P
Puurrppoossee.. The aim of this study was to use the scored storage symptoms questionnaire to screen urodynamic stress incontinence (USI) in women with overactive bladder (OAB).
M
Meetthhooddss.. We randomly enrolled 238 women with OAB. Scored storage symptoms questionnaire scores (SSQS) were incorporated as part of independent history at the first consultation. The scores of each patient were analyzed and correlated with the gynecologist's clinical diagnosis, which was based on urodynamic findings.
R
Reessuullttss..Subjects with USI had significantly higher urge incontinence scores, leakage amount scores, stress incontinence scores, and total scores than those without USI. The risk of USI increased with the severity of stress incontinence symptoms. By defining total scores over 12 and stress incontinence scores over 2 as the cut-off points for USI, we found that the SSQS had a sensitivity of 82%, a specificity of 85%, a positive predictive value (PPV) of 79%, a negative predictive value (NPV) of 87%, and an accuracy of 84%. To test the sensitivity of the SSQS to predict clinically important changes, the SSQS of 20 successfully treated patients were compared before and 6 months after surgical treatment of USI. There were significant decreases in values of all six parameters (frequency, nocturia, urgency, urge incontinence, leakage amount, and stress incontinence) and total scores.
C
Coonncclluussiioonnss. The scored storage symptoms questionaire is of value in determining changes in the storage symptoms of the lower urinary tract, and is a sensitive method for predicting USI. ( Mid Taiwan J Med 2006;11:222-9 )
K
Keeyy wwoorrddss
overactive bladder, storage symptoms of lower urinary tract, storage symptoms questionnaire score, urodynamic stress incontinence
IINNTTRROODDUUCCTTIIOONN
Storage symptoms of the lower urinary tract (eg frequency, urgency, urinary incontinence) are commonly encountered in both sexes and all ages. Overactive bladder (OAB) is a chronic, debilitating syndrome defined by the International Continence Society as urgency, with or without
urge incontinence, usually with frequency and nocturia, that can not be explained by metabolic (eg diabetes) or local pathological factors (eg urinary tract infection, stones, interstitial cystitis) [1].
Stress urinary incontinence (SUI) is a lower urinary tract symptom [2]. Up to 20% of women with OAB symptoms had a urodynamic diagnosis of urodynamic stress incontinence (USI) [3].
However, as many as 75% of women OAB and SUI had USI [2]. Lower urinary tract storage
Received : 13 June 2006. Revised : 3 July 2006.
Accepted : 27 September 2006.
Address reprint requests to : Wei-Chun Chang, Department of Obstetrics and Gynecology, China Medical University Hospital, 2 Yuh-Der Road, Taichung 404, Taiwan.
A Scored Storage Symptoms Questionnaire to Screen Urodynamic Stress Incontinence
in Women with Overactive Bladder
Huey-Yi Chen1,2, Yao-Ching Hung1,3, Tung-Chuan Yang1,2, Lian-Shung Yeh1,3, Wei-Chun Chang1,3
1Department of Obstetrics and Gynecology, China Medical University Hospital; 2School of Chinese Medicine,
3School of Medicine, China Medical University, Taichung, Taiwan.
symptoms (eg OAB, SUI, OAB SUI ) are not disease specific, and it is unclear whether invasive urodynamic assessment is mandatory to determine the etiology and treatment modality.
Although there are a plethora of questionnaires for evaluating urinary incontinence, only one study has attempted to differentiate between USI and OAB [4]. The questionnaire by Kauppila et al [5] is long and difficult to use. Therefore, there is a need for a concise, easy-to-use questionnaire, which can distinguish the two diseases. We propose the scored storage symptoms questionnaire modified from the questionnaire by Kauppila et al. To our knowledge, no other study has scientifically evaluated SUI in women with OAB by a scored storage symptoms questionnaire. An exploration of the scored storage symptoms questionnaire in the evaluation of SUI in women with OAB was therefore thought to be of importance. In this respect, the purpose of this study was to use the scored storage symptoms questionnaire to screen urodynamic stress incontinence in women with overactive bladder.
M
MAATTEERRIIAALLSS AANNDD MMEETTHHOODDSS Subjects
We randomly enrolled 238 subjects (age range, 23 to 78 yr) (mean, 51.1 10.8 yr) with OAB who presented for urogynecological consultation in our department. The random
samples were generated by computer. The exclusion of subjects with specific diseases such as diabetes mellitus, urinary tract infection, stones, interstitial cystitis, or pelvic organ prolapse was made on the basis of medical history, physical examination, or laboratory findings.
Investigations
The patients first consulted a specialized nurse for history taking and preliminary tests. The scored storage symptoms questionnaire shown in Table 1 was incorporated as part of independent history at the first consultation. After consenting to the study, the subjects self-administered the questionnaire and were instructed to mark any questions they found confusing or difficult to answer. The specialized nurse then debriefed the patient about the questionnaire and about marked questions in particular. Patient descriptions of problems with questions were recorded verbatim.
The identical questionnaire was then administered by mail approximately 1 week after the initial administration to examine short-term test-retest reliability. The resulting score was not calculated until the study was over, thus blinding the gynecologist. The specialized nurse also had no knowledge of the scored storage symptoms questionnaire results. Urine samples were examined, and cultured if infected. The patients filled in frequency/volume-charts so that the results could be presented to the gynecologist at the next consultation.
Table 1. Items in the scored storage symptoms questionnaire
Item reponses of question 1 are assigned values of 0 for "1 to 8 times a day", 1 for "9 times a day", 2 for "10 times a day", 3 for "11 times a day", 4 for "12 times a day", and 5 for "13 or more times a day". Item reponses of question 2 are assigned values of 0 for "0 to 1 time", 1 for "2 times", 2 for "3 times", 3 for "4 times", 4 for "5 times", and 5 for "6 or more times". Item reponses of question 3 and 4 are assigned values of 0 for "not at all", 1 for "less than 1 time in 5", 2 for "less than half the time", 3 for "about half the time", 4 for "more than half the time", and 5 for "almost always". Item reponses of question 5 and 6 are assigned values of 0 for "not at all", 1 for "very slight amount", 2 for "slight amount", 3 for "moderate amount", 4 for "severe amount", and 5 for "very severe amount".
During the last six months or so:
Question 1. How many times did you urinate during the day?
Question 2. How many times did you typically get up to urinate from the time you went to bed at night until the time you got up in the morning?
Question 3. How often have you felt a strong need to urinate with little or no warning?
Question 4. How often have you been unable to get to the bathroom in time to urinate?
Question 5. How much urinary leakage have you felt with each episode of incontinence?
Question 6. How much urinary leakage have you felt during physical activity eg coughing, sneezing, lifting etc?
The gynecologist's consultation consisted of detailed history taking, physical examination including pelvic and rectal examination, urethracystoscopic examinations for stones or interstitial cystitis, evaluating data from multi-channel urodynamic studies including uroflowmetry, filling and voiding cystometry, and stress urethral pressure profile, and 20-minute pad test. The scored storage symptoms questionnaire results were unknown to the gynecologist. The gynecologist recorded two sets of diagnoses for our scientific purpose; a urodynamic diagnosis and a clinical diagnosis after a comprehensive assessment of all available data except for the scored storage symptoms questionnaire.
Urodynamic assessments
Urodynamic assessment was carried out according to the method described by Lin et al [6]. Storage dysfunction (SD) and voiding dysfunction (VD) were defined according to Lin et al [6]. The types of urinary incontinence are classified as idiopathic detrusor overactivity (IDO), USI, or mixed USI/IDO according to the International Continence Society (ICS) [7]. A Dantec six-channel urodynamic monitor with computer analysis (Menuet, Tonsbakken,
Skovlunde, Denmark) was used in this study. All procedures were performed by an experienced technician, and the data were interpreted by one observer to avoid bias.
Statistical analysis
Variables among subjects with and without USI were compared by the Mann-Whitney test.
Time 1-Time 2 test-retest reliabilities were examined for individual questions and total scores. These associations were examined by calculating Pearson's product-moment correlation coefficients. Correlations of 20-minute pad tests and SSQS were analyzed by analysis of variance.
A multivariate logistic regression model and odds ratios (OR) (with 95% confidence intervals (CI)) were used to assess the independent prognostic value of the scored storage symptoms questionnaire variables for predicting USI.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were defined according to the values used by Sackett et al [8]. These measures were calculated using the gynecologist's clinical diagnosis, which was based on urodynamic findings, as the standard. Receiver operation characteristic (ROC) curves were drawn
Table 3. Storage symptoms questionnaire scores in subjects with and without urodynamic stress incontinence
Values are mean SD, statistical analysis by Mann-Whitney test. *Total score is sum of questions 1 to 6.
1-frequency 2-nocturia 3-urgency
4-urge incontinence 5-leakage amount 6-stress incontinence Total score*
2.18 1.13 1.99 1.07 1.43 1.10 0.95 1.20 1.28 1.00 1.36 0.96 9.19 4.12
Urodynamic stress incontinence Negative
(n = 137)
Positive (n = 101) Question p
2.20 0.80 2.13 0.98 1.52 0.82 1.21 1.02 2.76 0.84 3.08 0.81 12.88 3.19
0.610 0.275 0.117 0.007
< 0.001
< 0.001
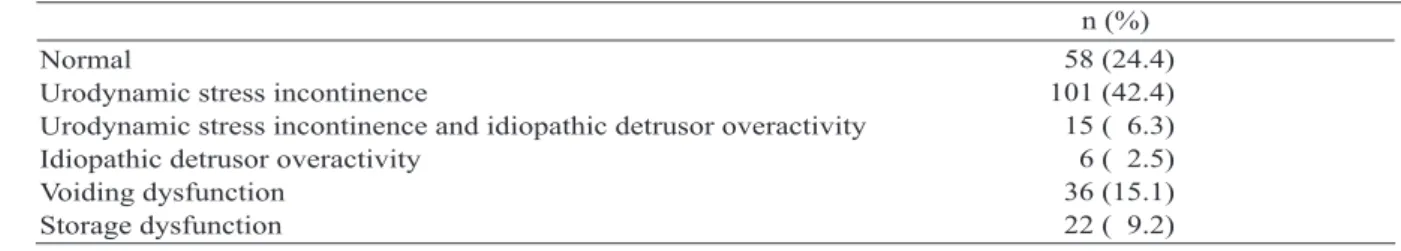
< 0.001 Table 2. Diagnoses in 238 women with storage symptoms of lower urinary tract
Normal
Urodynamic stress incontinence
Urodynamic stress incontinence and idiopathic detrusor overactivity Idiopathic detrusor overactivity
Voiding dysfunction Storage dysfunction
n (%) 58 (24.4) 101 (42.4) 15 ( 6.3) 6 ( 2.5) 36 (15.1) 22 ( 9.2)
according to the procedure described by Sackett et al [8]. The Wilcoxon signed-rank test was used for comparisons of variables in successfully treated subjects before and after treatment. All statistical tests were two-sided. A p value less than 0.05 was considered statistically significant.
The data were analyzed by the Statistical Package for Social Sciences (SPSS for Windows, release 8.0, SPSS Inc, Chicago, IL, USA).
R
REESSUULLTTSS
The final diagnoses after clinical and urodynamic investigations are presented in Table 2. Figure 1 depicts the distribution of the storage symptoms questionnaire scores (SSQS) among 238 women with or without USI. SSQS in subjects with and without USI are provided in Table 3. Subjects with USI had significantly higher urge incontinence socres, leakage amount scores, stress incontinence scores, and total scores than those without USI.
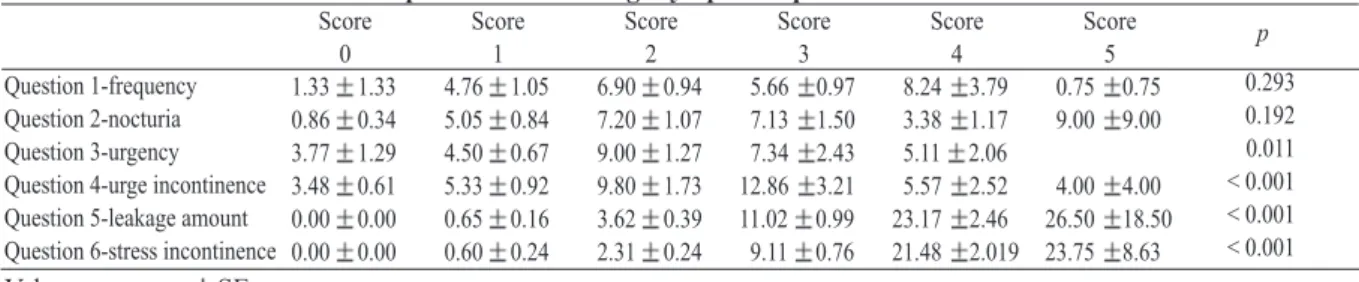
A total of 204 of 238 subjects returned the Time-2 questionnaire for the assessment test- retest reliability (86%). Table 4 gives the Pearson's correlation coefficients comparing Time 1 and Time 2 responses for each retained question
and total score. Only the questions on frequency and urgency showed much instability (r = 0.60 and 0.58, respectively). However, the test-retest correlation of the total score was excellent (r = 0.89).The correlation between 20-minute pad tests and SSQS is provided in Table 5. The scoring groups of questions about urgency, urge incontinence, leakage amount, and stress incontinence differed significantly in 20-minute pad tests. Table 6 summarizes odds ratios with 95% confidence intervals for USI of scored storage symptom questionnaire variables after multivariate logistic regression analysis. The risk of USI increased with the severity of stress incontinence symptoms (OR = 11.82, 95% CI = 4.82 to 28.94).
Figure 2 shows the cut-off points for total scores and stress incontinence scores on the ROC curves. The optimum cut-off points (inflation points) were > 12 for total scores and > 2 for stress incontinence scores. The diagnostic
Table 4. Test-retest reliability of individual symptom questions and total scores
*Total score is sum of questions 1 to 6.
1-frequency 2-nocturia 3-urgency
4-urge incontinence 5-leakage amount 6-stress incontinence Total score*
0.60 0.71 0.58 0.79 0.81 0.82 0.89 r Question
Fig. 1. Distribution of the storage symptoms questionnaire scores among 238 women with and without urodynamic stress incontinence (USI).
Table 5. Correlation of 20-minute pad tests and storage symptoms questionnaire scores
Values are mean SE.
Question 1-frequency Question 2-nocturia Question 3-urgency Question 4-urge incontinence Question 5-leakage amount Question 6-stress incontinence
1.33 1.33 0.86 0.34 3.77 1.29 3.48 0.61 0.00 0.00 0.00 0.00 Score
0
4.76 1.05 5.05 0.84 4.50 0.67 5.33 0.92 0.65 0.16 0.60 0.24 Score
1
6.90 0.94 7.20 1.07 9.00 1.27 9.80 1.73 3.62 0.39 2.31 0.24 Score
2
5.66 0.97 7.13 1.50 7.34 2.43 12.86 3.21 11.02 0.99 9.11 0.76 Score
3
8.24 3.79 3.38 1.17 5.11 2.06 5.57 2.52 23.17 2.46 21.48 2.019
Score 4
0.75 0.75 9.00 9.00
4.00 4.00 26.50 18.50 23.75 8.63
Score 5
0.293 0.192 0.011
< 0.001
< 0.001
< 0.001 p
sensitivity, specificity, predictive values and accuracy for USI when total scores exceeded 12, when stress incontinence scores exceeded 2, as well as the two scores combined are presented in Table 7. By defining total scores over 12 and stress incontinence scores over 2 as the cut-off points for USI, we found that the SSQS had a sensitivity of 82%, a specificity of 85%, a positive predictive value (PPV) of 79%, a negative predictive value (NPV) of 87%, and an accuracy of 84%. To test the sensitivity of the
SSQS to predict clinically important changes, the SSQS of 20 successfully treated patients were compared before and 6 months after surgical treatment of USI (Table 8). There were significant decreases in values of all six parameters (frequency, nocturia, urgency, urge incontinence, leakage amount, and stress incontinence) and total score in the scored storage symptoms questionnaire. The largest decreases were for nocturia, leakage amount, stress incontinence and total score (p < 0.001).
Table 6. Odds ratios with 95% confidence intervals for urodynamic stress incontinence of storage symptoms questionnaire variables after multivariate logistic regression analysis
*p < 0.001. OR = odds ratio; 95% CI = 95% confidence interval.
Frequency Nocturia Urgency
Urge incontinence Leakage amount Stress incontinence
0.74 (0.40-1.37) 1.43 (0.84-2.42) 0.95 (0.40-1.06) 0.65 (0.40-1.06) 0.95 (0.44-2.06) 11.82 (4.82-28.94)*
OR (95% CI)
Table 7. Diagnostic sensitivity, specificity, predictive values and accuracy for urodynamic stress incontinence when total score > 12 and/or stress incontinence score > 2
PPV = positive predictive value; NPV = negative predictive value.
Sensitivity, % Specificity, % PPV, % NPV, % Accuracy, %
55 84 72 72 72 Total score > 12
77 94 91 85 87
Stress incontinence score > 2
82 85 79 87 84
Total score > 12 and stress incontinence score > 2
Fig. 2. Diagram of cut-off points. A: Total scores. B: Stress incontinence scores shown in receiver operation characteristic (ROC) curve analysis.
A B
D
DIISSCCUUSSSSIIOONN
Our findings show that using combined total scores over 12 for USI and stress incontinence scores over 2 as the cut off points yields an accuracy of 84%. For some purposes, diagnosing USI could perhaps be done even more simply by just asking if the woman experiences involuntary loss of urine when coughing or sneezing, without accompanying urge symptoms [9]. However, we found that this method of assessment only yielded an accuracy of 49%
(45/91).
Our results indicate that the SSQS is a reliable and valid means of evaluating the severity of USI symptoms; furthermore, the results show that the score generated from the SSQS is sensitive to clinically important time-dependent changes within individual patients. These features are all desirable in a questionnaire designed for discriminative, predictive or evaluative purposes [10]. Unlike previously published symptom scores, such as the detrusor instability score [5], the SSQS has been designed for self- administration in a uniform manner and has been validated in that mode of administration. The SSQS (accuracy: 84%) has higher face validity because it includes more conceptual symptoms that are seen as closely related to USI by clinicians (accuracy: 49%), and is therefore a more appropriate clinical tool than the incontinence impact questionnaire and the urogenital distress inventory developed for clinical and research application [11].
The lack of comparability in outcome measurements has been a problem in interpreting clinical research on USI for use in clinical
practice. As a partial solution to this problem, we propose that 6 questions in the SSQS be included in the protocols of prospective studies of the natural history and epidemiology of USI, and that the SSQS be reported when results of treatment are described. Investigators are encouraged to include other symptom questions that they believe are important as well, but the inclusion of this basic question set will provide an unparalleled opportunity to compare results among studies.
The measurement of USI symptoms is only one facet of the evaluaction of the natural history and the response to treatment of USI, albeit an extremely important one from the patient's perspective. Investigators will want to study other parameters, including physiological measures and ratings of patient quality of life, to obtain a complete picture of disease progression or treatment effectiveness. In addition, the measurement of rates of important outcome events, such as sexual dysfunction and incontinence, are also needed. Finally, important treatment complications, such as acute urinary retention and voiding dysfuction, should be described.
Although we have tried to develop the best symptom score possible for storage symptoms of the lower urinary tract, future improvements are warrented. We are currently evaluating the SSQS among patients from a spectrum of educational, cultural and socioeconomic backgrounds. We suspect minor wording changes may eventually make the SSQS more adaptable to the broadest possible population of urological patients.
We hope that the evaluation strategy we have outlined will serve as a model to evaluate future
Table 8. Preoperative and postoperative storage symptoms questionnaire scores in successfully treated subjects
Values are mean SD.
1-frequency 2-nocturia 3-urgency
4-urge incontinence 5-leakage amount 6-stress incontinence Total score
2.35 0.81 2.35 0.99 1.85 0.88 1.35 1.18 3.30 0.80 3.50 0.89 14.70 3.54
1.40 0.75 0.95 0.60 0.70 0.66 0.15 0.37 0.10 0.31 0.15 0.37 3.35 1.79
0.001
< 0.001 0.001 0.001
< 0.001
< 0.001
< 0.001 Preoperative
(n = 20)
Postoperative
(n = 20) p
Question
modifications of this score or alternative symptom scores for storage symptoms of the lower urinary tract, as well as for other important urologyical problems.
In conclusion, the results of our study suggest that the scored storage symptoms questionaire is of value in determining changes in the storage symptoms of the lower urinary tract, and it is a sensitive method for predicting USI.
A
ACCKKNNOOWWLLEEDDGGMMEENNTT
The authors would like to thank Miss Kuei- Yung Yang for her assistance.
R
REEFFEERREENNCCEESS
1. M i l s o m I , A b r a m s P, C a r d o z o L , e t a l . H o w widespread are the symptoms of an overactive bladder and how are they managed? A population- based prevalence study. BJU Int 2001;87:760-6.
2. Lin LY, Yeh NH, Lin CY, et al. Comparisons of urodynamic characteristics between female patients with overactive bladder and overactive bladder plus stress urinary incontinence. Urology 2004;64:945-9.
3. Digesu GA, Khullar V, Cardozo L, et al. Overactive bladder symptoms: do we need urodynamics?
Neurourol Urodyn 2003;22:105-8.
4. Klovning A, Hunskaar S, Eriksen BC. Validity of a scored urological history in detecting detrusor instability in female urinary incontinence. Acta Obstet Gynecol Scand 1996;75:941-5.
5. Kauppila A, Alavaikko P, Kujansuu E. Detrusor instablity score in the evaluation of stress urinary incontinence. Acta Obstet Gynecol Scand 1982;61:
137-41.
6. Lin HH, Torng PL, Sheu BC, et al. Urodynamically age-specific prevalence of urinary incontinence in women with urinary symptoms. Neurourol Urodyn 2003;22:29-32.
7. Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003;61:37- 49.
8. Sackett DL, Haynes RB, Guyatt GH, et al. Clinical Epidemiology: a Basic Science for Clinical Medicine.
2ndedition. Boston: Little-Brown, 1991:125-32.
9. Lagro-Janssen AL, Debruyne FM, van Weel C. Value of the patient's case history in diagnosing urinary incontinence in general practice. Br J Urol 1991;67:
569-72.
10. Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chronic Dis 1985;38:
27-31.
11. Uebersax JS, Wyman JF, Shumaker SA, et al. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn 1995;14:131-9.
1,2 1,3 1,2 1,3 1,3
1
2 3
404 2
2006 6 13 2006 7 3
2006 9 27
238
12 2
8 2 % 8 5 % 7 9 % 8 7 % 84%
20 6
2006;11:222-9