Elsevier Editorial System(tm) for Journal of the American Medical Directors Association Manuscript Draft
Manuscript Number:
Title: Work autonomy of certified nursing assistants in long-term care facilities: Discrepant perceptions between nursing supervisors and certified nursing assistants
Article Type: Long-Term Care around the Globe Keywords: role, quality of job, task identity, delegation. Corresponding Author: Dr Li-Fan Liu,
Corresponding Author's Institution: First Author: Li-Fan Liu
Order of Authors: Li-Fan Liu; Wei-Pei Liu; Jong-Yi Wang
Abstract: Objective: Despite increasing demand of certified nursing assistants (CNAs) in long-term care (LTC) facilities, their work autonomy delegated by nursing supervisors remained ambiguous and varied. This study investigates the CNAs' role in LTC facilities by examining their task identities and the degrees of work autonomy from the perspectives of nursing supervisors and CNAs. Whether the characteristics and staffing level of institutions affected the CNAs' work autonomy and delegations was also examined.
Method: A stratified random sampling method was used to sample LTC facilities in Taiwan.
A self-administered structured questionnaire was answered by senior nursing supervisor and CNA in each sampled institution for their perception of work autonomy in the five main aspects of CNAs' job contents: personal care, affiliated nursing care, auxiliary medical service, social care, and
administration services. Student t-test and general linear models (GLM) were used to test the mean differences of CNAs' work autonomy and their relationship with the institutions' characteristics. Results: Both nursing supervisors and CNAs rated the highest scores of work autonomy in the aspect of personal care, and the lowest scores in the aspect of affiliated nursing care. However, the nursing supervisors expected higher work autonomy of CNAs on the work items in affiliated nursing care and auxiliary medical services than did the CNAs (p<0.05). The institutional-level factors were significantly associated with perceptions of nursing supervisors toward CNAs' work autonomy. The types, sizes (capacity), occupancy rates, CNA staff numbers of the long-term care facilities, and resident numbers were related to the CNAs' work autonomy as perceived by their nursing supervisors. No difference among the aspects of the administration activities and the social care was seen.
Conclusions: There are discordance views towards CNAs' work autonomy both in nursing supervisors and CNAs across different settings in LTC institutions. A consistent good nursing supervision in terms of CNAs' job delegation by nursing supervisors could help with reducing CNAs' role ambiguity and their task identity, and further to enhance their job satisfaction. Clear and mandated regulation of CNAs job contents is needed for their work identity and autonomy to improve the quality of care in LTC facilities.
Institute of Gerontology,
College of Medicine,
National Cheng Kung University
Li-Fan Liu,PhD.Assistant Professor, TEL: +886-6-3028173
Institute of Gerontology, FAX: +886-6-3028173
No. 1, University Road, 70428, EMAIL: lilian@mail.ncku.edu.tw Tainan, TAIWAN
Dear editor:
We submit the enclosed manuscript (attached file), titled as " Work Autonomy of Certified Nursing Assistants in Long-term Care Facilities: Discrepant
Perceptions between Nursing Supervisors and Certified Nursing Assistants” for the consideration to be published in your distinguished Journal. In this origin study, we have investigated the controversial issue of task identity and work autonomy in the job contents of certified nursing assistants in different types of long-term care
facilities from the perspectives of nursing supervisors and CNAs. We have found there are discrepant perceptions between nursing supervisors and certified nursing assistants regarding the work autonomy of CANs’ job content which may have impact on the quality of care in long-term care facilities. We think this important information may be interesting to your readers of policy makers as well as related research
scientists in the field of long term care study. All authors have read the manuscript and approve its submission. The material of this study is original and has not been
submitted for publication elsewhere.
Your favorable consideration is greatly appreciated and we look forward to your prompt reply with valuable reviews and comments.
Sincerely yours, Li-Fan Liu, PhD.
Assistant Professor of Gerontology, National Cheng Kung University
1, University Road, Tainan, Taiwan 70428, R.O.C Tel: (886)-6-302-8173 Fax: (886)-6-302-8173 E-mail: lilian@mail.ncku.edu.tw.
Cover Letter
Work autonomy of certified nursing assistants in long-term care
facilities: Discrepant perceptions between nursing supervisors and
certified nursing assistants
Li-Fan Liu1, § , Wei-Pei Liu2,Jong-Yi Wang2
1
Institute of Gerontology, College of Medicine, National Cheng Kung University, Tainan;
2
Department of Health Services Administration, China Medical University, Taichung, TAIWAN.
Running Title: Work autonomy of CNA in LTC facilities
§Corresponding author
Li-Fan Liu, PhD
Institute of Gerontology, College of Medicine, National Cheng Kung University, No. 1, University Road, Tainan, 704, TAIWAN.
Email addresses: lilian@mail.ncku.edu.tw,
Key words: role, quality of job, task identity, delegation.
Work autonomy of certified nursing assistants in long-term care facilities:
Discrepant perceptions between nursing supervisors and certified nursing
assistants
Running Title: Work autonomy of CNA in LTC facilities
Key words: role, quality of job, task identity, delegation.
Abstract
Objective: Despite increasing demand of certified nursing assistants (CNAs) in long-term
care (LTC) facilities, their work autonomy delegated by nursing supervisors remained
ambiguous and varied. This study investigates the CNAs’ role in LTC facilities by examining their task identities and the degrees of work autonomy from the perspectives of nursing supervisors and CNAs. Whether the characteristics and staffing level of institutions affected the CNAs’ work autonomy and delegations was also examined.
Method: A stratified random sampling method was used to sample LTC facilities in Taiwan.
A self-administered structured questionnaire was answered by senior nursing supervisor and CNA in each sampled institution for their perception of work autonomy in the five main aspects of CNAs’ job contents: personal care, affiliated nursing care, auxiliary medical
service, social care, and administration services. Student t-test and general linear models (GLM) were used to test the mean differences of CNAs’ work autonomy and their relationship with the institutions’ characteristics.
Results: Both nursing supervisors and CNAs rated the highest scores of work autonomy in
the aspect of personal care, and the lowest scores in the aspect of affiliated nursing care. However, the nursing supervisors expected higher work autonomy of CNAs on the work items in affiliated nursing care and auxiliary medical services than did the CNAs (p<0.05). The institutional-level factors were significantly associated with perceptions of nursing
supervisors toward CNAs’ work autonomy. The types, sizes (capacity), occupancy rates, CNA staff numbers of the long-term care facilities, and resident numbers were related to the CNAs’ work autonomy as perceived by their nursing supervisors. No difference among the
aspects of the administration activities and the social care was seen.
Conclusions: There are discordance views towards CNAs’ work autonomy both in nursing
supervisors and CNAs across different settings in LTC institutions. A consistent good nursing supervision in terms of CNAs’ job delegation by nursing supervisors could help with
reducing CNAs’ role ambiguity and their task identity, and further to enhance their job
satisfaction. Clear and mandated regulation of CNAs job contents is needed for their work identity and autonomy to improve the quality of care in LTC facilities.
Introduction
The increasing needs of CNAs and their role in LTC facilities
With the population ageing and the needs of long-term care (LTC) sharply increasing, there has been a corresponding increase in demand for certified nursing assistants (CNAs), who are the most prevalent caregivers in LTC institutions and form the centerpiece of the formal LTC system [1, 2]. In Taiwan, as in other countries, CNAs provide 80-90% of direct resident care for older people in a variety of care settings [3, 4]. The role of CNAs in LTC facilities has been emphasized in previous studies [5-7]. Traditionally, they have been regarded as performing less skilled and non-clinical task-oriented work, reporting to their assigned registered nurses. Since CNAs provide the “high touch” that is essential to the quality of care for elders and chronically disabled individuals [2], they are therefore expected to develop ongoing relationships with the residents and treat them in a positive, caring way [8].
On the other hand, the changes in care delivery models have left registered nurses (RNs) with less and less time for direct care. As long term care becomes more complex, RNs are now performing the indirect role of coordinating and planning the patient care process, which will increasingly rely on CNAs to provide direct care to residents and even some of the nursing functions in LTC facilities [9]. These increasing needs of CNAs in the daily health care delivery of LTC facilities has also increasing the possible conflict of perception
regarding CNAs work contents and autonomy, not just among RNs but also CNAs themselves.
The conflicting perception of CNAs’ role in LTC facilities
Studies revealed several factors that might result in conflicting perceptions of the CNAs’ role among RNs. Perry et al. [10] reported that RNs have difficulty in defining and limiting CNAs’ roles because they have an all-embracing role, doing everything and anything within the LTC facilities. By contrast, CNAs define their role in terms of what they are not allowed to do. Previous literature suggests that a lack of role clarification was evident and differences emerged between the views of CNAs and RNs regarding the positions of CNAs in the care process [5]. This situation might be also driven by the change of health care economics, for example, reducing subsidies or insurance coverage, which pressure LTC institutions to minimize the staffing level, rethink substitute/alternative workforce, and increase workloads for CNAs.
The retention and job satisfaction of CNAs and their quality of care
The high turnover rate of CNAs in the LTC market makes the issue more critical.
Although resulting from a variety of factors, it has been mainly related to their current quality of jobs (including wages, benefits, workloads, role ambiguity, and career opportunities) that
could negatively affect the quality of services delivered and the quality of life provided in LTC facilities [1, 11-13]. Research in Canada found that, from the perspective of job dimensions, staffs in LTC institutions were least satisfied with their task identity, and
indicated that the job dimensions of skill variety, task significance, autonomy, and feedback have been considered highly important for the general satisfaction of personnel who provide nursing and auxiliary nursing care activities [14]. In the US, Tylor et al. [9] found that the CNAs’ work autonomy, together with task identity and intrinsic feedback, would influence
their job satisfaction. These job characteristics (i.e., skill variety, task identity, task
significance, autonomy, and intrinsic feedback), formed the job design and through which influences employee performance [15].
The issues of task identity and work autonomy of CNAs’ job contents
Task identity identifies the degree to which the job allows completion of a whole and identifiable piece of work. In contrast, work autonomy has been conceptualized in various ways. It generallyrefers to the degree to which the job provides independence and discretion in scheduling the work and determining ways to carry it out [15]. It has also denoted other work experiences that may be implied by “occupational self-direction”, e.g., the
decision-making latitude and the amount of innovative thinking required by the job, indicating the freedom granted in performing one's job [16]. Since the CNAs’ role in LTC
institutions has grown increasingly important due to multiple factors, the conflicting perceptions of their role as viewed by RNs could interactively influence the CNAs’ task identity and work autonomy in LTC institutions. This issue is also important for the quality of care provided by CNAs in LTC facilities; however, it has not been extensively studied in Taiwan.
Driven by the increasing need and high turnover of CNAs in Taiwan and other parts of the world, this research focused on the issue of CNAs’ role clarification in LTC facilities, and explored the perceptions and the extent of their work autonomy in various institutions from the perspectives of nursing supervisors and CNAs. We believe these results would add knowledge to the role clarification of CNAs, and then in turn influence both job quality of CNAs and RNs as well as the quality of care they provide in LTC settings.
Methods
This is a cross-sectional exploratory study design. A stratified random sampling method was used. Fifty percent (683 institutions) of three types of LTC institutions (nursing homes, residential care homes, and veterans’ homes) in Taiwan were first randomly sampled, followed by the number of beds of sampled institutions as secondary strata. Since the aim was to investigate the views of nursing supervisors and CNAs in each sampled institution,
one representative senior nursing supervisor and one senior CNA in each sampled institution were identified based on their years of service (the longest), and asking their participation in answering a self-administered structured questionnaire, respectively.
The questionnaire included five main aspects of CNAs’ job contents. The aspect of personal care included 31 work items categorized into 5 categories of oral feeding, urinary and bowel elimination, housekeeping (e.g., personal cloth & linen laundry), oral hygiene and bathing, assisting with moving, positioning, and daily activity. The aspect of affiliated
nursing care had 43 items classified into 7 categories, as tubing care, wound dressing, helping residents take medicine, helping the nurse to perform an injection, measurements of vital signs, basic restorative care, and answering inquires about the residents’ health condition. The aspect of administration services consisted of 19 items divided into the 4 categories of
environment maintenance, helping the nurse to perform administrative work, communication with the residents’ family members, participating in case discussion, and helping to plan and perform the daily activities. The aspect of auxiliary medical services consisted of 6 items including liaisons with medical facilities, escorting the patients for scheduled or unscheduled out-patient visits, escorting the resident to emergency room/or to admission into hospital, helping the physician to examined the residents, helping to arrange physician clinical rounds in LTC facilities. The aspect of social care contained the 13 items including routine telephone contact with the residents’ families, routine home visits to the residents’ families, chatting
with residents, listening to residents’ complaints, helping residents to contact their families,
helping the residents with letter writing, help the residents to make telephone calls, help the residents with outdoor activities, and assisting with daily grocery shopping and other chores.
The questionnaire was designed in which CNAs’ work contents were identified and the researchers designed the questionnaire based on previous research reports in Taiwan and other part of the world [17, 18]. The sampled nursing supervisors and CNAs were asked to answer the questions about their perceptions towards the issues of role boundary, task identity, and the extent of work autonomy of CNAs in their institutions by examining the mean score of work autonomy in CNAs’ work contents as well as other open-ended questions. The response score of work autonomy was designed by using four point scale: 1=CNAs were not allowed to work independently; 2=CNAs were allowed to work with nurse professionals under supervision; 3=CNAs could work independently after training and delegation of tasks by nurse professionals; 4=CNAs could work independently. The questionnaire included five main aspects, 16 categories, and 112 work items in total. It had been piloted before the main study for expert validity and had high internal consistency (Cronbach’s α=0.81).
The main study was conducted for four months in 2007. In total, valid 163
self-administrative questionnaires from nursing supervisors and 165 from senior CNAs from 163 LTC facilities were collected. Regarding the sample representatives, no difference in geographical distribution of long-term care institutions (p=0.1123) between samples and the
study population in Taiwan was found. The response rate of sampled institutions that agreed to participate was 48%, including 60 nursing homes, 99 residential care homes, and 4 veterans’ homes.
The collected data were analyzed by using SPSS 15.0 version. The statistical methods of coefficients of variation (CV), t-test, ANOVA, and general linear models (GLM) with the post hoc test (Searle, Speed, & Milliken, 1980) were used to test the mean differences of response scores according to the characteristics of independent variables (unbalanced cells are due to different numbers in each variable) and the dependent variable as continuous interval.
Results
The characteristics of sampled institutions and its demand and supply
There were 163 sampled institutions composed of registered residential care homes (60.7%, n=99), authorized by Ministry of Interiors (MOI), registered nursing homes (36.8%, n= 60) under the Department of Health (DOH), and also the veterans’ homes under the Council of Veteran’s Administration (2.5%. n= 4). Among them, 79.1% were freestanding homes and 20.9% were hospital-based institutions, of which nursing homes were mainly hospital-based (56.9%), and the residential care homes were mainly freestanding types of homes (93.4%). There were 55.9% sampled institutions whose occupancy rates were over 90%. Regarding the
size of the sample homes, nearly half of the responding nursing homes were ranged from 50 to 99 beds (44.8%), and the residential care homes mainly had beds under 50 (78.7%). More than half (55.9%) of the 163 homes had been registered over 5 years when the survey was conducted.
According to the survey conducted by MOI [19], the supply of LTC institutions in Taiwan was approximately 371 beds per 10,000 elderly people, and the lowest rate was 111 beds (in islands counties). In this research, nearly sixty percent of the sampled institutions were located in the counties with an abundant supply (> 371 beds per 10,000 elderly people) of LTC beds (98 homes) and only 4.3% (7 homes) were located in an area with a relative shortage of institutional care as defined by the government in the Ten Year Long-Term Care Plan [19].
The characteristics of nursing supervisors and CNAs
The workforce allocation of CNA to resident ratio varied from 1:5 in nursing homes, 1: 8 in residential care homes, and 1:20 in veterans’ homes due to the different regulations for the respective types of LTC facilities in Taiwan. In our sampled LTC institutions, nearly 31% of the sampled homes who had full time CNA workers less than six persons and about 40% of the sampled homes hired part-time CNAs. The average annual turnover of CNAs in sampled homes was 13%. Most of the CNAs were women (97.6%), married (89.3%), and
above 30 years old with primarily a senior high school education level (40%). The work experiences of investigated CNAs ranged from 1 to 3 years, and in general the CNAs working in nursing homes were older and more experienced than those in residential care homes. Regarding the characteristics of sampled nursing supervisors, more than 75% of them have held the same position for more than 6 years; more than 80% of them have at least a college degree. In this research, the work experience of nursing supervisors in sampled nursing homes was longer than those who work in sampled residential care homes, while most of the nursing supervisors in residential care home have a higher education level on average.
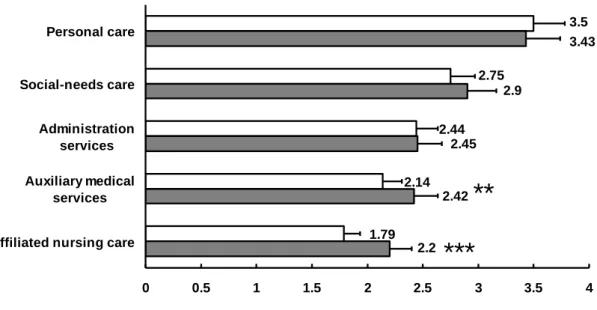
The nursing supervisors’ views toward the extent of work autonomy in CNAs’ job contents
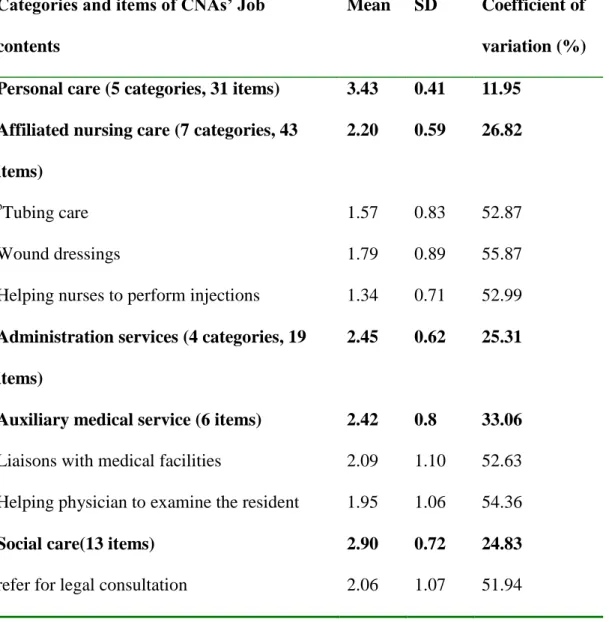
As viewed from nursing supervisor, the aspect of personal care was given the highest independence score (3.43 ± 0.46), followed by social care (2.90 ± 0.73), administration services (2.45± 0.62), and auxiliary medical services (2.42 ± 0.79), while affiliated nursing care received the lowest mean score (2.20 ± 0.59). It was found no statistically significant differences on the mean scores of each aspect between nursing supervisors from various types of homes (p>0.05). To examine the degree of consensus regarding the work autonomy of CNAs among responding nursing supervisors, Table 1 shows the details of the work subcategories and items with the coefficient of variation more than 50% of its mean scores
(suggesting discordance of consensus). Although nursing supervisors have an overall consensus on each aspect of CNA job contents, 23 work items (23/112, 20.5%) have variations over 50%. Among them, the aspect of nursing care accounted for as many as 15 work items (15/43, 34.9%), 5 items on the aspect of administration services (5/19, 26.3%), 2 items on auxiliary medical service (2/6, 33%), and 1 item on the aspect of social care (1/13, 7.69%). These results demonstrated discordance of consensus regarding the work autonomy of CNAs among the responding nursing supervisors, particularly on the aspect of nursing care, including tubing care, wound dressing, and helping nurses with injections. In the open-ended questions, most of the nursing supervisors believed that CNAs were their assistants and could help with almost everything they needed.However, in terms of job contents, their main concerns were particularly on the communication skills of CNAs with other health
professionals and the residents’ families in the caring process. Nursing supervisors expressed that the caring responsibilities were still theirs.
The CNAs’ views toward the extent of work autonomy in their job contents
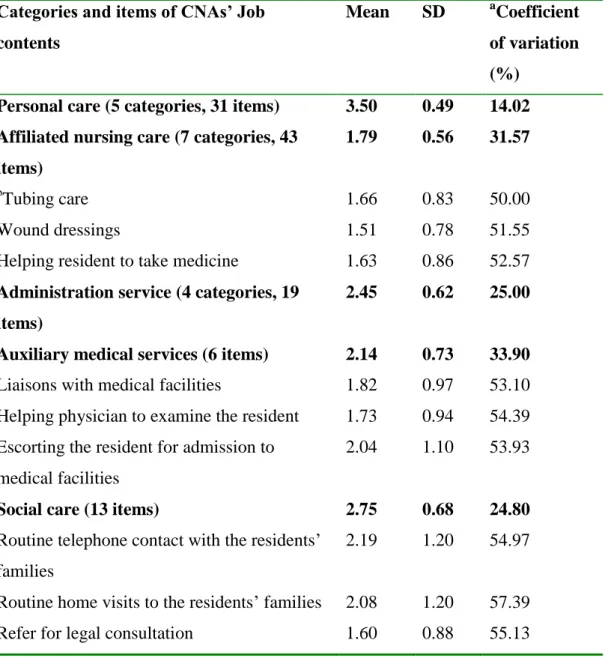
From the views of CNAs, they also rated aspect of personal care the highest independence score (3.50 + 0.49), followed by social care (2.75 + 0.68), administration services (2.45 + 0.62), and auxiliary medical services (2.14 + 0.73), while the affliated nursing care received the lowest mean score (1.79 + 0.56). Table 2 lists the details of the
subcategories in each aspect of CNAs work contents that has a coefficient of variation over 50% of its mean scores. From the perspective of CNAs, these results revealed that several work contents of CNAs were ambiguous in terms of work autonomy, which may influence their task identity and work autonomy of their daily work in LTC facilities. In the open-ended questions, they also expressed the importance of on-job-training, especially for the skilled task if they need to help with.
The discrepancy regarding work autonomy on CNAs’ job contents between nursing
supervisors and CNAs
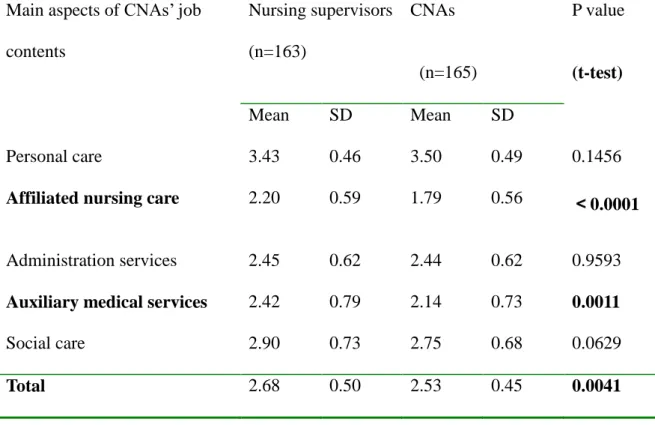
Figure 1 shows the mean scores of work autonomy in each aspect of CNAs’ job contents as answered by the nursing supervisors and CNAs. The ranking work autonomy in these five aspects of CNA work was similar between the CNAs and nursing supervisors. Personal care has the highest level of work autonomy, followed by social care, administration sertvices, auxiliary medical service, and affiliated nursing care had the lowest level of work autonomy in CNA work contents. When compared with the mean score of work autonomy between nursing supervisors and CNAs, no statistically significant differences were present in views of CNA work autonomy in personal care, administration services, and social care between these two groups (Table 3). However, a significant difference in the mean scores for affilated nursing care (p<0.01) and auxiliary medical service was found (p<0.01). When all five
aspects of CNAs’ work contents were combined, the mean scores of work autonomy between these two groups was also statiscally different (p<0.01). In general, the nursing supervisors expected the CNAs to have more work autonomy in these two aspects than did the CNAs.
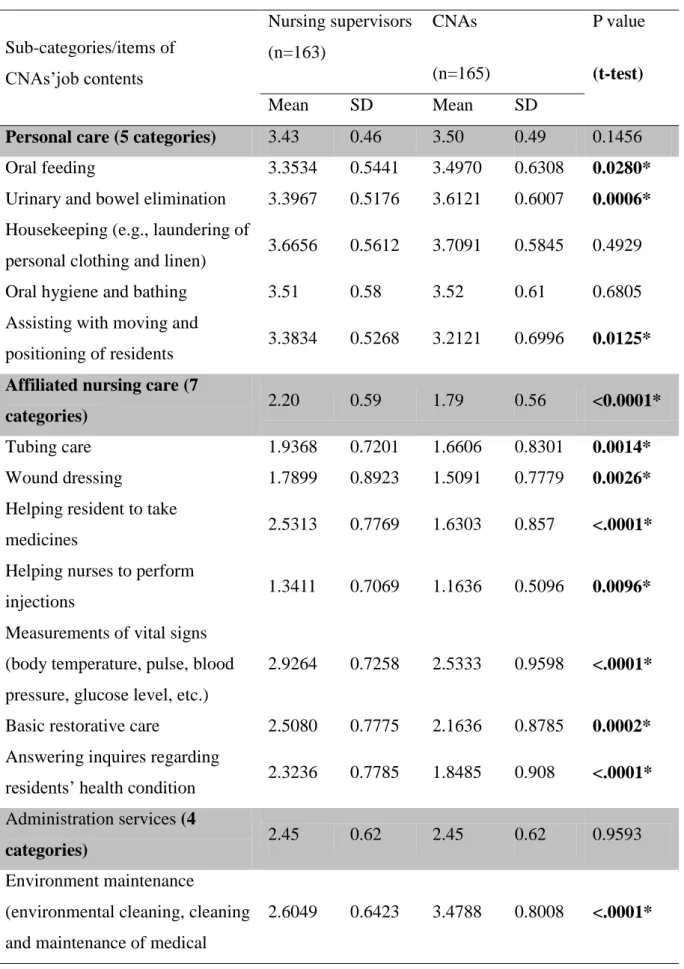
To understand the different perceptions toward the extent of work autonomy, each sub-category rated by the nursing supervisors and CNAs was further compared and the results were listed in Table 4. There were 3 categories (3/5) in personal care, seven (7/7) in affiliated nursing care, 2 (2/4) in administration services, 4 (4/6) in auxiliary medical service, and 4 items (4/13) in social care, in total, 20 categories/items that had significant difference in the mean scores of work autonomy between nursing supervisors and CNAs (p<0.05). In addition, for all the work categories/items that had significant different mean scores of work autonomy (between nursing supervisors and CNAs), the mean scores rated by nursing supervisors were generally higher than those rated by CNAs except for the oral feeding, urinary and bowel elimination in the aspects of personal care and environment maintenance in the aspect of administration services.
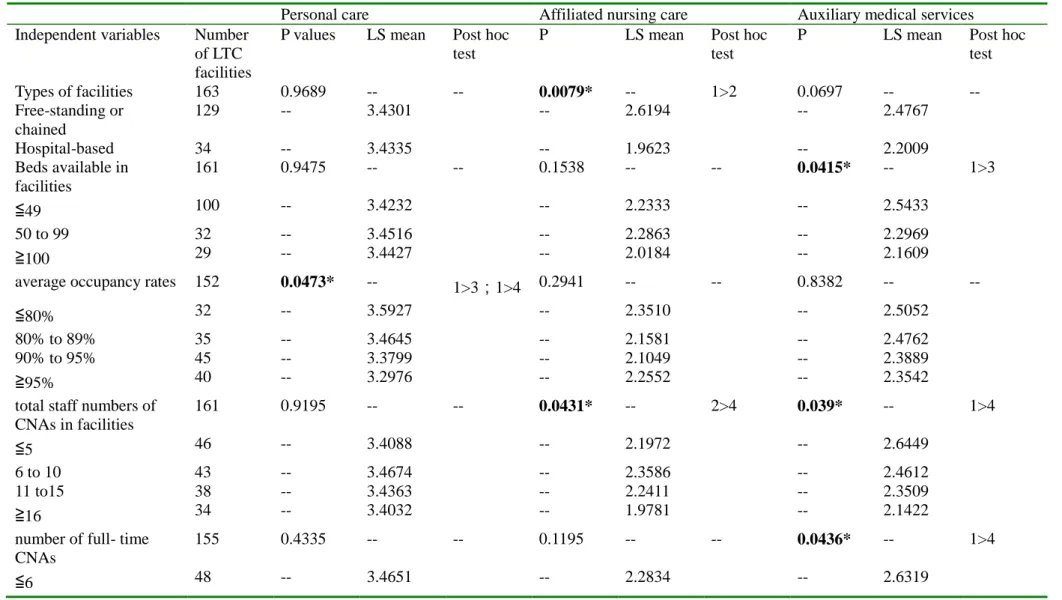
The relationships among the characteristics of institutions, staff numbers, and the extent of CNAs’ work autonomy as perceived by the nursing supervisors
Since the extent of work autonomy of CNAs may be influenced by the nursing
institutions (types, sizes, occupancy rates, and staff numbers) and the extent of CNAs’ work autonomy perceived by the nursing supervisors are shown in Table 5. The results showed that the types of institutions and the staff numbers of CNAs in sampled facilities were associated with the mean scores of work autonomy in the subcategories of nursing care rated by the responding nursing supervisors. That is, in the aspects of affiliated nursing care, the nursing supervisors in freestanding homes gave a higher mean score than those in hospital-based institutions. Institutions with the staff numbers above 16 have the lowest level of work autonomy of CNAs in the aspect of nursing care. In addition, the institutions with lower average occupancy rates rated the highest work autonomy of CNAs on the aspects of personal care. The sizes of the home, the total numbers of full-time CNA staff, and the numbers of residents in the homes were also found to be associated with the mean scores of work autonomy in auxiliary medical services. That is, the smaller the sizes of the home, the lower the level of CNA staff in homes, and the fewer the residents living in homes, nursing
supervisors expected CNAs to have higher work autonomy on the work items in auxiliary medical services. No difference among the aspects of the administration activities and the social care was seen. We have also analyzed the correlations among the types, occupancy rate, and CNA staff numbers with the characteristics of LTC facilities (Table 6). Correlations between the types of LTC facilities, the numbers of beds, total numbers of CNAs, and the numbers of full-time CNAs were found. In summary, the types, sizes (capacity), occupancy
rates, CNA staff numbers of the long-term care facilities, and resident numbers were related to the CNAs’ work autonomy as perceived by their nursing supervisors.
Discussion
This study aimed to explore the task identity and work autonomy of CNAs in long term care facilities from the perspectives of nursing supervisors and CNAs. From the nursing supervisors’ view, nearly one-fifth of CNAs’ work routines had coefficients of variation higher than 50%, suggesting discordance of views on some job contents of CNAs (Table 1). Our results found that the responding nursing supervisors have the greatest consensuses on the aspect of personal care and the least consensus on affiliated nursing care. In the aspect of affiliated nursing care, 15 work items (34.9%) belonged to the three categories of tubing care, wound dressing, and helping nurses with injections have coefficient of variation higher than 50%. It is interesting to note that CNAs ranked the work autonomy of each aspect of their work contents in the same order as did the nursing supervisors. However, among CNAs, they also expressed different views toward work autonomy (coefficient of variation higher than 50%), particularly in the aspects of affiliated nursing care and auxiliary medical services and some items of social care (Table 2). In these aspects, nursing supervisors expected CNAs to have higher work autonomy than did the CNAs (p < 0.001) (Tables 3 and 4). Consequently, these results raise several critical issues regarding CNAs’ job contents to be discussed.
Firstly, the role and the extent of work autonomy of CNAs in LTC facilities need to be addressed. From the open-ended questions of this study, the responding nursing supervisors expressed that the assistance from CNAs was indispensable. However, their concerns about CNAs’ work autonomy focused on the communication skills of CNAs’ with other health
professionals and families of residents rather than their skill competence.The lack of consensus on the issues of task identity and work autonomy pose a dilemma between workforce allocation and CNAs’ skill training and competence, particularly on the aspect of
affiliated nursing care. The areas of concern include tubing care of affiliated nursing cares, ranging from noninvasive sputum suction to invasive nasal-gastric tube insertion and urine catheterization for male residents. An investigation by Workman [20] in the UK, for example, found that nurses were concerned about the threat to their roles by HCAs (health care
assistants). Sometime, role ambiguity and task uncertainty are even more important to job satisfaction and retention for RNs than CNAs who work in long term care facilities. For the former group, these issues would also relate to responsibility and supervision. As expressed in the initial concerns of the health care assistants (HCAs) in the Burns’ study [21], they were keen to know the boundaries of roles and were worried whether that would be conflict with the expectations from other team members in the institutions. Therefore, for the benefit of residents in the LTC facilities, it is imperative for the nursing supervisors or managers to clarify the CNAs’ role and task identity of their work along with the degree of work
autonomy in their job contents under appropriate supervision.
Secondly, from the perspective of job quality in LTC facilities, and the practical issues in delivering quality care effectively and efficiently, the role and work delegation of CNAs must take into account in making health policy at the macro-level. In the recent trend of an ageing population and rising medical expenses of acute care hospitals, it is suggested that support workers should be more involved in routine daily care (e.g., grooming, feeding, and toileting) than just assisting nursing staff [22]. Since CNAs know most about the residents’ needs and provided the minute-to-minute care, as a team member, it is not easy to limit CNAs to some of the work belonging to RNs. Therefore, despite controversy, care assistants have been recognized as making a vital contribution to healthcare provision and previous research indicated that primary care personnel are not being utilized to the extent of their training [22]. In a report regarding the role of HCAs in NHS, UK, the authors found that HCAs were taking more responsibility to direct care, but the role of HCAs and the degree of legitimacy attached to it differed, reflecting underlying differences in the nursing model subscribed to by RNs at each trust [6]. Our results, consistent with these findings, found that the characteristics of LTC facilitates do affect the job delegation and work autonomy of CNAs. In the LTC industry with demanding workforce, the person-fit job redesign was built on evidence-based support and the environment, which CNAs could have the opportunity to use their knowledge on the job and control their work [23] and could actually increase staff stability and job
satisfaction. However, the challenge for the reconfiguration of CNA roles may rely on the paradigm shift of the managers and the leaders of LTC facilities to focus more on
target-oriented training for CNAs, rather than the traditional role of CNAs [6]. Therefore, development of effective and multiple ways to provide recognition and expand work responsibilities for CNAs are the major challenges for leaders in LTC facilities, which may include redesigning jobs and on-the-job training programs for CNAs so as to maintain appropriate growth and maturity in their work capabilities in LTC facilities. It should also consider the future partnership of nurses and CNAs. This managed strategy for human resources may resolve registered nurses’ difficulty in delegating work to CNAs and conflicts between nursing staff and CNAs.
The third issue related to work autonomy in LTC facilities is the number of staff. Staffing standards have proven to be related to the quality of care and associated with restraint use and the number of total deficiencies at all types of facilities [24]. Our results showed association between the institutional sizes, staff numbers and the perceptions of nursing supervisors toward work autonomy of CNAs (Table 5). The characteristics of homes and human resource allocations would apparently influence nursing supervisors’ perceptions in terms of their work assignment and supervision to CNAs. It is not uncommon in facilities with smaller staffing level to have the flexible use of staff and to request for more inputs and contributions from CNAs, and the extent of their work autonomy. Interestingly, previous
research reported that it was an issue related to good basic supervision that nursing assistants were more likely to be committed to their jobs when they perceived their supervisors to be respectful, helpful, and providing good feedback [8]. Actually, in LTC institutions with low wages and heavy job demands, workers may experience requests for more self-direction and knowledge input as further demands instead of job enhancements [8]. Therefore, it was not sufficient to have a consensus toward work autonomy of CNAs supported with knowledge and skill training; we found that, more importantly, it should be the consistent supervision of CNAs by nursing supervisors across different settings. The lack of education may be the single most important barrier to nursing supervisors’ effective delegation [25]. Formal efforts
to help RNs learn these skills must come through education and on-the-job training.
Finally, it is imperative for the government to sponsor the change of CNAs work across the occupational boundaries. The government has clearly regulated the duties of RNs under the legislations in Taiwan. Despite that CNAs have been recognized as an important and increasingly needed, however, no contemporary regulations specific to CNAs in Taiwan have been enacted. The nursing supervisors would perceive the role of CNAs and the degree of work autonomy attached to it differed, reflecting the respecitve differences subscribed to CNAs’ job contents by RNs at each homes. For example, most of nursing supervisors
reckoned the controversy surrounding the autonomy of CNAs to perform sputum suctions in the aspect of affiliated nursing care; however, our results revealed that work items beyond
sputum suction, mostly on the aspect of affiliated nursing care, and some aspects of auxiliary medical service and social care, also lacked a consensus among nursing supervisors and CNAs. It could be due to the lack of regulations or guideline in defining specific job descriptions for CNAs that nursing supervisors have different perceptions according to the organizational culture and norms in their homes. With the increasing demand for CNAs in LTC facilities, clear guidelines and regulations based on the resident-centered task identity are warranted and should be mandated accordingly. As such, these guidelines or regulations may resolve the controversial issue and discrepant perceptions of work autonomy in the job contents of CNAs between CNAs and nursing supervisors, improve quality of care, and protect practice nurses, certified nursing assistants, employers, and residents in LTC facilities alike.
Conclusion
In summary, increasing demand for CNAs’ contributions in long-term care facilities has been inevitable. From our study, there are discordance views towards CNAs’ work autonomy both in nursing supervisors and CNAs across different settings in daily care. A consistent good nursing supervision in terms of CNAs’ job delegation by nursing supervisors and across long-term care facilities, could help with reducing CNAs’ role ambiguity and their task identity, and further to enhance their job satisfaction. Nursing supervisors may need more
training as supervisors of CNAs, and CNAs also need more support for their work identity and autonomy to improve their performance from the management. Further researches are needed to explore the newly emerging partnership between RNs and CNAs and new models of care and evidence-based practice (e.g., clear practice guidelines) that often require the impetus to change to produce successful, sustainable improvements in long-term care.
Acknowledgements
This study was supported by the grants of National Science Council, Taiwan, NSC94-2416-H-426-001 and NSC95-2416-H-039-003. The authors wish to thank the
cooperation from nursing staff and certified nursing assistants interviewed in this island-wide survey. We sincerely thank Professor Anthea Tinker, King’s College London, UK, for her critically proofreading of the manuscript.
References
1. Liu LF. Job satisfaction of certified nursing assistants and its influence on the general satisfaction of nursing home residents: An exploratory study in southern Taiwan.
Geriatr Nurs 2007; 28:54-62.
2. Stone RI, Dawson SL. The origins of better job better care. Gerontologist, 2008; 48:5-13.
3. Institute of Medicine. Quality of care in nursing homes. 2001, National Academy Press, Washington, DC.
4. Lee SD. National health research institutes report on aging research. 1997, National Health Research Institutes. Taipei.
5. Baldwin J, Roberts JD. Fitzpatrick JI, While A, et al. The role of support worker in nursing homes: a consideration of key issues. J Nurs Manag 2003; 11:410-420.
6. Bach S, Kessler I, Heron P. Role redesign in a modernized NHS: the case of health care assistants. Hum Res Manag J 2008; 18:171-187.
7. Pennington K, Scott J, Magilvy K. The role of certified nursing assistants in nursing homes. J Nurs Admin 2003; 33:378-384.
8. Bishop CE, Weinberg DB, Walter L, Dossa A, et al. Nursing assistants’ job commitment: effect of nursing home organizational factors and impact on resident well-being.
Gerontologist 2008, 48 (Special issue 1):36-45.
9. Tyler DA, Parker VA, Engle RL, Brandeis GH, et al. An exploration of job design in long-term care effect on nursing employee satisfaction. Heal Care Manag Rev, 2006; April-June, 137-144.
10. Perry M, Carpenter I, Challins D, Hope K. Understanding the roles of registered general nurses and assistants in UK nursing homes. J Adv Nurs 2003; 42:497-505.
11. Brannon D, Zinn JS, Mor V, Davis J. An exploration of job, organizational, and environmental factors associated with high and low nursing assistant turnover.
Gerontologist, 2002; 42:159-168
12. Casltle NG, Engberg J. Staff turnover and quality of care in nursing homes. Med Care 2005; 43:616-626
13. Parsons SK, Simmons WP, Penn K, Furlough, M. Determinants of satisfaction and turnover among nursing assistants: The results of a statewide survey. J Gerontol Nurs 2003; 29:51–58.
14. Hall LM, O'Brien-Pallas L. Redesigning nursing work in long-term care environments.
Nurs Econ 2000; 18:79-87
15. Hackman JR, Oldham GR. Work Redesign. 1980, Prentice Hall, USA.
16. Lorence J, Mortimer JT. Job involvement through the life course: a panel study of three age groups. Am Soc Rev 1985; 50:618-638.
17. Hsieh PC, Su HF. Retention and attrition of certified care assistants in the long-term care industry from the Taipei area: An interview survey. Int J Nurs Stud 2007; 44:93-104. 18. Serrentino SA, Gorek B: Basic Skills for Nursing Assistants in Long Term Care - Text &
Workbook Package (1 ed). 2005, Mosby, USA.
19. http://vol.moi.gov.tw. Ministry of Interior of the Executive Yuan, Taiwan. The ten year long-term care plan of Taiwan. 2007. Accessed on February, 2009.
20. Workman B. An investigation into how the health care assistants perceive their role as support workers to the qualified staff. J Adv Nurs 1996; 23:612–619.
21. Burns S. Developing the health care assistant role. Pri Health Care 2006; 16, 21-25. 22. Hysong SJ, Best RG, Moore FI. Are we under-utilizing the talents of primary care
personnel? A job analytic examination. Implementation Sci 2009; 2:10-31.
Effects on nursing home resident outcomes. Gerontologist 2005;43:309-317. 24. Park J, Stearns SC. Effects of state minimum staffing standards on nursing home
staffing and quality of care. Health Serv Res 2009; 44:56-73.
25. Institute of Medicine. Retooling for an Aging America: Building the Health Care
Table 1 Nursing supervisors’ views toward the work autonomy of CNAs’ job contents.
Categories and items of CNAs’ Job contents
Mean SD Coefficient of variation (%) Personal care (5 categories, 31 items) 3.43 0.41 11.95
Affiliated nursing care (7 categories, 43 items)
2.20 0.59 26.82
b
Tubing care 1.57 0.83 52.87
Wound dressings 1.79 0.89 55.87
Helping nurses to perform injections 1.34 0.71 52.99 Administration services (4 categories, 19
items)
2.45 0.62 25.31
Auxiliary medical service (6 items) 2.42 0.8 33.06 Liaisons with medical facilities 2.09 1.10 52.63 Helping physician to examine the resident 1.95 1.06 54.36
Social care(13 items) 2.90 0.72 24.83
refer for legal consultation 2.06 1.07 51.94
a
Coefficient of variation was calculated as the percentage of standard deviation dividing by mean, which represent the range of data among multiple groups.
b
Only the job subcategories or items with coefficient of variation over than 50% of its mean score (i.e. discordance within group) are shown .
Table 2 CNAs’ view toward the work autonomy of their job contents
Categories and items of CNAs’ Job contents
Mean SD aCoefficient of variation (%)
Personal care (5 categories, 31 items) 3.50 0.49 14.02 Affiliated nursing care (7 categories, 43
items)
1.79 0.56 31.57
b
Tubing care 1.66 0.83 50.00
Wound dressings 1.51 0.78 51.55
Helping resident to take medicine 1.63 0.86 52.57 Administration service (4 categories, 19
items)
2.45 0.62 25.00
Auxiliary medical services (6 items) 2.14 0.73 33.90 Liaisons with medical facilities 1.82 0.97 53.10 Helping physician to examine the resident 1.73 0.94 54.39 Escorting the resident for admission to
medical facilities
2.04 1.10 53.93
Social care (13 items) 2.75 0.68 24.80
Routine telephone contact with the residents’ families
2.19 1.20 54.97
Routine home visits to the residents’ families 2.08 1.20 57.39 Refer for legal consultation 1.60 0.88 55.13
a
Coefficient of variation was calculated as the percentage of standard deviation dividing by mean, which represent the range of data among multiple groups.
b
Only the job sub-categories or items with coefficient of variation over than 50% of its mean score (i.e. discordance within group) were shown on the table.
Table 3 Comparison of the mean scores of work autonomy in five main aspects of CNA
job contents between nursing supervisors and CNAs.
Main aspects of CNAs’ job contents Nursing supervisors (n=163) CNAs (n=165) P value (t-test) Mean SD Mean SD Personal care 3.43 0.46 3.50 0.49 0.1456
Affiliated nursing care 2.20 0.59 1.79 0.56 <0.0001
Administration services 2.45 0.62 2.44 0.62 0.9593 Auxiliary medical services 2.42 0.79 2.14 0.73 0.0011
Social care 2.90 0.73 2.75 0.68 0.0629
Table 4. Comparison of the mean scores of work autonomy in sub-categories/items of CNAs job contents between nursing supervisors and CNAs.
Sub-categories/items of CNAs’job contents Nursing supervisors (n=163) CNAs (n=165) P value (t-test) Mean SD Mean SD
Personal care (5 categories) 3.43 0.46 3.50 0.49 0.1456
Oral feeding 3.3534 0.5441 3.4970 0.6308 0.0280*
Urinary and bowel elimination 3.3967 0.5176 3.6121 0.6007 0.0006* Housekeeping (e.g., laundering of
personal clothing and linen) 3.6656 0.5612 3.7091 0.5845 0.4929 Oral hygiene and bathing 3.51 0.58 3.52 0.61 0.6805 Assisting with moving and
positioning of residents 3.3834 0.5268 3.2121 0.6996 0.0125* Affiliated nursing care (7
categories) 2.20 0.59 1.79 0.56 <0.0001*
Tubing care 1.9368 0.7201 1.6606 0.8301 0.0014*
Wound dressing 1.7899 0.8923 1.5091 0.7779 0.0026*
Helping resident to take
medicines 2.5313 0.7769 1.6303 0.857 <.0001*
Helping nurses to perform
injections 1.3411 0.7069 1.1636 0.5096 0.0096*
Measurements of vital signs (body temperature, pulse, blood pressure, glucose level, etc.)
2.9264 0.7258 2.5333 0.9598 <.0001*
Basic restorative care 2.5080 0.7775 2.1636 0.8785 0.0002* Answering inquires regarding
residents’ health condition 2.3236 0.7785 1.8485 0.908 <.0001* Administration services (4
categories) 2.45 0.62 2.45 0.62 0.9593
Environment maintenance
(environmental cleaning, cleaning and maintenance of medical
instruments)
Help nurses to perform their
administrative jobs 2.2446 0.6851 2.0303 0.9654 0.0210* Communication with residents’
family members and participating in case discussion.
2.3160 0.8565 2.2242 0.799 0.3167
Helping to plan and perform daily
activities in the facilities 2.1288 0.8301 2.0545 0.8209 0.4157 Auxiliary medical services (6
categories) 2.42 0.79 2.14 0.73 0.0011*
Liaisons with medical facilities 2.0920 1.0989 1.8242 0.9687 0.0198* Escorting resident to out-patient
department in medical facilities 2.8405 0.8159 2.6727 0.8846 0.0752 Escorting resident to emergency
service 2.6074 0.9192 2.5515 0.8654 0.5714
Helping physician to examine
residents 2.4110 0.9605 2.0485 0.8958 0.0005*
Arranging physician clinical
rounds in LTC facilities 1.9509 1.0646 1.7273 0.9394 0.0444* Escorting the resident for
admission to medical facilities 2.6135 0.9707 2.0364 1.0982 <.0001* Social care (13 categories) 2.90 0.73 2.75 0.68 0.0629 Routine telephone contact with
the residents’ families 2.7546 1.031 2.1879 1.2026 <.0001* Routine home visits to the
resident’s families 2.5521 1.0432 2.0848 1.7966 0.0002* Chatting with resident 3.3865 0.8114 3.4303 0.8919 0.6422 Listening to residents’ complaints 3.4110 0.7756 3.4727 0.8232 0.4855 Helping residents’ to contact their
families 2.8589 0.993 2.8303 1.1241 0.8074
Helping residents with letters
writing 3.0184 1.0685 2.8667 1.1558 0.2180
telephone calls
Helping residents with daily
activities and decisions 2.9018 0.9109 2.9212 0.937 0.8496 Help residents with outdoor
activities 2.7301 0.9432 2.5152 0.9602 0.0417*
Shopping for the residents by
their request 3.0000 0.9362 2.9758 1.0874 0.8289
Assisting with daily grocery
shopping 2.8957 0.9914 2.8970 0.9916 0.9908
Referral to legal consultations 2.0613 1.0697 1.6000 0.8821 <.0001* Help to perform recreation
Table 5. The relationship between the independent variables (characteristics of institutions, staff) and the dependent variables (the degree of work autonomy of CNAs’ job contents viewed by the nursing supervisors)
Personal care Affiliated nursing care Auxiliary medical services Independent variables Number
of LTC facilities
P values LS mean Post hoc test
P LS mean Post hoc test
P LS mean Post hoc test Types of facilities 163 0.9689 -- -- 0.0079* -- 1>2 0.0697 -- -- Free-standing or chained 129 -- 3.4301 -- 2.6194 -- 2.4767 Hospital-based 34 -- 3.4335 -- 1.9623 -- 2.2009 Beds available in facilities 161 0.9475 -- -- 0.1538 -- -- 0.0415* -- 1>3 ≦49 100 -- 3.4232 -- 2.2333 -- 2.5433 50 to 99 32 -- 3.4516 -- 2.2863 -- 2.2969 ≧100 29 -- 3.4427 -- 2.0184 -- 2.1609
average occupancy rates 152 0.0473* -- 1>3;1>4 0.2941 -- -- 0.8382 -- --
≦80% 32 -- 3.5927 -- 2.3510 -- 2.5052
80% to 89% 35 -- 3.4645 -- 2.1581 -- 2.4762
90% to 95% 45 -- 3.3799 -- 2.1049 -- 2.3889
≧95% 40 -- 3.2976 -- 2.2552 -- 2.3542
total staff numbers of CNAs in facilities 161 0.9195 -- -- 0.0431* -- 2>4 0.039* -- 1>4 ≦5 46 -- 3.4088 -- 2.1972 -- 2.6449 6 to 10 43 -- 3.4674 -- 2.3586 -- 2.4612 11 to15 38 -- 3.4363 -- 2.2411 -- 2.3509 ≧16 34 -- 3.4032 -- 1.9781 -- 2.1422
number of full- time CNAs
155 0.4335 -- -- 0.1195 -- -- 0.0436* -- 1>4
7 to 10 32 -- 3.5161 -- 2.2754 -- 2.4115 11 to 17 38 -- 3.4423 -- 2.2797 -- 2.4518 ≧18 37 -- 3.3383 -- 1.9843 -- 2.1396 Numbers of residents living in facility 160 0.8451 -- -- 0.2075 -- -- 0.0251* -- 1>3;1>4 ≦23 42 -- 3.4286 -- 2.3311 -- 2.6786 24 to 41 41 -- 3.4831 -- 2.2127 -- 2.5000 42 to 64 38 -- 3.4015 -- 2.1769 -- 2.2939 ≧65 39 -- 3.4020 -- 2.0781 -- 2.1880 1. *P<0.05,** P<0.01。
2. The level of work autonomy: 1=CNAs were not allowed to work independently; 2=CNAs were allowed to work with nurse professionals under supervision; 3=CNAs could work independently after training and delegation of tasks by nurse professionals; 4=CNAs could work independently.
3. The table only shows the variables with a statistical difference between independent (characteristics of institutions, staff) and dependent variables (the aspects of CNAs’ job contents).
4. LS-means are, in effect, within-group means appropriately adjusted for the other effects in the model. More precisely, they estimate the marginal means for a balanced population (as opposed to the unbalanced design). For this reason, they are also called estimated population marginal means (Searle, Speed & Milliken, 1980).
able 6. The comparison of various parameters between hospital-based and free-standing (or chained) LTC facilities.
Parameters of the scale of LTC facilities
Characteristics of LTC facilities Number Free-standing (or
chained) (%) Hospital-based (%) p value Number of beds 161 78.88 21.12 0.0224* ≦49 100 66.93 44.12 -- 50 to 99 32 15.75 35.29 -- ≧100 29 17.32 20.59 --
Total number of CNAs 161 78.88 21.12 0.0149*
≦5 46 33.07 11.76 -- 6 to 10 43 28.35 20.59 -- 11 to 15 38 21.26 32.35 -- ≧16 34 17.32 35.29 -- Number of full-time CNAs 155 78.71 21.29 0.0291* ≦ 6 48 34.43 18.18 -- 7 to 10 32 20.49 21.21 -- 11 to 17 38 26.23 18.18 -- ≧18 37 18.85 42.42 -- Number of part-time CNAs 151 78.15 21.85 0.0861 0 91 56.78 72.73 -- 1 to 2 23 17.80 6.06 -- 3 to 5 18 14.41 3.03 -- 6 to 8 9 5.93 6.03 -- ≧ 9 10 5.08 12.12 -- Number of residents 160 78.75 21.25 0.1520 ≦ 23 42 29.37 14.71 -- 24 to 41 41 26.98 20.59 -- 42 to 64 38 22.22 29.41 -- ≧ 65 39 21.43 35.29 -- Occupation rate 161 79.61 20.39 0.2893 ≦ 80% 32 22.31 16.13 -- 80% to 89% 35 19.83 35.48 -- 90% to 95% 45 29.75 29.03 -- ≧ 95% 40 28.10 19.35 --
Figure 1. The mean score of work autonomy of CNAs job contents as viewed by nursing supervisors and CNAs
2.44 2.14 1.79 2.75 3.5 2.2 2.42 2.45 2.9 3.43 0 0.5 1 1.5 2 2.5 3 3.5 4 Personal care Social-needs care Administration services Auxiliary medical services
Affiliated nursing care
CNAs NSs