Introduction
The delivery of home care services is an important part of both the medical care system and the long-term care system. In Taiwan, the percentage of elderly people in the population increased from 2.5% in 1951 to 7.8% in 1996, and is expected to be 21.7% in 2036.1 The number of dependent elderly persons with ≥ 2 impaired activities of daily living is estimated to increase from 60,900 in 1995 to 141,700 in 2020, and 252,700 in 2035.2Currently, patients served by home care agencies in Taiwan are usually bed-bound with limited self-care ability because of various under-lying illnesses. On the other hand, 90% of the home
care agencies belong to hospitals, 4.3% to public health stations, 2.2% to nursing homes, and 3.2% are independent. These agencies are not equally distrib-uted throughout large cities and rural areas.3Previous studies of home care services in Taiwan primarily con-centrated on assessment of needs,4,5 health status,6 costs,7and quality of services.3There is a lack of stud-ies on the actual health care utilization of home care patients in Taiwan. A detailed report of the current situation would help health care providers and health policymakers identify deficiencies and develop a com-prehensive plan.
The aim of this study was to survey the health care utilization of patients in a home care agency of an
Health Care Utilization of Home Care Patients at
an Academic Medical Center in Taiwan
Yu-Ching Chou1, Liang-Kung Chen2,3, Yu-Ju Lin4, Li-Fang Chou5,
Tzeng-Ji Chen2,3*, Shinn-Jang Hwang2,3
1Department of Family Medicine, Yuan-Shan Veterans Hospital, Ilan, 2Department of Family Medicine, Taipei
Veterans General Hospital, 3School of Medicine, 4Institute of Health and Welfare Policy, National Yang-Ming
University, and 5Department of Public Finance, National Chengchi University, Taipei, Taiwan, R.O.C.
Background: Previous surveys of home care patients in Taiwan have primarily concentrated on patients’ status and needs. The aim of this study was to review the actual health care utilization of home care patients during the course of 1 year.
Methods: Home care patients at an academic medical center in Taiwan were selected and their insurance claims data at this hospital in 2001 were analyzed. Analyses included the patients’ patterns and diagnoses of visits and admissions, and their drug utilization. For diagnoses made at outpatient departments, the grouping system from the National Hospital Ambulatory Medical Care Survey in the United States was used. The Anatomical Therapeutic Chemical Classification system was applied to drug grouping.
Results: The home care agency of the hospital cared for 165 patients (66 women, 99 men) in 2001. In total, these 165 patients received 1,358 home visits, 2,751 outpatient visits, and 108 inpatient admissions. While the most fre-quent diagnoses for all visits were cerebrovascular disease, hypertension, diabetes mellitus, chronic and unspecified bronchitis, psychoses, and other disorders of the central nervous system, the most frequent diagnoses at discharge from the hospital were urinary tract infection and pneumonia. In all visits, 12,282 items of drugs were prescribed in 2,337 prescriptions. On average, each prescription contained 5.3± 2.8 items of drugs. The most frequently prescribed drugs were antacids, expectorants, laxatives, selective calcium channel blockers, and antithrombotic agents.
Conclusion: The home care agency of the hospital should pay more attention to provision of comprehensive care and review of drug prescribing. [J Chin Med Assoc 2006;69(11):523–528]
Key Words: academic medical centers, health care surveys, home care, long-term care, Taiwan
*Correspondence to: Dr Tzeng-Ji Chen, Department of Family Medicine, Taipei Veterans General Hospital, 201, Section 2, Shih-Pai Road, Taipei 112, Taiwan, R.O.C.
academic medical center in Taiwan. Analyses included the diagnoses, drug use, and admissions of these patients.
Methods
The academic medical center of the current study is the largest public hospital in Taipei, Taiwan, and is a major teaching hospital affiliated with several medical schools. It has 2,800 inpatient beds and a polyclinic with an average of 10,000 outpatients daily. Nearly all patients are insured under the National Health Insurance (NHI) program in Taiwan. We enrolled all the active patients of the hospital-based home care agency from January 1, 2001 to December 31, 2001. These patients received regular home visits by physicians and nurses from the department of family medicine of the hospital.
NHI claims data of the enrolled patients in the hospital in 2001 were used for analysis. The claims included visit, admission, and prescription files. The visit file recorded encounter data such as the patient’s sex, birthday, physician’s specialty, date of consulta-tion, and up to 3 diagnoses coded according to the International Classification of Disease, 9th revision, Clinical Modification (ICD-9-CM) for each visit. The admission file can include 5 diagnoses for each ad-mission. Because the ICD-9-CM contains more than 15,000 codes, the analysis would be less feasible with-out prior grouping. For the with-outpatient sector, we adopted the grouping system specifically developed by the National Ambulatory Medical Care Survey in the USA, where all diagnostic codes were reclas-sified into 194 diagnosis groups.8 For the inpatient sector, we grouped the diagnoses according to the first 3 digits of each ICD-9-CM code. The prescrip-tion file contained data of prescribed drugs such as drug name, dosage, route, frequency, amount, and costs in each visit and admission. Drugs were classified according to the Anatomical Therapeutic Chemical (ATC) Classification system.9
The claims data used in the current study were not limited to the services provided by the home care agency of the hospital. They included all kinds of ser-vices provided by the health care professionals of the hospital. The insurance claims served for and did not contain information about the patient’s activities of daily living.
Microsoft Access 2000 database software was used for data linkage and processing. The plain descriptive statistics including the count, mean, standard devia-tion (SD), and percentage were calculated. Because the annual number of visits varied from patient to patient, and a patient with more than 1 visit might be repeat-edly counted in the visit-based calculation, the denomi-nators of analyses included both total number of visits and total number of patients.
Results
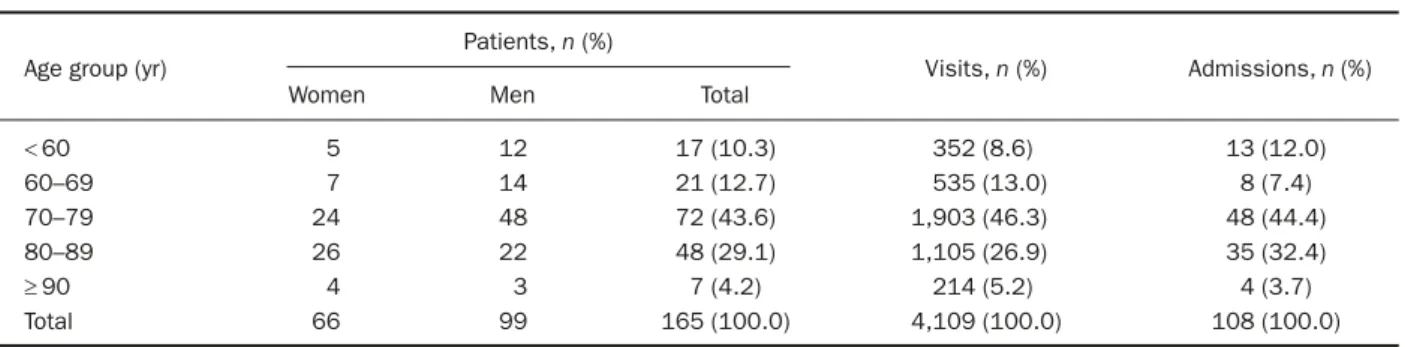
In 2001, home care services of the hospital were offered to 165 patients (66 women, 99 men). Mean patient age was 72.0± 13.6 years (range, 23–96 years), and 9-tenths of the patients were older than 60 years (Table 1).
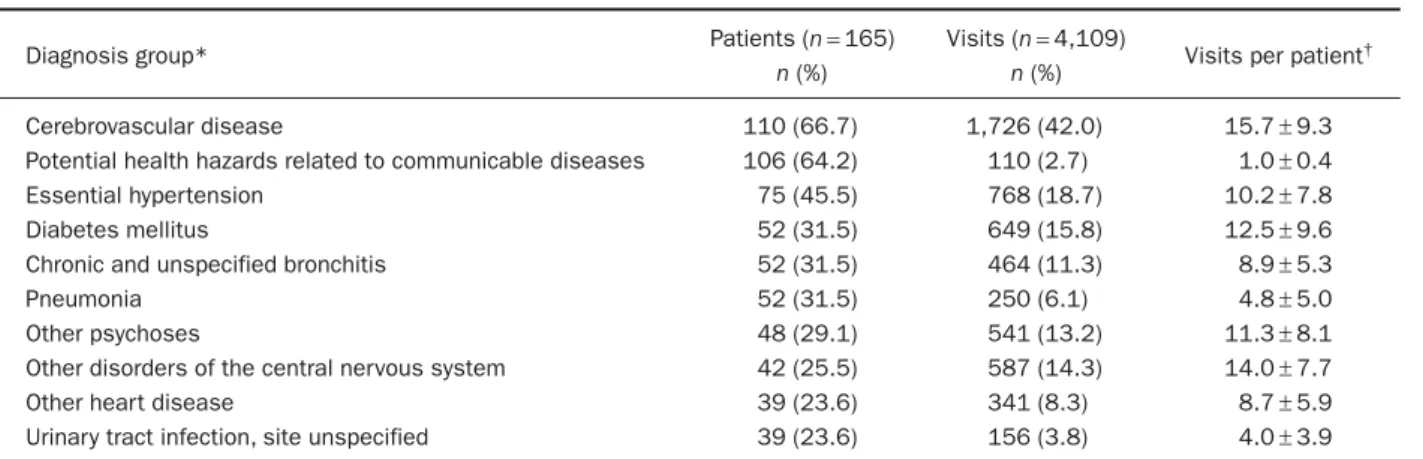
Apart from the 1,358 home visits provided by the department of family medicine, the patients also made 2,751 visits to other specialties of the hospital during the year. The 5 most frequent departments of outpatient visits were the departments of neurology (304 visits by 49 patients), general internal medicine (194 visits by 81 patients), dermatology (124 visits by 20 patients), cardiology (119 patients by 19 patients), and urology (79 visits by 10 patients). Diagnoses of cerebrovas-cular diseases were specified in 2-fifths of all visits by 2-thirds of patients. Other frequent diagnoses included essential hypertension, diabetes mellitus, chronic and unspecified bronchitis, psychoses, and other disorders of the central nervous system (Table 2).
Among the home care patients, 72 (43.6%) patients were admitted to the hospital, with a total of 108 admissions during the year. Twenty departments took
Table 1. Characteristics and health care utilization of home care patients
Age group (yr)
Patients, n (%)
Visits, n (%) Admissions, n (%) Women Men Total
< 60 5 12 17 (10.3) 352 (8.6) 13 (12.0) 60–69 7 14 21 (12.7) 535 (13.0) 8 (7.4) 70–79 24 48 72 (43.6) 1,903 (46.3) 48 (44.4) 80–89 26 22 48 (29.1) 1,105 (26.9) 35 (32.4) ≥ 90 4 3 7 (4.2) 214 (5.2) 4 (3.7) Total 66 99 165 (100.0) 4,109 (100.0) 108 (100.0)
part in the inpatient care. The top 5 specialties of admissions were the departments of chest medicine (18 admissions), neurology (16), infectious diseases (12), family medicine (11), and urology (7). The most frequent diagnoses at discharge from hospital were urinary tract infection and pneumonia (Table 3).
In total, 12,282 items of drugs were prescribed in 2,337 prescriptions at the outpatient departments for all home care patients. On average, each prescription con-tained 5.3± 2.8 items of drugs. Expressed in the third
level of ATC drug classification, the most frequently prescribed drugs for all patients were antacids, expec-torants, laxatives, selective calcium channel blockers, and antithrombotic agents (Table 4).
Discussion
A survey in the United States showed that family physicians did more home visits than internists.10There
Table 2. Distribution of illnesses and visits of home care patients
Diagnosis group* Patients (n= 165) Visits (n= 4,109) Visits per patient†
n (%) n (%)
Cerebrovascular disease 110 (66.7) 1,726 (42.0) 15.7± 9.3 Potential health hazards related to communicable diseases 106 (64.2) 110 (2.7) 1.0± 0.4 Essential hypertension 75 (45.5) 768 (18.7) 10.2± 7.8 Diabetes mellitus 52 (31.5) 649 (15.8) 12.5± 9.6 Chronic and unspecified bronchitis 52 (31.5) 464 (11.3) 8.9± 5.3
Pneumonia 52 (31.5) 250 (6.1) 4.8± 5.0
Other psychoses 48 (29.1) 541 (13.2) 11.3± 8.1 Other disorders of the central nervous system 42 (25.5) 587 (14.3) 14.0± 7.7 Other heart disease 39 (23.6) 341 (8.3) 8.7± 5.9 Urinary tract infection, site unspecified 39 (23.6) 156 (3.8) 4.0± 3.9
*Grouping according to Reference 8; †data presented as mean± standard deviation.
Table 3. Distribution of illnesses and admissions of home care patients
ICD-9-CM* Diagnosis group Admissions (n= 108) Patients (n= 165)
n (%) n (%)
599 Other disorders of urethra and urinary tract 39 (36.1) 29 (17.6) 486 Pneumonia, organism unspecified 33 (30.6) 26 (15.8) 401 Essential hypertension 32 (29.6) 27 (16.4) 250 Diabetes mellitus 32 (29.6) 24 (14.5) 438 Late effects of cerebrovascular disease 28 (25.9) 25 (15.2) 290 Senile and presenile organic psychotic conditions 13 (12.0) 13 (7.9) 331 Other cerebral degenerations 9 (8.3) 5 (3.0) 518 Other diseases of the lung 8 (7.4) 8 (4.8) 434 Occlusion of cerebral arteries 8 (7.4) 7 (4.2) 582 Chronic glomerulonephritis 8 (7.4) 6 (3.6) 348 Other conditions of brain 8 (7.4) 5 (3.0)
428 Heart failure 8 (7.4) 4 (2.4)
427 Cardiac dysrhythmias 7 (6.5) 5 (3.0)
276 Disorders of fluid, electrolyte, and acid-base balance 6 (5.6) 6 (3.6)
342 Hemiplegia 6 (5.6) 6 (3.6)
707 Chronic ulcer of skin 6 (5.6) 6 (3.6) 788 Symptoms involving urinary system 6 (5.6) 4 (2.4)
038 Septicemia 5 (4.6) 5 (3.0)
507 Pneumonitis due to solids and liquids 5 (4.6) 5 (3.0) 578 Gastrointestinal hemorrhage 5 (4.6) 5 (3.0) 496 Chronic airway obstruction, not elsewhere classified 5 (4.6) 4 (2.4) 402 Hypertensive heart disease 5 (4.6) 3 (1.8) 600 Hyperplasia of prostate 5 (4.6) 3 (1.8)
is no similar study in Taiwan. At the academic medical center of our study, home visits to home care patients were generally offered by physicians and nurses of the department of family medicine. Most of these home care patients were either immobile or had limited activities of daily living. But, the outpatient visits at other specialties among these patients were twice the number of home visits. Patients in Taiwan have the right to free access to specialists without referrals. Even though an outpatient visit might be a referral from the physicians and nurses of the home care agency, the total number of outpatient visits to specialists seemed too high. Besides the multi-morbidity of patients, the
competence of home care agencies in providing com-prehensive care needs further examination.
The kinds of illnesses requiring medical help are associated with underlying diseases. For example, falls, urinary tract infection, and chest infection are the most common complications after acute stroke.11 In our study, we could observe similar associations. Two-thirds of our patients had a diagnosis of cerebrovas-cular disease. Because physicians might not code the preexisting diseases in visits for other problems, the actual percentage of patients with cerebrovascular disease may have been higher. On the other hand, urinary tract infection and pneumonia were the most
Table 4. Drug utilization at the outpatient departments by the third level of Anatomical Therapeutic Chemical (ATC) Classification
Prescribed items Prescriptions* Patients
Prescriptions ATC code Group name (n= 12,282) (n = 2,337) (n = 165)
n (%) n (%) n (%) per patient
†
A02A Antacids 1,337 (10.9) 1,219 (52.2) 136 (82.4) 9.0± 4.9 R05C Expectorants, excl. combinations with 856 (7.0) 784 (33.5) 105 (63.6) 7.5± 4.2
cough suppressants
A06A Laxatives 799 (6.5) 775 (33.2) 89 (53.9) 8.7± 4.6 C08C Selective calcium channel blockers 551 (4.5) 545 (23.3) 59 (35.8) 9.2± 4.0
with mainly vascular effects
B01A Antithrombotic agents 534 (4.3) 481 (20.6) 56 (33.9) 8.6± 4.0 N03A Antiepileptics 443 (3.6) 383 (16.4) 42 (25.5) 9.1± 4.1 A10B Oral blood glucose lowering drugs 389 (3.2) 297 (12.7) 32 (19.4) 9.3± 3.8 S01A Anti-infectives 375 (3.1) 362 (15.5) 61 (37.0) 5.9± 4.5 D07A Corticosteroids, plain 336 (2.7) 325 (13.9) 56 (33.9) 5.8± 4.7 C04A Peripheral vasodilators 335 (2.7) 319 (13.6) 38 (23.0) 8.4± 4.2 C09A ACE inhibitors, plain 299 (2.4) 299 (12.8) 32 (19.4) 9.3± 3.6 N02B Other analgesics and antipyretics 255 (2.1) 250 (10.7) 67 (40.6) 3.7± 3.2 C07A Beta blocking agents 250 (2.0) 250 (10.7) 34 (20.6) 7.4± 4.4 R06A Antihistamines for systemic use 250 (2.0) 198 (8.5) 45 (27.3) 4.4± 5.0 R05F Cough suppressants and expectorants, 247 (2.0) 245 (10.5) 56 (33.9) 4.4± 3.7
combinations
N05A Antipsychotics 232 (1.9) 219 (9.4) 26 (15.8) 8.4± 4.7 N06A Antidepressants 208 (1.7) 188 (8.0) 21 (12.7) 9.0± 4.3 A03F Propulsives 207 (1.7) 203 (8.7) 33 (20.0) 6.2± 4.7 C01D Vasodilators used in cardiac diseases 201 (1.6) 191 (8.2) 22 (13.3) 8.7± 4.7 R03C Adrenergics for systemic use 198 (1.6) 182 (7.8) 25 (15.2) 7.3± 4.0 N05B Anxiolytics 190 (1.5) 188 (8.0) 32 (19.4) 5.9± 4.3 R03D Other anti-asthmatics for systemic use 173 (1.4) 173 (7.4) 26 (15.8) 6.7± 4.0 A07F Antidiarrheal microorganisms 157 (1.3) 157 (6.7) 18 (10.9) 8.7± 4.1 D01A Antifungals for topical use 150 (1.2) 140 (6.0) 28 (17.0) 5.0± 3.6 J01E Sulfonamides and trimethoprim 135 (1.1) 135 (5.8) 34 (20.6) 4.0± 3.3 N04B Dopaminergic agents 127 (1.0) 99 (4.2) 10 (6.1) 9.9± 3.3 J01C Beta-lactam antibacterials, penicillins 124 (1.0) 120 (5.1) 39 (23.6) 3.1± 2.2 N05C Hypnotics and sedatives 119 (1.0) 118 (5.0) 17 (10.3) 6.9± 5.1 G04C Drugs used in benign prostatic hypertrophy 117 (1.0) 117 (5.0) 14 (8.5) 8.4± 4.8 J07B Viral vaccines 105 (0.9) 105 (4.5) 105 (63.6) 1.0± 0.0 M02A Topical products for joint and muscular pain 101 (0.8) 101 (4.3) 25 (15.2) 4.0± 4.0
frequent diagnoses of admissions. More attention should be paid to Foley care and respiratory care in home care patients.
In our study, antacids were prescribed frequently. Although antacids are not prescription-only drugs, they were reimbursed by the NHI in Taiwan before October 2005. It was reported that 2-fifths of pre-scriptions in Taiwan contained antacids and the per-centage was as high as 87% in prescriptions with non-steroidal anti-inflammatory drugs (NSAIDs).12But the concomitant prescribing of antacids and NSAIDs is not a good explanation of the use of antacids in our study because oral NSAIDs were seldom prescribed to our patients. The use of antacids might be partly attributable to the fact that magnesium compounds were usually taken as laxatives.
According to previous surveys of nursing homes in other developed countries, psychotropic drugs were prescribed most frequently, and the prevalence of psy-chotropic drug use among nursing home residents var-ied from 20% to 50%.13,14In our study, we calculated the use of separate groups of psychotropic drugs: anti-psychotics (15.8% of patients), anxiolytics (19.4%), hypnotics (10.3%), antidepressants (12.7%), and anti-epileptics (25.5%). These data seem to be comparable to the results of other studies. The prevalence of psy-chotropic drug use within the NHI in Taiwan was estimated to be 9.2% in 2000.15 It seems that the consumption of psychotropic drugs in our home care patients is higher than that in the general population. Annual influenza vaccination could lower morbid-ity and mortalmorbid-ity in high-risk elderly.16 In Taiwan, people older than 65 years, nursing home residents, and those with diabetes, cardiovascular disease, chro-nic pulmonary disease, chrochro-nic renal disease, and other immunocompromised diseases have been able to receive free annual influenza vaccination provided by the government since 1998. In our study, only 63.6% of the home care patients received vaccination at our hospital during the year. The cause for incomplete cov-erage could be either refusal by patients or vaccination at other clinics, e.g. public health station.
As a survey of the insurance claims, our current investigation had some limitations. First, patients’ com-plaints, symptoms, or other reasons for the visit were absent in the NHI claims. They could be inferred only from the diagnoses. Second, the diagnostic codes served for reimbursement and were seldom verified. Overdiag-nosing in the form of tentative diagnosis could not be ruled out. On the other hand, the outpatient claims contained only 3 diagnostic codes for each consulta-tion and the inpatient claims only 5 for each admis-sion. Not every underlying medical illness may have
been coded and there may have been underdiagnosis. Third, the prescription of drugs might only represent the prescribing behavior of physicians. The claims cannot differentiate between a physician’s professional judgment and the patient’s request. The prescription of antacids is an example. However, an approach with uniform electronic datasets remains a practical and objective method.
Our study was based on patients at an academic medical center. Our results might not be representa-tive of the national situation in Taiwan. Besides, any change in the criteria for patient enrollment within the NHI would influence the content of home care ser-vices. Because the academic medical centers in Taiwan currently play a large part in outpatient and inpatient health care, our experiences should still be of value to co-workers in related areas.
In conclusion, there is room for improvement in the home care agency of the hospital to provide com-prehensive care. More attention needs to be paid to urinary tract infection and pneumonia, as the most common diagnoses of admissions, in the care of home care patients in future. Polypharmacy is another issue that deserves further investigation. A system of routine monitoring and benchmarking might help to guarantee a high quality of care.
References
1. Manpower Planning Department. Projections of the Population
of Taiwan Area, Republic of China, 1995–2036. Taipei:
Man-power Planning Department, Council for Economic Planning and Development, Executive Yuan, 1997.
2. Department of Statistics. The Report on the Old Status Survey. Taipei: Department of Statistics, Ministry of the Interior, 2000. 3. Shyu YI, Liao MN, Shao JH, Yang CL. A survey of home nurs-ing services in Taiwan. Public Health Nurs 1999;16:432–40. 4. Yu YM, Wu KH, Chen HK, Chen YC. Possibility of Home Care
Service to be Included in the Planning Nationwide Insurance Program. Taipei: Department of Health, Executive Yuan, 1990.
5. Wu SZ, Chiou CJ. The exploration of related factors of nursing care programs in home health care patients. Nurs Res 1995; 5:279–89.
6. Ho YL. A Comparative Study on Three Long-term Care Modes
in Taiwan: Assessment of Resources Consumption, Health Status Changes, and Patients’ Family Satisfaction. Taichung: China
Medical College, 1992. [Master’s thesis]
7. Lee YC, Huang YW. A Study on Cost of Home Care Services. Taipei: Department of Health, Executive Yuan, 1995. 8. Schappert SM. Ambulatory care visits to physician offices,
hos-pital outpatient departments, and emergency departments: United States, 1997. Vital Health Stat 13 1999;143:1–39. 9. World Health Organization Collaborating Centre for Drug
Statistics Methodology. Guidelines for ATC Classification and
DDD Assignment, 3rdedition. Oslo: World Health Organization
Collaborating Centre for Drug Statistics Methodology, 2000. 10. Keenan JM, Boling PE, Schwartzberg JG, Olson L,
of the home visiting practice and attitudes of family physicians and internists. Arch Intern Med 1992;152:2025–32.
11. Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Com-plications after acute stroke. Stroke 1996;27:415–20. 12. Liu JY, Chen TJ, Hwang SJ. Concomitant prescription of
non-steroidal anti-inflammatory drugs and antacids in the outpatient setting of a medical center in Taiwan: a prescription database study. Eur J Clin Pharmacol 2001;57:505–8.
13. van Dijk KN, de Vries CS, van den Berg PB, Brouwers JRBJ, de Jong-van den Berg LTW. Drug utilisation in Dutch nursing homes. Eur J Clin Pharmacol 2000;55:765–71.
14. Ruths S, Straand J, Nygaard HA. Psychotropic drug use in nursing homes: diagnostic indications and variations between institutions. Eur J Clin Pharmacol 2001;57:523–8.
15. Su TP, Chen TJ, Hwang SJ, Chou LF, Fan AP, Chen YC. Utilization of psychotropic drugs in Taiwan: an overview of outpatient sector in 2000. J Chin Med Assoc 2002;65: 378–91.
16. Gross PA, Hermogenes AW, Sacks HS, Lau J, Levandowski RA. The efficacy of influenza vaccine in elderly persons: a meta-analysis and review of the literature. Ann Intern Med 1995; 123:518–27.