Referral-free Health Care and Delay in Diagnosis for Lung Cancer Patients
Vivian Chia-Rong Hsieh
1, Trong-Neng Wu
2, Shu-Hui Liu
1,3and Shwn-Huey Shieh
4,5,*Objective: Lung cancer is not only one of the most prevalent cancers but is also a lethal disease with a very low 5-year survival rate. Delay in diagnosis further reduces the chance of early treatment and worsens patients’ survival. The purpose of this study was to understand the delay in the diagnosis of lung cancer under the healthcare system in Taiwan, and to iden- tify the factors associated with it.
Methods: A total of 840 patients diagnosed with lung cancer who had completed or were undergoing cancer treatments were recruited from a medical center in central Taiwan from July 2007 to January 2011. Structured questionnaires were administered regarding demographic characteristics, factors associated with their time to diagnosis and the length of delay in days.
Results: Mean age was 62.68 years with 52.16 days to diagnosis on average. Number of hospital visits before confirmation of diagnosis differed significantly with the level of health- care institution initially visited (P , 0.001). Compared with patients who had three or more hospital visits, patients who only visited two and one hospital(s) had a significant 34.91-day (95% confidence interval: 16.29 – 53.53) and 42.25-day (95% confidence interval: 20.76 – 63.76) reduction in their time to diagnosis (P , 0.001).
Conclusions: As the number of hospital visits increased, the delay in diagnosis also increased. It is vital to shorten the time to diagnosis for lung cancer patients by limiting the number of medical visits and educating the public to restrict excessive use of medical resources and strengthen their trust in medical professionals.
Key words: delay in diagnosis – lung cancer – referral and consultation – hospitals
INTRODUCTION
As of 2010, lung cancer is the second leading cancer for men and the leading type for women. According to the statistics published by the Department of Health, Executive Yuan, Taiwan, 11.9%
(9516/79 818) of cancer cases were diagnosed with lung cancer in 2008 ( 1), and the disease caused a total of 8194 deaths in 2010, accounting for ➇20.0% of all cancer deaths ( 2). Of all cancer deaths, mortality rates for lung
cancer were 20.8 and 18.5% for men and women, respective- ly. Although markedly low, the 5-year survival rate for women (15%) was slightly higher than that for men (10%) ( 3), compared with 5–10% worldwide ( 4). These low survival rates could be potentially due to the inattentiveness toward un-apparent or even asymptomatic signs at an early stage, and delay in diagnosis further reduces the chance of early treat-ment and worsens patients’ survival ( 5– 7).
Prompt diagnosis, together with the advancement in medical treatments, on the parts of both the service providers and patients carry out the potential to significantly improve the survival of these patients. Success of surgical resection, in particular, depends greatly on early diagnosis while the lo- cality of the tumor remains un-metastasized ( 8 – 1 0).
Therefore, delay in the pre-diagnosis process should be ef- fectively minimized. Currently, different definitions and methods for categorizing delayed diagnosis exist. A previous study has divided delayed diagnosis into three segments, namely patient delay, physician delay and system delay.
Patient delay denotes the gap between awareness of symp- toms and initial visit to the primary physician. Physician delay or general practitioner delay, also known as ‘GP delay’, indicates the gap between initial visit to the primary physician and commencing of lung cancer examinations. System delay refers to the period between the lung cancer examinations and treatment, which also involves delays in referral, diagnosis and treatment ( 1 1). Another study referred to delayed diagnosis as a combination of patient delay and provider delay ( 1 2). Provider delay was further divided into diagnosis delay and treatment delay, where the former refers to the period between a patient’s initial visit and diagnosis confirmation, and the latter refers to the period between diagnosis and the start of treatment ( 13 – 1 5). All these defi- nitions, however, were characterized under health systems where referral mechanism exists.
Because the referral system relies heavily on the context- ual framework of a nation’s healthcare service delivery, the ties between delay in diagnosis and patient healthcare- seeking behavior essentially depict the determining factors for survival rates of these cancer patients. Taiwan adopts a single-payer, universal healthcare system, the National Health Insurance (NHI) whose coverage rate currently lies over 99% ( 16). With this healthcare system, people can access any level of healthcare institutions, from primary clinics, district hospitals, regional hospitals, to medical centers at their free will. No restriction is placed on the number and the level of care institution the patient wishes to attend. Treatments for severe disease such as lung cancer and services used in the pre-diagnosis stage are mostly covered by the NHI, but only medical institutions of suffi-cient magnitude could provide such advanced technology such as tumor imaging. Relative differences in co-payment and quality of services, however, still exist across different hospital levels. Hence, patients’
healthcare-seeking behavior can really vary with regard to their physical accessibility to medical services, amount of out- of-pocket payment, self-awareness of the disease condition and symptoms, and their perception of ‘best-suited’
physicians/hospital known to cure the disease. Variation in this behavior inevitably impacts the length of delay incurred in the pre-operative stage of lung cancer patients, and thus, their survival.
Although past research has examined various aspects of delay in diagnosis, most focused on the influence of the primary physician and referral systems of the healthcare
system ( 1
7). This system in Taiwan, however, differs fromthe system of other countries in that insurance beneficiaries have the freedom of choice in seeking medical assistance. This is worthy of investigation to understand the delay in diagnosis of lung cancer under the NHI in Taiwan, and to identify the factors associated with it.
PATIENTS AND METHODS
The study sample recruited 840 patients diagnosed with lung cancer from a medical center in central Taiwan from July 2007 to January 2011. At the time of survey, these patients had either completed or were undergoing cancer treatments.
Consent was obtained from all participants included in the study. A structured questionnaire was used to conduct one- on-one interviews and included items relating to demo-graphic characteristics (age, gender, marital status, educa-tional level and employment status), factors associated with their time to diagnosis (hospital level, examination per-formed on initial visit, number of medical visits before con-firmed diagnosis) and the length of delay in days. All items were answered on a recall basis. To test its validity, the ques-tionnaire was designed and evaluated by five healthcare pro-fessionals specialized in thoracic oncology. The protocol of this study was approved by the Institutional Review Board at the China Medical University Hospital (DMR96-IRB-78).
The four hospital levels were categorized in accordance with NHI’s classification of medical institutions by their ac- creditation criteria. We believe that this parameter reflects patients’ preference and their healthcare-seeking behavior under universal coverage. The type of examination on the initial visit would indicate if relative advancement in medical technology on the provider’s side effectively reduces delay in diagnosis. By studying the number of hos- pital visited before a confirmed diagnosis, the consequence of a deficient referral system as well as the patients’ percep-tion of the hospital and/or their trust toward the service pro-vider would be illustrated. The type of examination upon the initial visit was also analyzed for the reason that the technol-ogy available on the provider’s side that could determine the length of delay in diagnosis.
Currently, delayed diagnosis is being recognized in the international community under the assumption that a referral system and primary physician mechanisms are present in the healthcare systems. It is different in the case of Taiwan where patients can access any level of healthcare institution without requiring referral from a primary physician. For the purpose of this study, ‘delay in diagnosis’ has been defined as the period from a patient’s initial medical visit to any hos-pital to his/her confirmed diagnosis of lung cancer, and has been compared in relative terms with a reference group in our analyses. This period should capture the paths of patients’ healthcare- seeking behavior and delays between visits ( 1
8, 1 9).T a b l e
1 .
D e m o g r a p h i c
c h a r a c t e r i s t i c s ,
d i a g n o s i s
f a c t o r s
of patients and length of delay in diagnosis (N ¼ 840)
Variables n (%) Delay in diagnosis (days) P value Mean SD T (F) value
Gender
Male 469 (55.9) 49 73 1.30 0.195
Female 370 (44.1) 56 80
Age
₃50 124 (18.1) 47 60 0.89 0.472
51–60 169 (24.7) 55 83
61–70 176 (25.7) 53 84
71–80 168 (24.5) 42 61
.80 48 (7.0) 41 53
Educational attainment
,Elementary 98 (11.7) 51 68 0.72 0.576
Elementary 326 (38.9) 58 81
Junior high school 103 (12.3) 44 76 Senior high school 169 (20.1) 48 76
₃College 143 (17.0) 54 76
Marital status
Single 22 (2.6) 42 77 0.86 0.461
Married 791 (94.8) 51 74
Divorced/separated 5 (1.9) 93 153
Widowed 16 (0.6) 66 101
Profession
Civil service 32 (3.9) 46 68 1.33 0.207
Education 14 (1.7) 83 127
Labor 64 (7.6) 51 74
Business 110 (13.4) 46 70
Agriculture 70 (8.5) 49 60
Housekeeping 169 (20.6) 55 76
Retired 148 (18.0) 52 88
None 213 (26.0) 51 109
Hospital level on initial visit
Medical center 376 (44.8) 46 73 2.86 0.036 Regional hospital 241 (28.7) 55 80
District hospital 149 (17.7) 50 69
Clinic 74 (8.8) 74 99
Number of hospitals before confirmed diagnosis
1 299 (35.6) 43 68 11.9 ,0.001
2 463 (55.1) 52 76
₃3 78 (9.3) 90 104
Examination on initial visit
None 50 (6.1) 62 82 3.71 0.011
X-ray 247 (30.0) 58 79
X-ray þ CT 527 (64.0) 47 73
Continued
Jpn J Clin Oncol 2012 Page 3 of 6
Table 1. Continued
Variables n (%) Delay in diagnosis (days) P value Mean SD T (F) value
Stage
1 229 (29.1) 51 79 0.87 0.461
2 46 (5.8) 39 62
3 197 (25.0) 48 68
4 316 (40.1) 56 81
SD, standard deviation; CT, computed tomography.
Mean age: 62.68 years. Mean of diagnosis delay: 52.16 days.
Descriptive analyses were used to describe patients’
demo-graphic profile, factors associated with their delay in diagno-sis, and the length of their delay before confirmed diagnosis. T-tests and one-way analysis of variance were performed to test the differences between groups and their mean delay. The highest level of healthcare institution referred to medical centers, followed by levels of regional hospitals, district hospitals and local clinics. Multiple regression ana-lysis was finally conducted to predict key factors affecting the delay in lung cancer diagnosis with consideration of other covariates. All statistical analyses were performed using SAS software, version 9.2 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Demographic characteristics of the study participants were shown in Table 1. Mean age was 62.68 years with 52.16 days to diagnosis on average for the studied subjects. More males (55.90%) were recruited than females (44.10%), with the majority of patients being married (94.84%), belonging to the 61 – 70 years age group (25.69%), or having obtained an elementary school degree (38.89%). Women generally experienced a longer delay in diagnosis (56 days) compared with men (49 days). Patients of 51 – 60 years of age experi- enced the longest time to diagnosis (55 days) among all age groups. Patients whose highest level of education was elem- entary school experienced longest delay in diagnosis (58 days) among all education groups. However, patients who were divorced or separated had the overall longest delay in diagnosis (93 days) in the univariate analysis. Regarding em- ployment status, the largest group consisted of participants who were unemployed (25.98%), followed by the partici-pants working as housekeepers (20.61%) and retirees (18.05%).
Patients working in the education discipline had the longest mean time to diagnosis of 83 days. No significant relationship, however, was found between patient demo-graphics (gender, age, marital status, education level and
employment status) and the number of days until diagnosis (P . 0.05).
Table 1 identified the significant factors related to medical visits before diagnosis: service level (P ¼ 0.036) and exam- ination type on initial visit (P ¼ 0.011), and total number of service visits prior to a confirmed diagnosis (P , 0.001). It was only 43 days before diagnosis was confirmed for those who made only one medical visit. For those who visited the medical center on their first service visit, the mean time to diagnosis was 46 days. We further observed the absence of a statistically significant difference between different stages of lung cancer and diagnostic delay (P ¼ 0.461).
Cross-tabulated results in Table 2 showed that the number of hospitals visited before a confirmed diagnosis was in asso- ciation with the hospital level upon the first medical visit made by these patients. Nearly 65% of patients made more than one medical visit. Among those who only made one total visit, 87.29% visited a medical center on their initial visit, whereas of those who made three or more visits, only 14.10% visited a medical center on their initial visit. The number of hospital visits before confirmation of diagnosis differed significantly with the level of healthcare institution initially visited (P , 0.001) (Table 2).
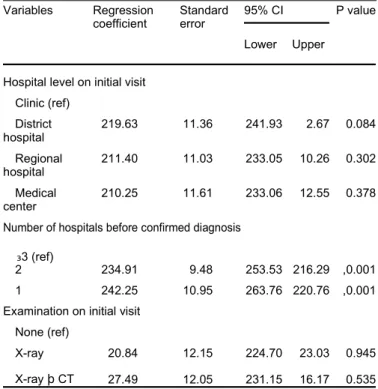
Multiple regression analysis was performed to predict the key factors associated with the delay in diagnosis. Compared with patients who had three or more hospital visits (reference group), patients who only visited two and one hospital(s) had a significant 34.91-day [95% confidence interval (CI): 16.29 – 53.53] and 42.25-day (95% CI: 20.76 – 63.76) reduc-tions in their time to diagnosis (P , 0.001) (Table 3).
Regarding the variable ‘the level of the healthcare institu- tion a patient initially visited’, when ‘general clinic’ was used as reference, patients who visited a medical center, re-gional hospital and district hospital on their initial visit experienced a statistically insignificant reduction of 10.25,
Table 2. Service level at initial medical visit and total number of hospitals visited prior to diagnosis
Number of hospitals before Total P value confirmed diagnosis
1 2 ₃3
n (%) n (%) n (%)
Hospital level on initial visit ,0.001
Medical center 261 (87.29) 104 (22.46) 11 (14.10) 376 Regional hospital 13 (4.35) 201 (43.41) 27 (34.62) 241 District hospital 13 (4.35) 116 (25.05) 20 (25.64) 149 Clinic 12 (4.01) 42 (9.07) 20 (25.64) 74 Total 299 (35.60) 463 (55.12) 78 (9.29)
There was a sum of 766 (91.19%) of subjects (n ¼ 840) who had initial visits to hospital level services (i.e. 376 þ 241 þ 149).
11.40 and 19.63 days in their time before diagnosis, respect-ively. Patients who received an X-ray together with computer tomography (CT) scan on the initial visit experienced a re-duction of 7.49 days, although not statistically significant, in the delay in diagnosis (P ¼ 0.535). For patients who received only an X-ray on the first visit had a reduction of 0.84 days (P ¼ 0.945).
DISCUSSION
The data presented here show that the greatest reduction in time to diagnosis was observed when the patient only visited one hospital before diagnosis after adjusting for effects of service level and examination type on the initial visit. Although the choice of hospital level at the first medical at-tendance appeared to be an important factor, its effect was rendered insignificant in the final analysis after adjusting all factors related to medical visits before diagnosis.
To our knowledge, this is the first study to evaluate the factors associated with absolute time to diagnosis as well as relative delay in diagnosis in consideration of numerous pre- dictors from the standpoint of the lung cancer patients under a referral-free healthcare system. We investigated the number and level of healthcare institutions a patient visited before a confirmed diagnosis and the type of examination given in re- sponse to their visit. Average GP delay and specialist delay for diagnosing lung cancer in the UK was 32 (symptom to Table 3. Multivariable regression analysis between diagnosis factors and days of delay in diagnosis
Variables Regression Standard 95% CI P value
coefficient error
Lower Upper
Hospital level on initial visit Clinic (ref)
District 219.63 11.36 241.93 2.67 0.084
hospital
Regional 211.40 11.03 233.05 10.26 0.302
hospital
Medical 210.25 11.61 233.06 12.55 0.378
center
Number of hospitals before confirmed diagnosis
₃3 (ref)
2 234.91 9.48 253.53 216.29 ,0.001
1 242.25 10.95 263.76 220.76 ,0.001
Examination on initial visit None (ref)
X-ray 20.84 12.15 224.70 23.03 0.945
X-ray þ CT 27.49 12.05 231.15 16.17 0.535
CI, confidence interval.
N ¼ 824.
chest physical referral) and 82 (chest physician referral to operation) days, respectively ( 1 0). Compared with 52.16 days observed in our study, which consisted of the additional delay potentially caused by making more than one medical visit before diagnosis, the length of delay is seem-ingly short in the absence of a regular referral mechanism. Another study using survey results of the National Health Service indicated a 33.1- and 12.6-day delay in average GP delay and secondary care delay, respectively—exclusive of a mean 51.8-day patient and primary care delay ( 1 7). Two Scandinavian studies conducted revealed that the lag between the initial visit to the GP and diagnosis confirmation among patients with lung cancer was 88 and 97 days, respectively ( 2 0, 2 1). While most studies found a delay relatively longer than what we have identified, a Turkish study reported that the average delay in a diagnosis for lung cancer was just 41 days ( 1 8). Because the countries that have been investigated are very distinct not only in their healthcare systems, but also very much in their cultural and local contexts, we believe further examination into their health service delivery and healthcare-seeking behavior is worthwhile.
In Taiwan, there is no referral system based on the primary physician mechanism, which means that people can access any healthcare institution to obtain opinions from dif-ferent physicians without a referral from their primary care physician.
With such a critical disease like lung cancer, patients’ limited knowledge of the disease or skepticism about the physician at their initial visit tempted them to seek second opinions at other hospitals or higher-level healthcare institutions. Therefore, the period between a patient’s initial visit and the diagnosis confirmation does not necessarily involve delay due to referrals, although in most highly sus-pected cases, clinic or district hospital physicians would still refer them to larger facilities like regional hospitals or medical centers. For this reason, we believe this is why the delay in diagnosis may be prolonged because of this ‘phys-ician shopping’ behavior.
Most of the patients in this study visited two or more hospitals before a confirmation of their diagnosis. As the number of hospital visits increased, the delay in diagnosis also increased.
From how this study was designed, we could not directly relate the delay in diagnosis to patient survival. We also could not precisely estimate the ‘safe’ window of this dur-ation for lung cancer patients to have a favorable prognosis as it would require more detailed description on the hist-ology and location of the tumor. What we have identified, however, were possible factors that could prolong this delay in the current health system. Among those that only visited once, the greatest reduction in time to diagnosis was observed. In addition, most recruited patients who only made one medical visit before diagnosis chose to visit the highest-level medical centers. This is a mere representation of the current health- seeking situation for patients in Taiwan in which they seek technological advancement with heigh-tened expectations—
one phenomenon greatly aggravated
first by having as many as four medical centers in the 20 km-radius vicinity of central Taiwan, and second, by the NHI as it attempts to reduce cost by waiving the registration fee for multiple visits in the same institution, which is most likely to be medical centers with multiple disciplinary prac-tices and advanced medical imaging technologies like the chest CT. Therefore, patients with lung-cancer-like symp-toms would most likely visit medical centers, unless they were initially unaware of their condition or they reside in more remote areas where access to local clinics and district hospitals are more likely.
This, however, does not suggest that the first medical visit to medical centers may be the most cost-effective measure for the patient and the NHI. Registration fees (compulsory copayment made on each medical visit: $210 New Taiwan Dollars (NTD; $29.8NTD ¼ $1US year 2010) for a visit to medical center and $140NTD for regional hospital) and the cost of a CT scan are higher than an X-ray. Since we did not recruit non-lung cancer patients, we could not estimate the amount of costs incurred for those non-cases who visited a medical center on initial visit with suspected lung cancer symptoms. There should be a balance between costs spent and the outcome gained from reduction in time to diagnosis.
On the other hand, of those who attended three or more medical services prior to diagnosis, the majority picked re- gional or district hospitals first. This implies that without the presence of a referral system, lung cancer patients who visited local clinics or district hospitals on their first medical visit would likely be paying two or more medical visits before a confirmation of their diagnosis. Even so, there were a considerable proportion of participants who sought two or more medical visits subsequent to their initial visit to a medical center.
This study only recruited lung cancer patients from a medical center in central Taiwan, an area containing ➇4 million people. To collect data, this study requested patients to recall their diagnosis process. Hence, the presence of recall bias regarding the dates of hospital visits is likely. Patients may not be aware of the level of the healthcare insti-tution of their initial visit, leading to a bias in classification. One other limitation in this study was that it did not consider patients’
initial symptoms. More serious symptoms, such as weight loss or hemoptysis, may be more likely to prompt further investigation of the disease. Factors concerning service providers, such as a physician’s seniority and experi-ence on interpretation of a chest CT scan, can also affect their diagnosis of lung cancer and the length of delay. Future studies could look into incorporating these factors for a more extensive examination.
It appears that the foremost goal to shorten time to diag- nosis for lung cancer patients may be to reduce the number of medical visits and that these visits do not necessarily need to be at medical centers, given the current diagnostic standard in the country. We need to educate the public through community action to prevent excessive use of medical resources and heighten their trust in today’s medical
professionals. Moreover, we should shift our focus toward disease prevention. The NHI program has been implemented for 17 years in Taiwan, and the associated healthcare system is relatively stable and mature. Patients are highly satisfied with the program and its progress since its inauguration ( 2 2).
Nevertheless, the number of patients diagnosed with lung cancer is increasing in Taiwan and its health system is still focused on disease treatment, rather than disease prevention and early detection ( 2 2).
We hope through findings of this study, factors associated with the delay in diagnosis for lung cancer patients could be depicted. This is to thoroughly understand the influences on lung cancer diagnosis by patients’ health-seeking behavior and diagnosis capabilities of healthcare institutions at different levels in the NHI envir-onment without a referral mechanism.
CONCLUSION
This study highlighted that without a referral mechanism, the ‘physician shopping’ behavior of patients with cancer further delays the diagnosis. More hospital visits before diagnosis is confirmed to lead to a longer delay in diagnosis, which reduces the chances of early treatment and survival. Although the NHI program enables people to receive health-care services under a comprehensive healthcare delivery system, excessive hospital visits for lung cancer not only wastes medical resources, but also leads to a longer delay in diagnosis, minimizing the chance of early treatment. This study reminds the public of the symptoms of early-stage lung cancer and provides health education.
References
1. Bureau of Health Promotion. 2008 Cancer Registry Report. Department of Health; 2011.
2. Department of Health. 2010 Statistics of Causes of Death. 2011.
3.Taiwan Cancer Registry. Five-Year Relative Survival of Cancer. 2011.
4. Moody A, Muers M, Forman D. Delays in managing lung cancer. Thorax 2004;59:1–3.
5. Bozcuk H, Martin C. Does treatment delay affect survival in non-small cell lung cancer? A retrospective analysis
from a single UK centre. Lung Cancer 2001;34:243–52.
6. Loh LC, Chan LY, Tan RY, et al. Effect of time delay on survival in patients with non-small cell lung cancer—a
Malaysian study. Asia Pac J Public Health 2006;18:69–71.
7. Porta M, Gallen M, Malats N, Planas J. Influence of "diagnostic delay" upon cancer survival: an analysis of five
tumour sites. J Epidemiol Community Health. 1991;45:225–30.
8. Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors,
treatment, and survivorship. Mayo Clin Proc 2008;83:584–94.
9. Schwartz AM, Henson DE. Diagnostic surgical pathology in lung cancer: ACCP evidence-based clinical practice
guidelines (2nd edition). Chest 2007;132(3 Suppl):78S–93S.
10. Billing JS, Wells FC. Delays in the diagnosis and surgical treatment of lung cancer. Thorax 1996;51:903–6.
11. Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. Br J Cancer 2009;101(Suppl
2):S5–8.
12. Unger-Saldana K, Infante-Castaneda C. Delay of medical care for symptomatic breast cancer: a literature review.
Salud Publica Mex 2009;51(Suppl 2):s270–85.
13. Barber MD, Jack W, Dixon JM. Diagnostic delay in breast cancer. Br J Surg 2004;91:49–53.
14.Caplan LS, May DS, Richardson LC. Time to diagnosis and treatment of breast cancer: results from the National Breast and
Cervical Cancer Early Detection Program, 1991–1995. Am J Public Health 2000;90:130–4.
15. Gwyn K, Bondy ML, Cohen DS, et al. Racial differences in diagnosis, treatment, and clinical delays in a population-
based study of patients with newly diagnosed breast carcinoma. Cancer 2004;100:1595–604.
16. National Health Research Institutes [Internet]. National Health Insurance Research Database: introduction;
[updated 25 February 2009; cited 11 November 2011]. Available from: http://w3.nhri.org.tw/nhird/ en/index.htm.
17. Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS
Patients: Cancer. Br J Cancer 2005;92:1959–70.
18. Annakkaya AN, Arbak P, Balbay O, Bilgin C, Erbas M, Bulut I. Effect of symptom-to-treatment interval on
prognosis in lung cancer. Tumori 2007;93:61–7.
19. Wang J, Liu F, Gao H, et al. The symptom-to-treatment delay and stage at the time of treatment in cancer of
esophagus. Jpn J Clin Oncol 2008;38:87–91.
20. Koyi H, Hillerdal G, Branden E. Patient’s and doctors’ delays in the diagnosis of chest tumors. Lung Cancer
2002;35:53–7.
21. Mansson J, Bengtsson C. Pulmonary cancer from the general practitioner’s point of view. Experience from the health
centre area of Kungsbacka, Sweden. Scand J Prim Health Care 1994;12:39–43.
22. National Health Insurance. Stauts Comparsion Between National Health Insurance and International Health Care
Service System. Taipei, Taiwan: Department of Health.