facilities significantly increases from 11.51% in 1997 to 14.53% in 2003 (increased 26.26%). This may reflects the possible quality
difference for providers with different types of ownership.
Most of new patients are initially admitted in either a metropolitan or local community hospital. However, the ratio admitted in local community hospitals significantly dropped from 40.87% in 1997 to 29.52% in 2003 (27.77% dropped). This is probably due to the closure of local community hospitals in Taiwan over this decade. On other interesting point is that though less than 20% of new patients go for their first hemodialysis treatment in a private clinic, however, its ratio actually increased around 30% (15.14% in 1997 to 19.67% in 2003). This indicates private clinics are getting playing an important role in the industry and the high profitability in this industry. Another phenomenon is that new patients are more likely to go
11
for their first treatment in a larger scale provider. One can find from table 3 as well that the ratio of patients who go for a provider with more than 15 beds increases significantly over these 7 years. The above significantly differences on characteristics of a patient’s first admitted provider indicate that there may exists a provider selection problem. This suggests us to control for those related characteristics of a patient’s first admitted provider when estimating the survival rates.
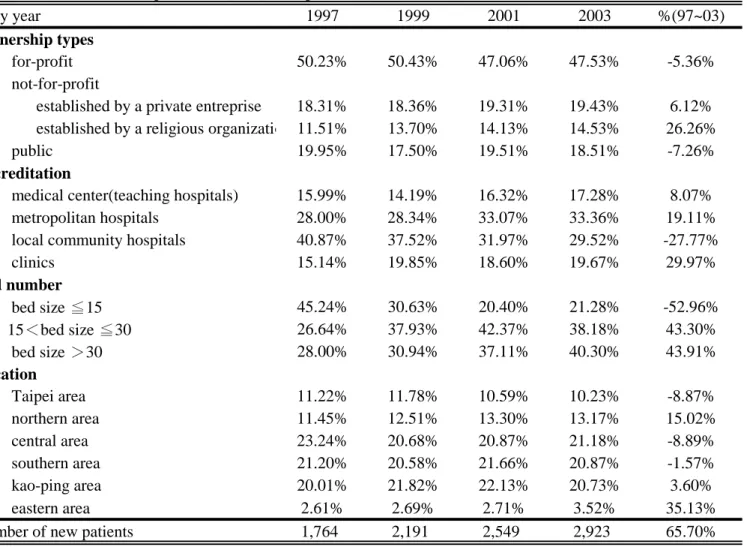
The average number of dialysis facilities within 10 km in a patient’s residing area slightly increases over observational periods as shown in the table 4. On average, there are around 20 providers located within 10 km in a patient’s residing area. This indicates on average, over these periods, an ESRD patient has more choice when seeking hemodialysis treatment. From the top panel of table 4, we also notice that there is a drop on number of provider within 10 km in a patient’s residing area in 2001. This may be due to the implementation of global budgeting in Taiwan starting from 2001. However, this figure increases to 20.9 in 2003 again. This suggests us for controls of time period dummies when estimating a patient’s survival. If we separate these providers by their ownership types, most of them are for profit (around 60%). During these periods, the number of for profit dialysis centers increases from 12.15 in 1997 to 14.97 in 2003 (23.21% increases). A similar growth rate of number of providers can be found in the ownership type of not-for-profit that is
established by a private enterprise. This may be due to the high profitability in this industry so that it attracts “for-profit” type firms to enter the market. A similar phenomenon can be found if we separate providers by their accreditation. From the last row of top panel of table 4, during these observational periods, most of patients’ choice is of local community hospitals or private clinics. However, over these periods, the average number significantly decreases for local community hospitals and increases for private clinics. This is probably due to the closures of local community hospitals in Taiwan in recent decade.
Though we observe a diversified pattern on the average number of providers, we do observe a consistent pattern on the average number of dialysis beds within 10 km in a patient’s residing area. One can find from the lower panel of table 4 that from 1997 to 2003,
12
the average number of beds located in a patient’s residing area significantly increases (around 62%). In addition, this increasing pattern can be found if we separating providers by their ownership type or accreditations. The different pattern shown in these two panels suggests us to use two different measures for a patient’s choice feasibilities.
Results
Basic results - Kaplan-Meier survival estimates
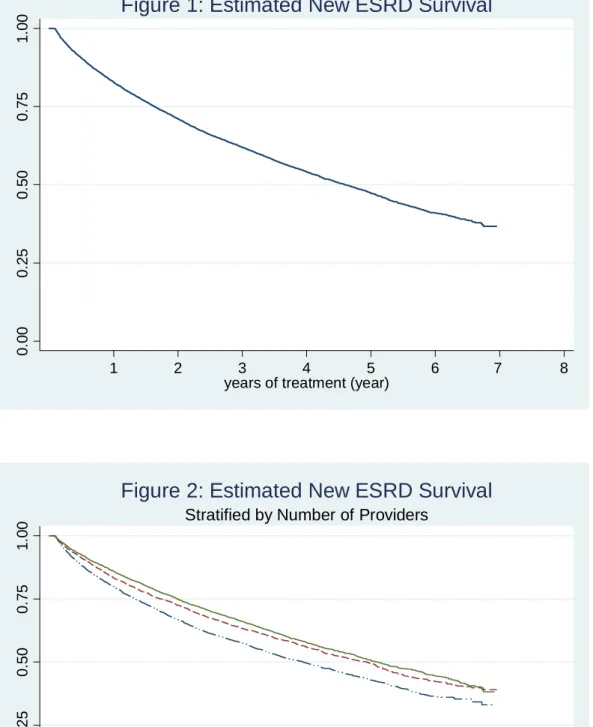
We first present the overall Kaplan-Meier survival estimates in figure 1. The estimated survival curve declines dramatically in the very beginning, and then become flatter as the survival year increases. This indicates that a patient’s mortality rates increases in a diminishing rate and is consistent with existing clinic studies showing that the first year survival rate is dropped by 2~15% (DeOreo, 1997; Lin, 2002). From our estimation, the first year mortality rate is around 17.17%, and rises in a diminishing rate as the survival year increases. Around 71% of patients can survive for more than one year, however, their chance to survive shrinks to be half-half conditional on patients have been receiving 4.6 years of treatment.
Figure 2 estimates the overall Kaplan-Meier survival rates for three groups of patients residing in areas with different choice feasibility measured by the number of providers located 10 km in a patient’s residing area. We classify a patient as one with scarce choice feasibilities if he has less than seven providers located nearby, modest choice feasibilities if the number of providers nearby his residing area is between 7 and 24, and numerous choice feasibilities if
the number is more than 2424.. From the estimation shown in figure 2, three observational
points can be addressed. Firstly, overall speaking, the shapes of these three survival curves are similar with that in figure 1, indicating no matter how many choices of providers one has, its mortality is increasing in a diminishing rate. Secondly, a patient with more choices on providers does have better outcome. From our estimations, the survival rate conditional on
24
The dividing points are based on the first and third quantile of the number of providers within 10 km.
13
receiving one year treatment is 85.91% for a patient with numerous choice feasibilities, which is 3.1% higher than that for a patient with modest choice feasibilities. The survival rate conditional on receiving one year treatment is 79.91% which is 4.3% lower than that for a patient with modest choice feasibilities. Lastly, the difference of survival rates among these three groups of patients is getting larger when the years of treatment received increase. This indicates that the impact of choice feasibilities on a patient’s health outcome may be
significant in a long run. Actually, a log-rank test(Mentel and Haenszel, 1959) is performed25,
and the
X
2(
df
2)
value is equal to 90.77 (p values
<0.01) which is significant under thetraditional significance level26.
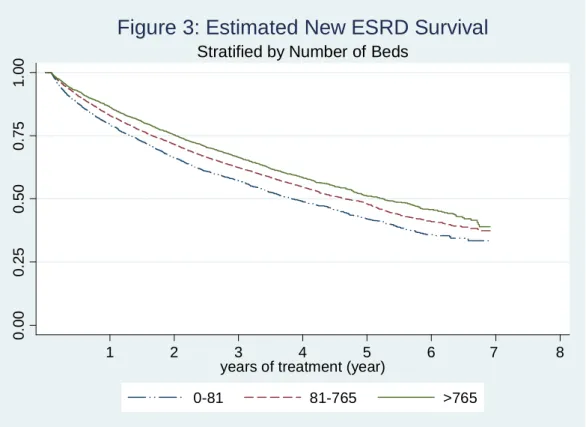
The above estimations use the number of dialysis providers, both hospitals and clinics, as the measure of a patient’s choice feasibility. This measurement treats all providers equal regardless the scale of a dialysis facility. We therefore turn to estimate the Kaplan-Meier survival rates based on the total number of dialysis beds within 10 KM in a patient’s residing area. Results are presented in figure 3. One can find that as the number of beds increase, a patient’s survival rate increases as well, which are consistent with those we found in figure 2.
The log-rank test shows the
X
2(
df
2)
value is equal to 75.58 (p values
<0.01)27. Itindicates that the survival rates for a patient’s health outcome is better when he resides in an area with more choice feasibilities measured by the number of dialysis beds located nearby
Regression estimations - Cox’s hazard model
The above Kaplan-Meier survival estimates based on different measure of choice feasibilities find that a patient with more choices is better off in his health outcome. However, these estimations do not control for many other risk factors that will affect a patient’s survival,
25
The null hypothesis is H0:h t1
h t2
h t3
, where h ti
the is the hazard function for patients in group i.26
We also perform other tests that are mostly used in tests of hypothesis under survival analysis including Wilcoxon test(Breslow, 1970; Gehan, 1965), Tarone-Ware test (Tarone and Ware, 1977), and the Peto-Peto-Prentice test(Peto and Peto, 1972; Prentice, 1978). All of these tests shows the same results with that obtained by using log-rank test.
27
The Wilcoxon test, Tarone-Ware test, and the Peto-Peto-Prentice test are performed as well. All tests provide us the same restuls.