行政院國家科學委員會專題研究計畫 成果報告
體外震波碎石術對人體內白血球產生自由基,紅血球內的抗
氧化酵素以及脂質過氧化反應的變化情形
計畫類別: 個別型計畫 計畫編號: NSC91-2314-B-002-372- 執行期間: 91 年 08 月 01 日至 92 年 07 月 31 日 執行單位: 國立臺灣大學醫學院泌尿科 計畫主持人: 陳淳 計畫參與人員: 黃鶴翔 報告類型: 精簡報告 處理方式: 本計畫可公開查詢中 華 民 國 92 年 10 月 16 日
行政院國家科學委員會補助專題研究計畫
□成果報告 □期中進度報告 體外震波碎石術對人體內白血球產生自由基,紅血球內的抗氧化酵素以及脂質過 氧化反應的變化情形計畫類別:
; 個別型計畫 □ 整合型計畫
計畫編號:NSC91-2314-B002-372- -
執行期間:91 年 08 月 01 日至 92 年 07 月 31 日
計畫主持人:陳淳
共同主持人:黃鶴翔
計畫參與人員:
成果報告類型(依經費核定清單規定繳交):;精簡報告 □完整
報告
本成果報告包括以下應繳交之附件:
□赴國外出差或研習心得報告一份
□赴大陸地區出差或研習心得報告一份
□出席國際學術會議心得報告及發表之論文各一份
□國際合作研究計畫國外研究報告書一份
處理方式:除產學合作研究計畫、提升產業技術及人才培育研究計畫、列管計畫 及下列情形者外,得立即公開查詢 □涉及專利或其他智慧財產權,□一年□二年後可公開查詢執行單位:台大醫學院泌尿部
中 華 民 國 92 年 10 月 15 日
中文摘要及關鍵詞:體外震波碎石術是一種非侵襲性的治療尿路結石的一種治療方式。但是,由 文獻上的報告顯示,體外震波碎石術本身並非是一種完全無副作用的治療方式。 如果利用顯微鏡來作組織學的觀察,可以發現腎臟小管細胞在接受體外震波處理 之後,細胞質內會出現氣泡、空洞的現象。另外也有實驗發現:在接受震波處理 過的組之內也會發現有 hydroxyl 自由基生成增加的現象。而這種現象則表示: 在接受震波處理過的組織內,該組織內產生氧化壓力的來源和產生過氧化反應增 加。而在另一個實驗中發現,腎臟在接受體外震波碎石術 24 小時之後,腎臟內 的 superoxide dismutase 和 catalase 的酵素活性會有顯著的降低現象。
在本實驗中共包含了 25 位腎結石的病患(group II), 25 位輸尿管結石的病患 (group III), 和 25 位年齡和性別都相當的對照組(group I)。 我們收集每一位受試
者的術前和接受體外震波碎石術 12 小時之後的尿液標本,以及 6 西西的血液標 本。 我們測試尿液標本中的 electrolyte, oxalate, citrate, tubular enzymes, 和 lipid
peroxides。 每位受試者的紅血球標本則檢查其中 Lipid peroxide 和 GSH/GSSG
的含量多寡變化。 白血球製造 superoxide anion 和 hydrogen peroxide 的能力變 化亦在每位受試者的血液中分離白血球來作測試。結果我們發現在第組和第 3 組的病人在接受體外震波碎石術後 12 小時,其尿液中的脂質過氧化產物仍有顯 著升高的現象, 尿液中的主要電解質是沒有差異,但是尿液中的蛋白質和草酸 鹽濃度仍有顯著的上升現象。此時的尿液中腎小管酵素則是回復到正常的水準。 這些結果顯示:經過體外震波碎石術治療後 12 小時,雖然腎小管的傷害已經恢 復,但是腎臟內的自由基生成量仍然升高。至於為何尿中的草酸鹽濃度比再接受 體外震波碎石術之前還要高,其作用機轉仍須進一步研究。 在周邊血液中,我們發現紅血球細胞膜上的 GSH 在第 2 組和第 3 組病人中 有顯著的降現象,這個發現和先前另一篇研究報告的:在動物實驗中腎臟內的 SOD 和 catalase 活性在接受體外震波碎石術之後會有顯著的下降是相符合的。但 是,紅血球細胞膜內的 MDA 和 TBARS(脂質過氧化產物)在第 2 組和第 3 組 病人中卻沒有顯著的變化。白血球製造自由基的能力在第 2 組和第 3 組病人於接 受體外震波碎石術之後,和對照組比較起來,亦無明顯的差異。以上的結果顯示: 體外震波碎石術對人體的傷害主要是發生在腎臟,會造成腎臟內自由基形成的增 加,而體外震波碎石術所造成的腎小管傷害,可在體外震波碎石術 12 小時後恢 復。體外震波碎石術對於周邊血液中的 component 影響不大,並不會造成白血球 的活化,但是會減少紅血球中 GSH 的含量,但並不會造成紅血球氧化壓力的增 加。 關鍵詞: 體外震波碎石術,自由基,高草酸尿症,草酸鈣結石。 英文摘要及 keywords:
Extracorporeal shock wave lithotripsy (ESWL) is a noninvasive routine treatment modality for urolithiasis. However, it is not completely free from side effects. Microscopic examination of urine voided immediately after ESWL frequently demonstrates vacuolized renal tubular cells. Another study reported that a significant amount of hydroxyl radical was measured in the affected tissue. This revealed the source of oxidant stress and peroxidation reactions in the ESWL-treated kidney tissue increased. Free-radical scavenger enzymes (superoxide dismutase and catalase) decreased significantly in the kidney tissue after 24 hours following ESWL treatment was also reported.
There were 25 kidney stone patients (group II), 25 ureteral stones patients (group III), and 25 age and sex matched controls (group I) included in this study. 24-hour urine and 6 ml peripheral whole blood were drawn in each subject before and 12-hour following ESWL treatment. Urinary electrolyte, oxalate, citrate, tubular enzymes, and lipid peroxides were evaluated. Lipid peroxide and GSH/GSSG were evaluated in each RBC sample. The ability to produce superoxide anion, and hydrogen peroxide were evaluated in each WBC sample. In this study we found that urinary lipid peroxides increased significantly in patients with kidney and ureteral stones received ESWL treatment. After 12 hour following ESWL, urinary oxalate and protein levels increased significantly, but tubular enzymuria returned to the basal levels. These results implied that free radical production still increase in the kidney 12 hours after ESWL treatment, though there was no significant renal tubular damage already. The mechanism that caused the urinary oxalate level further increased after ESWL is unknown, and need further evaluation.
In the circulation, GSH decreased in the RBC membrane was found in patient with urolithiasis and treated ESWL, and this result was comparable with the animal model which found the activity of SOD and catalase in the kidney decreased after ESWL treatment. However, MDA and TBARS had no significant change in the RBC membrane when compared with the controls. The ability to produce free radical in the WBC of peripheral circulation also had no significant difference when compared with the controls. These results implied that the major trauma caused by ESWL was in the kidney, where free radical production increased. Tubular damage could recover soon after 12 hours following ESWL treatment. ESWL trauma to the components in the circulation was rare, only decreased GSH was found.
Keywords: Extracorporeal shock wave lithotripsy, free oxygen radicals, hyperoxaluria, calcium oxalate stone.
會合併有腎臟內自由基的產生[1]。但是,由血液中所測得到上升的冷光值,只 有在第七天時才被發現,在餵食以烯甘醇 21-42 天後,卻無法再由血液中測得任 何冷光值有上升的趨勢,只有從腎臟經灌流 nitroblue tetrazolium (NBT)之後由腎 臟組織切片上觀察到仍有自由基產生增加的現象[2]。配合 common leukocyte
antigen 以及 macrophage 的 immunohistochemical 的染色,我們發現在腎臟內逐
漸增加的 monocyte 或 macrophage 可能是在結石後期腎臟內自由基仍增加的一個 重要原因[2]。Thamilselvan 等人在 1997 年時發表論文顯示:用乙烯甘醇來誘發 腎結石的模式中,是會伴隨腎臟內 lipid peroxidation 增加的現象,而且是由一開 始餵食乙烯甘醇開始至六十天止都有[3]。可見得在腎臟因高草酸尿症而產生草 酸鈣結石的同時,腎臟本身就受到 oxidative stress 的影響了。 腎結石經過 ESWL 治療後,1 年之後有 6%的病人會復發,3 年內有 28%,5 年內有 42%,九年內則有大於 70%的病人會復發腎結石[4]。 男性病患和有
multiple renal stone disease 是 ESWL 之後會再產生腎結石的重要因素[5]。 在接
受 ESWL 之後,Williams et al 發現 GFR 會下降 5% [6]。 Lechevallier et al 利用
single-photon emission computed tomography 來評估腎臟在接受治療後 30 天,其
腎實質上的 scarring 情形:結果發現接受 ESWL 治療後,有 33%的腎臟實質會 產生 4%的 scar,而 20%做過 PCNL 的腎臟才會產生這樣的 scar [7]。Evan 等人 曾針對 ESWL 後的腎臟,觀察局部地區的組織變化發現:所有震波經過的區域 都有受傷,尤其是血管和腎小管組織,會造成 tubular basement membrane
disruption [8]。 但仍有一部份的 damaged tissue 會變成纖維化,以及逐漸喪失 post-glomerular capillary。 最近,Willis 等人發現:在那些腎臟較小的或是已經
有 damaged kidney,ESWL-induced renal damage 會顯得特別顯著,而這兩種情 況也正是經常會發生在結石患者身上[9]。
由以上的 review 可發現:ESWL 對腎臟的傷害可能是經由兩途徑:高能量
的震波會對腎臟細胞造成直接的傷害,另外,腎臟血管的受傷可能會造成局部的 缺氧,而使得自由基的產生增加[10]。在動物實驗中,已發現 ESWL 會造成腎小 管的傷害,腎臟組織內的 catalase 和 SOD 的 enzyme level 顯著的下降,腎臟內的
lipid peroxidation 也會增加[10-13]。 所以,因高草酸尿而產生草酸鈣腎結石的病
患,在接受 ESWL 的時候,理論上腎臟會受到更大的 oxidative stress!
Superoxides 在生物體內,可以在以下的情況產生出來:by xanthine oxidase in endothelial cells, NAD(P)H oxidase 和 myeloperoxidase in activated phagocytes (neutrophils, monocytes and Kupffer cells), leakage of reactive oxygen from the mitochondrial respiratory chain, the arachidonic acid cascade, 以及 oxidation of NAD(P)H at the microsome 等等 [14-17]。 但是,在腎結石的過程中或是腎臟在
做 ESWL 時,superoxides 是由何處所產生的仍不是很清楚。 草酸鈣結晶在腎臟 內會誘發發炎反應,包括增加腎臟間質細胞的數目,以及讓腎臟間質的 matrix 增加等等 [18]. 在人和老鼠的腎臟內,macrophages 和 multinucleated giant cells 是主要包住存在在間質草酸鈣結晶的細胞。草酸鈣結晶也已經證實會引起
cytolysis of polymorphonuclear leukocytes and erythrocytes [19]. 多形性白血球可
以被很多病症所活化,例如:neurodegenerative disorders, chronic inflammatory
disease, atherosclerosis, and cancer, 而會去附著上內皮細胞,進而產生自由基[20].
由我們之前的實驗:我們發現 PMN infiltration into kidney 是在餵食乙烯甘醇後 第七天到第 21 天間會增加,腎臟內的抗氧化酵素活性則是到第 42 天時會降低
[2]。所以,在接受 ESWL 治療後的病人,其血液中的白血球是否有被活化,紅
血球內的抗氧化酵素是否有變化,仍不清楚。
研究目的、本文的研究目的是: 體外震波碎石術是否會對患有草酸鈣腎結石的病 患的 peripheral blood 中 oxidative stress 增加(自由基形成增加和紅血球抗氧化酵 素減低)。 另外, 是否 peripheral PMN 是引起體外震波碎石術升高腎臟 lipid
peroxidation 產物增加的原因。
研究方法、
1. Normal controls and Patients:
25 kidney stone patients (group II), 25 ureteral stones patients (group III), and 25 age and sex matched controls (group I) will be chosen for this study.
Group II 和 group III 病人在 ESWL 前先做一套下列所述的檢查,術後 12 小時
再測一次。
2. Measurement of Ccr, urine oxalate levels, urinary lipid peroxides (MDA, and thiobarbituric acid reacting substance (TBARS)
A). Twelve-hour urine specimens were collected from patients of all groups. The
total urinary volume was recorded and urinary creatinine (Cr), protein, and oxalate levels were determined. Cr was examined at the central laboratory of NTUH. Urinary protein was determined by a protein assay kit (Bio-Rad Protein Assay Kit), while the level of urinary oxalate was determined by a commercial available kit (Sigma). Urinary citrate levels were checked by a commercial available kit. Plasma creatinine levels were examined in each patient and to determine their
Creatinine clearance rate (Ccr).
B). Thiobarbituric acid (TBA) and MDA assay :
RBC and urine lipid peroxide level: used OXIS available kit.
3. Concentration of GSH and GSSG
The reduced (GSH) and the oxidized (GSSG) form of glutathione of whole blood (heparin-anticoagulated) are determined by OXIS kit.
4. PMN oxidative burst response (Lucigenin-amplified chemiluminescence):
Peripheral venous blood samples were obtained at 7:00 A.M. from the patients in all three groups. Blood samples were withdrawn in EDTA-prepared tubes and
immediately forwarded for PMN isolation. The EDTA-anticoagulated blood was centrifuged in a Ficoll-HyPaque density gradient centrifugation(300 g), erythrocytes were sedimented with polyvinyl alcohol and residual erythrocytes were removed by hypotonic lysis. Cells were washed twice (150 X g, 10 min, 4℃) and resuspended in phosphate-buffered saline (298 mM) with Ca2+ and Mg2+ (PBS) at a final
concentration of 5 X 106/ml. The lucigenin-enhanced chemiluminescence (CL) of 109 PMN/L, activated by 3% H2O2, were investigated using the CL Analyzing
System (CLD-110, Tohoku Electronic Industrial Co., Sendai, Japan). The system contains a photon detector (Model CLD-110), CL counter (Model CLC-10), water circulator (Model CH-200), and a 32-bit personal computer system. A cooler
circulator was connected to the photon detector to maintain the temperature at 5℃. 0.2 ml sample (109 PMN/L) were added to a stainless-steel cell (5 cm in diameter) and the CL was measured. After 100 seconds (to determine the background level), 1.0 ml of 1.5 mmol/L luciginin was injected into the cells. The CL in this sample was continuously measured for another 500 seconds. The total amount of CL was calculated by integrating the area under the curve and subtracting it from the
background level (equivalent to the mean dark value). Samples were expressed as CL counts/10s for each sample.
* Enhanced chemiluminescence:
Phorbol-myristate acetate (PMA)-induced superoxide production: 200 ng/ml
PMA is added along with luciginin as mentioned above.
5. Measurement of urinary tubular enzymes:
Urinary NAG and βGAL were determined according to Maruhn's method. Urinary enzyme activities were expressed per gram of urinary creatinine as described by Baggio et al.
6. Statistics:
Statistical analysis will be carried out using one-way ANOVA and Student’s t-test. All values are reported as mean ± SE. Paired t-test will be used to analyze the significance of parameters before and after removal of kidney or ureteral stones. A p valueless than 0.05 is considered significant different. The correlation between lipid peroxidation and urine tubular enzymes will be analyzed by linear regression.
結果與討論、
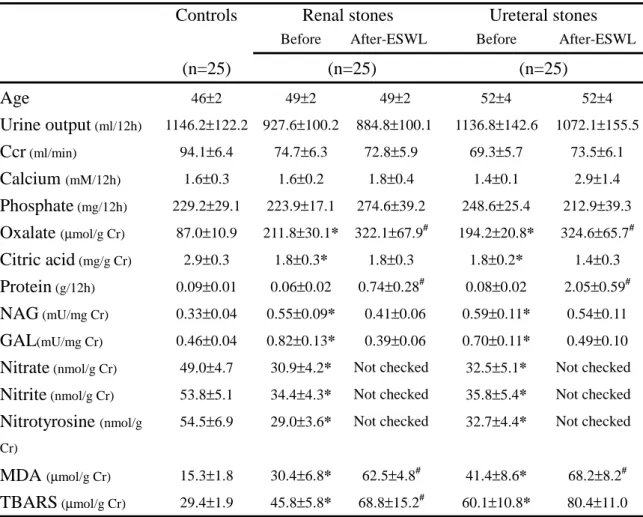
Table 1. Results of renal tubular enzymes, lipid peroxides, oxalate, citrate, and
electrolytes in the urinary samples.
* p < 0.05 when compared with the normal controls.
# p < 0.05 when compared the data before and after ESWL in patients of group II and group III.
Controls Renal stones Ureteral stones
Before After-ESWL Before After-ESWL
(n=25) (n=25) (n=25) Age 46±2 49±2 49±2 52±4 52±4 Urine output (ml/12h) 1146.2±122.2 927.6±100.2 884.8±100.1 1136.8±142.6 1072.1±155.5 Ccr (ml/min) 94.1±6.4 74.7±6.3 72.8±5.9 69.3±5.7 73.5±6.1 Calcium (mM/12h) 1.6±0.3 1.6±0.2 1.8±0.4 1.4±0.1 2.9±1.4 Phosphate (mg/12h) 229.2±29.1 223.9±17.1 274.6±39.2 248.6±25.4 212.9±39.3 Oxalate (µmol/g Cr) 87.0±10.9 211.8±30.1* 322.1±67.9# 194.2±20.8* 324.6±65.7# Citric acid (mg/g Cr) 2.9±0.3 1.8±0.3* 1.8±0.3 1.8±0.2* 1.4±0.3 Protein (g/12h) 0.09±0.01 0.06±0.02 0.74±0.28# 0.08±0.02 2.05±0.59# NAG (mU/mg Cr) 0.33±0.04 0.55±0.09* 0.41±0.06 0.59±0.11* 0.54±0.11 GAL(mU/mg Cr) 0.46±0.04 0.82±0.13* 0.39±0.06 0.70±0.11* 0.49±0.10
Nitrate (nmol/g Cr) 49.0±4.7 30.9±4.2* Not checked 32.5±5.1* Not checked
Nitrite (nmol/g Cr) 53.8±5.1 34.4±4.3* Not checked 35.8±5.4* Not checked
Nitrotyrosine (nmol/g Cr)
54.5±6.9 29.0±3.6* Not checked 32.7±4.4* Not checked
MDA (µmol/g Cr) 15.3±1.8 30.4±6.8* 62.5±4.8# 41.4±8.6* 68.2±8.2#
TBARS (µmol/g Cr) 29.4±1.9 45.8±5.8* 68.8±15.2# 60.1±10.8* 80.4±11.0
Table 2. Lipid peroxides, glutathione, glutathione reductase, and nitrotyrosin levels in
the samples of RBC of different group patients.
Controls Renal stones Ureteral stones
Before After-ESWL Before After-ESWL
(n=25) (n=25) (n=25) Nitrotyrosine (nmol/g Hb) 0.87±0.03 0.89±0.04 Not checked 0.94±0.06 Not checked
GSH (µM/g Hb) 4.86±1.22 1.60±0.41* 0.60±0.14# 1.42±0.11* 0.76±0.17#
GSSG (µM/g Hb) 0.14±0.04 0.40±0.03* 0.46±0.16 0.42±0.04* 0.45±0.15
GSH/GSSG 49.3±13.8 2.4±0.8* 1.3±0.4* 1.5±0.2* 1.2±0.3*
Glutathione reductase (mU/mg Hb)
0.44±0.12 0.27±0.03 Not checked 0.51±0.05† Not checked
MDA (µmol/g Hb) 0.020±0.001 0.035±0.005* 0.041±0.004 0.027±0.001* 0.031±0.004
TBARS (µmol/g Hb) 0.24±0.02 0.28±0.02 0.35±0.03 0.30±0.02* 0.34±0.02
Oxalate (µmol/g Hb) 0.36±0.05 0.52±0.05* Not checked 0.51±0.06* Not checked
(CL) of polymorphonuclear neutrophils isolated from controls and patients with renal or ureteral stones. All figures are mean ± SE.
Controls Renal stones Ureteral stones Restin g PMA-sti mulated Resting PMA-sti mulated Resting PMA-stimul ated O2- production (mmol/106 cells/10 mins) 1.9±0.1 3.1±0.1 1.4±0.1* 2.1±0.1† 1.37±0.04* 1.98±0.08† H2O2 production (nmol/2.5x106 cells/15 mins) 4.1±0.1 14.7±0.5 3.5±0.1* 8.1±0.2† 3.67±0.09* 8.06±0.12† Myeloperoxidase (U/106 cells/min) 4.62±0.06 3.75±0.08* 3.79±0.09* CL ( X 104) 4.3±0.3 10.6±1.5 4.1±0.4 13.8±2.9 4.8±0.8 27.8±8.6† Renal stones Post-ESWL Ureteral stones Post-ESWL Resting PMA-sti mulated Resting PMA-stimul ated O2- production (mmol/106 cells/10 mins) 1.7±0.1 1.9±0.2 1.7±0.1 2.1±0.2 H2O2 production (nmol/2.5x106 cells/15 mins) 4.0±0.1 15.±0.5 4.4±0.2 7.2±0.5 CL ( X 104) 4.8±1.6 6.2±2.7 4.9±1.5 17.8±9.5
* p < 0.05 when compared with the normal controls at resting status.
† p < 0.05 when compared with the normal controls stimulated with PMA.
From the results in Table 1, we found that the major parameters changed after ESWL were the urinary oxalate levels, urinary protein levels, and urinary lipid peroxides in group II and group III patients. In Table 2, we found that the GSH content in RBC was further decreased in group II and group II patients after ESWL treatment, and had a statistical significance when compared with the controls and the same group before ESWL (p<0.05). There was no significant change in the lipid peroxides in RBC after ESWL in patients with urolithiasis (Table 2). After ESWL, there also had no significant changes in the superoxide or H2O2 production in the
peripheral WBC of patients with urolithiasis (Table 3).
Combining all results in this study, we found ESWL for kidney stone or ureteral stone had no significant influence on the peripheral RBC and WBC, except GSH levels in the RBC was decreased in stone patients after ESWL. The major effects of ESWL on the kidney were the prominent proteinuria, increased lipid peroxides and more prominent hyperoxaluria. From the histological findings of an animal study [21], we found that vascular damage was a prime feature of shock wave trauma and combined with lytic and sublethal injury to renal tubules and interstitium leading to infiltration by circulating leukocytes. Therefore, the phenomenon of proteinuria might be the result of vascular injury during ESWL treatment. After 12 hours of ESWL, the phenomenon of tubular damage was recovered, because the urinary tubular enzymuria had no significant differences in group II and group III patients when compared with the controls. However, why the urinary oxalate levels becoming higher in stone patients after ESWL was unknown, and it needs further evaluation.
參考文獻、
1. Huang HS, Chen CF, Chien CT and Chen J: Possible biphasic changes of free radicals in ethylene glycol-induced nephrolithiasis in rats. Brit J Urol 85(9): 1143-1149, 2000.
2. Huang HS, Ma MC, Chen CF, and Chen J: Changes in the oxidant-antioxidant balance in the kidney of rats with nephrolithiasis induced by ethylene glycol. J Urol, In revision.
3. Thamilselvan S, Hackett RL, Khan SR: Lipid peroxidation in ethylene glycol induced hyperoxaluria and calcium oxalate nephrolithiasis. J Urol
157(3):1059-63, 1997.
4. Gambaro G, Favaro S, D’Angelo A: Risk for renal failure in nephrolithiasis. Am J Kidney Dis 37(2):233-243, 2001.
5. Kamihiara O, Ono Y, Katoh N, Yamada S, Mizutani K, Ohshima S: Long-term stone recurrence rate after extracorporeal shock wave lithotripsy. J Urol
156:1267-1271, 1996.
6. Willians CM, Kaude JV, Newman RC, Peterson JC, Thomas WC: Extracorporeal shock-wave lithotripsy: long term complications. AJR Am J Roentgenol
150:311-315, 1988.
7. Lechevallier E, Siles S, Ortega JC, Coulange C: Comparison by SPECT of renal scars after extracorporeal shock wave lithotripsy and percutaneous
nephrolithotomy. J Endourol 7:465-467, 1993.
8. Evan AP, Willis LR, Connors BA, McAteer JA, Lingeman JE: Renal injury by extracorporeal shock wave lithotripsy. J Endourol 5:25-35, 1991.
9. Willis LR, Evan AP, Connors BA, Blomgren P, Fineberg NS, Lingeman JE: Relationship between kidney size, renal injury, and renal impairment induced by shock wave lithotripsy. J Am Soc Nephrol 10:1753-1762, 1999.
10. Munver R, Delvencchio FC, Kuo RL, et al: In vivo assessment of free radical activity during shock wave lithotripsy using a microdialysis system: the renoprotective action of allopurinol. J Urol 2002 Jan;167(1):327-34.
renal tissues after ESWL: protective effects of antioxidant vitamins. Nephron 1998;79(2):181-5.
12. Sarica K, Kosar A, Yaman O, et al: Evaluation of ischemia after ESWL: detection of free oxygen radical scavenger enzymes in renal parenchyma subjected to high-energy shock waves. Urol Int 1996;57(4):221-3.
13. Strohmaier WL, Lahme S, Weidenbach PM, et al: Reduction of high-energy shock-wave-induced renal tubular injury by selenium. Urol Res 1999 Oct;27(5):382-5.
14. Marzi I, Zhong Z, Zimmerman FA, et al: Xanthine and hypoxanthine accumulation may contribute to reperfusion injury following liver transplantation. Transplant Proc 21:1319-1320, 1989.
15. Jaescke H, Bautista AP, Spolarics Z, Spitzer JJ: Superoxide generation by Kupffer cells and priming of neutrophils during reperfusion after hepatic ischemia. Free Radical Res Commun 15:277-284, 1991.
16. Marubayshi S, Dohi K, Yamada K, Kawasaki T: Changes in the levels of endogenous coenzyme Q10 homologous, α-tocopherol and glutathione in the rat
liver after hepatic ischemia and reperfusion and the effect of pretreatment with coenzyme Q10. Biochim Biophys Acta 797:1-9, 1984.
17. Minakami H, Arai H, Nakano M, et al: A new and suitable reconstructed system for NADPH-dependent microsomal lipid peroxidation. Biochem Biophys Res Commun 153:973-978, 1988.
18. Ruud de W, Noordermeer C, van der Kwast TH, et al: Calcium oxalate
nephrolithiasis: effect of renal crystal deposition on the cellular composition of the renal interstitium. Am J Kidney Disease 33(4): 761-771, 1999.
19. Elferink JGR: The mechanism of calcium oxalate crystal-induced haemolysis of human erythrocytes. Br J Exp Pathol 68:551-557, 1987.
20. Halliwell B: Free radicals, antioxidants and human disease: curiosity, cause or consequence? Lancet 344:721-724, 1994.
21. Evan AP, McAteer JA: Q-effects of shock wave lithotripsy; in Kidney Stones: Medical and Surgical Management, Coe FL, Favus MJ, Pak CYC, Parks JH, Preminger GM (eds): Philadelphia, Lippincott-Raven Press 1996, 549-570.
計畫成果自評部份 因為再申請本研究計畫時, 並沒有說明要先得到”研究倫理委員會審查通過”, 所以,本實驗做到一半時聽到此一消息,才申請在本院的研究倫理委員會審查, 所以影響了一些進度。 這個研究計畫很有意義:此計畫證實了 ESWL 會對腎臟造成傷害,會造成蛋 白尿增加,尿中的過氧化脂質量增加和尿中草酸鹽濃度增加。也會造成血液紅血 球中的 GSH 降低,如此,可能會增加血液中的氧化壓力,雖然血中的白血球製 造自由基的能力並沒有增加。