行政院國家科學委員會專題研究計畫 成果報告
子計畫五:疾病動物模式奈米微粒毒性探討(III)(2/2)
計畫類別: 整合型計畫
計畫編號: NSC93-2621-Z-002-004-
執行期間: 93 年 08 月 01 日至 94 年 07 月 31 日
執行單位: 國立臺灣大學公共衛生學院職業醫學與工業衛生研究所
計畫主持人: 鄭尊仁
計畫參與人員: 雷侑蓁,鄭伊玲,陳麗真
報告類型: 完整報告
處理方式: 本計畫可公開查詢
中 華 民 國 94 年 10 月 20 日
行政院國家科學委員會補助專題研究計畫
■ 成 果 報 告
□期中進度報告
奈米微粒與健康風險研究-子計畫五:疾病動物模式奈米微粒毒性探討
計畫類別:□ 個別型計畫
▓ 整合型計畫
計畫編號:NSC 91-2621-Z-002-026
NSC 92-2621-Z-002-014
NSC 93-2621-Z-002-014
執行期間:2002 年 8 月 1 日至 2005 年 7 月 31 日
計畫主持人:鄭尊仁
計畫參與人員:雷侑蓁、鄭伊玲、陳麗貞
成果報告類型(依經費核定清單規定繳交):□精簡報告 ▓完整報告
本成果報告包括以下應繳交之附件:
□赴國外出差或研習心得報告一份
□赴大陸地區出差或研習心得報告一份
□出席國際學術會議心得報告及發表之論文各一份
□國際合作研究計畫國外研究報告書一份
處理方式:除產學合作研究計畫、提升產業技術及人才培育研究計畫、列
管計畫及下列情形者外,得立即公開查詢
□涉及專利或其他智慧財產權,□一年□二年後可公開查詢
執行單位:國立台灣大學職業醫學與工業衛生研究所
中
華
民
國
年
月
日
奈米微粒與健康風險研究-子計畫五:疾病動物模式奈米微粒毒性探討
計畫編號:NSC91-2621-Z-002-026、NSC 92-2621-Z-002-014、NSC 93-2621-Z-002-014 執行期限:2002 年 8 月 1 日至 2005 年 7 月 31 日 主持人:鄭尊仁 國立台灣大學職業醫學與工業衛生研究所 計畫參與人員:雷侑蓁、鄭伊玲、陳麗貞 國立台灣大學職業醫學與工業衛生研究所 摘要 流行病學研究指出,空氣污染氣懸微粒的增 加,與呼吸系統疾病和心血管疾病死亡率增加有 關,這些死亡大都發生於已經有心肺疾病的個 人,然而確實致病機轉仍不清楚。近年研究發現 小粒徑微粒可能扮演更重要的角色,特別是奈米 微粒在同一重量濃度下,顆粒數變大,表面積也 加大,可能增加毒性,目前已有一些研究針對奈 米微粒與細胞毒性的關係進行探討,主要著重在 奈米微粒造成的發炎反應,但是對於奈米微粒引 起的呼吸道變化及心血管系統效應之間的關係並 不清楚,特別在易感性族群的健康效應研究更 少。本研究目的為:(1)探討肺高血壓疾病動物暴 露奈米聚苯乙烯後,肺部發炎與傷害反應,及氧 化壓力的產生,同時也探討這些指標與表面積之 相關。(2)以糖尿病大鼠模式進行奈米微粒心血管 毒性試驗,以氣管灌注方式暴露奈米碳黑,觀察 其肺部發炎及周邊血液發炎反應與內皮細胞功能 標記之變化。(3)探討自發性高血壓大鼠與健康 SD 大鼠在暴露奈米微粒後,肺部發炎與氧化傷害 之比較。(4)探討非細胞系統中奈米微粒粒徑與氧 化壓力之相關。(5)探討肺部上皮內襯液體(ELF) 對於奈米微粒引起細胞氧化傷害的影響,評估奈 米微粒與細胞反應後產生之氧化壓力及評估細胞 DNA 單股斷裂情形。 研究結果顯示,肺高血壓大鼠暴露微粒後, 暴露小粒徑微粒的動物有較高的肺部發炎及傷害 反應,同時這些反應與總表面積有關,另外氧化 壓力指標也有類似趨勢。我們也發現糖尿病大鼠 及健康大鼠,暴露於奈米碳黑都導致顯著的肺部 發炎及傷害反應,但是奈米碳黑只在糖尿病大鼠 造成顯著的周邊發炎反應增加,血管內皮素升高 及血液一氧化氮降低,奈米微粒暴露可能與糖尿 病有共同的的病理生理作用途徑,造成心血管疾 病增加的風險。進一步研究比較自發性高血壓大 鼠與健康 SD 大鼠的肺部發炎與氧化壓力,自發 性高血壓大鼠因抗氧化壓力能力較差,所以不管 在肺部發炎反應或氧化壓力指標都比較健康 SD 大鼠明顯。因為奈米微粒之毒性與氧化壓力有 關,所以進一步在非細胞系統中,測試奈米微粒 氧化壓力的產生,發現奈米碳黑產生的氧化壓力 隨暴露濃度及暴露時間增加,同時與總表面積有 關。而碳黑微粒在添加 ELF 的環境下能顯著降低 氧化壓力的產生,同時減少 DNA 單股斷裂的產 生。 我們的研究顯示,相同重量下,同材質的奈 米微粒毒性較粗微粒高,可能與奈米微粒的數目 及總表面積皆較粗微粒高,引起較大的氧化壓力 有關;奈米微粒除了造成肺部疾病,可能也與心 血管疾病有關,特別是易感性的糖尿病者,奈米 微粒的毒理效應更大,研究也發現氧化壓力在微 粒導致的肺部及心血管疾病,扮演重要角色。另 外,我們發現非細胞系統也可進一步發展成篩檢 的工具。研究顯示奈米粒徑微粒可在大氣微粒扮 演重要角色,同時在奈米材料毒性研究上,也提 供有用的資訊,有關奈米微粒毒理機轉,有待進 一步研究。 本研究報告將依照年度分為三部分,第一部 份為聚苯乙烯對肺高血壓大鼠之肺部發炎反應研 究。第二部份為糖尿病大鼠暴露奈米微粒之心血 管疾病研究,以及肺部上皮內襯液體(ELF)對於 奈米微粒引起細胞氧化傷害及細胞 DNA 單股斷裂 的影響。第三部份為奈米微粒於非細胞系統之氧 化壓力反應,還有自發性高血壓大鼠與健康 SD 大 鼠的肺部發炎與氧化壓力之比較。 關鍵詞:奈米微粒,心肺毒性,氧化壓力,肺高 血壓大鼠,糖尿病大鼠,自發性高血壓大鼠,內 皮細胞功能,碳黑,聚苯乙烯 AbstractEpidemiologic studies have shown consistent associations between the exposure to particulate air pollution and acute increase in morbidity and mortality, especially for susceptible subjects with pre-existing respiratory and cardiovascular disease. However, the exact mechanism remains unclear. Recent studies have shown that ultrafine particles may have a greater inflammatory effect than larger particles at the same mass concentration because of larger surface area and oxidative stress. However, the role of ultrafine particles on cardiopulmonary events is not clear. The goal of this study was: (1) to investigate the lung inflammation and oxidative
2
stress in pulmonary hypertensive rats exposed to polystyrene particles. (2) to evaluate the effect of ultrafine carbon black on lung inflammation, systemic inflammation and endothelial dysfunction in STZ-diabetic rats. (3) to compare the lung inflammation and oxidative stress between spontaneously hypertensive rats and healthy SD rats. (4) to investigate the oxidative stress formation in a cell free system exposed to carbon black nanoparticles. (5) to investigate the effect of epithelium lining fluids (ELF) on ultrafine carbon black-induced ROS generation and DNA single strand breaks. Our results revealed that polystyrene nanoparticles can induce greater lung inflammation and injury and oxidative stress as compared to larger particles. The outcome parameters and total surface area were also highly correlated. Carbon black nanoparticles induced lung inflammation in both DM and non-DM rats, while abnormal endothelial function was only observed in DM rats. We further
compared the lung inflammation and oxidative stress between SHR and SD, and found that those parameters were greater in SHR. In cell free system, the amounts of ROS increased with exposure concentration and exposure time. ELF significantly decreased ROS and DNA SSB. Our results indicate that nanoparticles can induce oxidative stress, which may be related with subsequent cardiopulmonary changes. The results also found that diseased subjects were more susceptible to nanoparticles. It is interesting to know that nanoparticles and diabetes may share the common pathway leading to cardiovascular events. We also find that cell free system may be used to screen nanoparticles.
Keywords: nanoparticles, diabetic rats, epithelium
lining fluid, reactive oxygen species, cardiopulmonary disease, endothelial function, spontaneously hypertensive rats, pulmonary hypertension, carbon black, polystyrene
奈米微粒與健康風險研究-子計畫五:疾病動物模式奈米微粒毒性探討
(I)
計畫編號:NSC91-2621-Z-002-026 執行期限:2002 年 8 月 1 日至 2003 年 7 月 31 日 主持人:鄭尊仁 國立台灣大學職業醫學與工業衛生研究所 計畫參與人員:雷侑蓁 國立台灣大學職業醫學與工業衛生研究所 中文摘要 目的 早期對於奈米微粒的毒性研究著重在金屬 作業場所,通常探討工人暴露於會引起金屬燻煙 熱的奈米燻煙微粒所造成的健康效應。最近的流 行病學研究指出,空氣污染中的大氣懸浮微粒暴 露與心肺疾病死亡率增加有關,相關研究指出, 大氣奈米微粒可能是呼吸與心血死亡率增加的重 要原因之一,然而機制並不清楚。奈米技術已成 為高科技產業的主軸,製程中產生的奈米微粒對 健康產生的影響並不清楚,因此有必要針對奈米 微粒毒性進行系統性的研究。本研究以低毒性的 聚苯乙烯奈米微粒進行細胞及動物實驗,探討不 同粒徑、數目濃度之奈米微粒造成的毒理效應。 方法 奈米聚苯乙烯微粒粒徑範圍包括 64、109、 535-nm,細胞實驗方面,以人類第二型肺泡上皮 細胞(A549)進行粒徑為 64、109、202、535-nm 之奈米微粒 100μg/ml 及 1mg/ml 各 4 小時之暴 露,以 ELISA 測定發炎前趨物細胞激素 IL-8 及 IL-6 之表現。動物實驗則以肺高血壓疾病動物模 式進行,以氣管灌注 0.5mlPBS 生理緩衝液為控制 組,0.5ml 100μg/ml 及 50μg/ml 的 64、109、202、 535-nm 奈米微粒為暴露組,暴露後 24 小時將大 鼠犧牲,收集肺灌洗液、組織及周邊血液,進行 肺部發炎指標及氧化壓力指標測量。 結果 細胞實驗方面,人類第二型肺泡上皮細胞 A549,暴露於 100μg/ml 奈米微粒組有較高之發炎 前趨細胞激素 IL-8 表現。動物實驗方面,與對照 組比較,暴露於 64-nm 奈米微粒之肺高血壓大 鼠,肺泡灌洗液之總細胞數及嗜中性球比例、及 總蛋白質皆顯著高於同質量濃度下較大粒徑的暴 露組,同時肺部灌洗液產生的細胞激素 IL-6 亦高 於對照組,代表暴露於奈米微粒的疾病動物肺部 有顯著的發炎反應。另外,暴露於 64-nm 奈米微 粒之大鼠,其肺部組織 GSH 則較對照組有明顯降 低的趨勢,與奈米微粒的表面積有劑量反應關 係;同時周邊血液的氧化壓力產物 8-OHdG 亦隨著 奈米微粒反應表面積的增加而上升,顯示暴露於 奈米微粒後會產生較高之氧化壓力。 結論 結果顯示,暴露於低毒性的奈米微粒會造成 肺高血壓大鼠肺部損傷,並且引發氧化壓力,造 成顯著發炎反應,本研究建議針對其他材質的奈 米微粒毒性及毒理機制進一步研究。 關鍵字:奈米微粒,人類肺泡上皮細胞,肺高血 壓大鼠,發炎指標 Abstract ObjectiveThe effects of air pollution particles on cardiopulmonary mortality and morbidity have been well documented. However the role of ultrafine particles on the mechanism of lung injury is unclear. The aim of the present study is to investigate inflammatory responses and oxidative stress of ultrafine polystyrene particles on disease animal model and alveolar cell lines.
Method
MCT-induced pulmonary hypertension rats were exposed to 100μg/mland 1 mg/mlof64-nm polystyrene nanometer particles by intratracheal instillation and sacrificed after 24h. Peripheral blood and brochoalveolar lavage fluid were collected for analysis of inflammation and oxidative stress markers. Further, A549 epithelial cells were exposed of100μg/mland 1 mg/mlof64,109 and 202-nm ultrafine polystyrene particles for 4 hours, respectively. Cytokine IL-6 and IL-8 were measured using ELISA.
Results
In the pulmonary hypertensive rats model, we demonstrated that there was a significant increase in total cells and percentage of neutrophils (p<0.05) in
2
100μg/mlof64-nm polystyrene particles compared with control rats. The total protein in bronchoalveolar lavage fluid showed a significant increase after treatment of 64-nm particles than controls (p<0.05). The depletion of glutathione (GSH) in the lung tissue was also observed in rats after the instillation of 64-nm ultrafine particles as compared with the control. We also demonstrated that higher cytokine IL-6 (p<0.05) and TNF-α in rats after instillation of 64-nm ultrafine particles. We observed that100μg/mlofultrafinepolystyrene particles induced higher levels of cytokine IL-8. However, IL-6 level were not increase after the particle treatment.
Conclusion
These findings suggest that ultrafine particles composed of low toxicity materials such as polystyrene may cause lung inflammation and oxidative stress in disease animal model, even at lower concentration.
Key words: nanometer particles, A549, pulmonary
hypertensive rats, inflammation
Introduction
Epidemiologic studies have shown consistent associations between the exposure to particulate air pollution and acute increase in morbidity and mortality, especially for susceptible subjects with pre-existing respiratory and cardiovascular disease (Pope et al., 2002; Pope and Dockery 1999; Samet et al., 2000). These epidemiologic studies also document that particles with a diameter below 2.5μm (PM2.5) have greater adverse health outcomes
as compared to particles with a diameter below 10μm (PM10). Recent studies further indicate that
the ultrafine particles (< 100 nm), which by count constitute the majority of urban particulate air pollution, may have an increased toxicity relative to larger particles under the same mass concentration (Ferin et al., 1992; Oberdorster et al., 1995; 2001).
One explanation of ultrafine particle toxicity is the production of oxidative stress. Reactive oxygen species (ROS) may be generated through the interaction between surface area of ultrafine particles and target cells, such as macrophages and epithelial cells. Then, ROS may elicit transcription of proinflammatory cytokines and result in a cascade of inflammation events (Stone et al., 1998). Many studies suggest that transition metals that are released from particle surface may be responsible for ROS generated toxicity (Dreher et al., 1997; Kodavanti et al., 1999). In addition, recent studies further suggest that inflammation observed in rats exposed to ultrafine carbon black and polystyrene
particle is due to either surface area or particle number effects, in the absence of transition metals (Brown et al., 2000, 2001). However, the relationship between ROS and surface area of ultrafine particles in susceptible population is still unclear.
Reduced glutathione (GSH) functions as a coenzyme in detoxification of xenobiotics and carcinogens, and as an antioxidant (Meister and Anderson, 1983). Depletion of GSH has been used as indicator of oxidative stress following PM exposure (MacNee et al., 1997). 8-hydroxydeoxyguanosine (8-OHdG) is one of the most abundant oxidative DNA adducts, a specific DNA damage which may initiate carcinogensis. It is mutagenic in nature and can cause G to T transversion (Loft and Poulsen, 1996). Exposure to urban particles have been associated with increased DNA damage (Corero et al., 2001). In this study, we investigated the effect of ultrafine polystyrene particles on inflammation and oxidative stress markers in pulmonary hypertensive rats; to determine whether surface area of ultrafine polystyrene particles play an important role in ROS generation in diseased animals.
Materials and methods
A549 cell culture and exposure to polystyrene particle
The human A549 cell line was from American Type Culture Collection and cultured in a humidified 37oC environment in F12-K medium supplemented with 10% fetal calf serum and 1% penicillin and streptomycin. This cell line, derived from a patient with alveolar cell carcinoma of the lung, has been used as a model of human alveolar type II cells. A549 epithelial cells were exposed to 100μg/ml of 64, 109 and 202-nm ultrafine polystyrene particles for 4 hours, respectively. Determination of cytokine IL-8 (R&D Systems, Minneapolis, MN) concentration was performed using ELISA.
Animals
Male Sprague-Dawley rats (body weight from 300 to 350g) were obtained from the National Laboratory Animal Breeding and Research Center, Taiwan. They were housed in plastic cages on Aspen chip bedding, and provided with Lab Diet 5001, water ad lib, except during the exposure. Animals were maintained on a 12-hour light/dark cycle at 22 + 1C and 55 + 10 % relative humidity.
Development of pulmonary hypertension
The model of pulmonary hypertension rats following treatment of rats with Monocrotaline
(MCT) was used (Kodavanti et al., 1998). A single intraperitoneal injection of MCT (Sigma Chemical Co., 60mg/kg) was administered to each rat. Fourteen days after MCT treatment, polystyrene particles instillaiton was conducted.
Polystyrene particle instillation
Polystyrene microspheres in three sizes: 64, 202 and 535 nm average diameter (Polysciences, UK) were suspended at a concentration of 100 and 50 μg/ml in idd H2O. Estimated surface area of instilled dose was in Table 1. Animals were anesthetized and 100 and 50μg/mlofeach particle suspension in 0.5 ml PBS was instilled into the lungs. Animals (n=4) received 0.5 ml PBS were as control group.
Bronchoalveoalr lavage
Rats were sacrificed 24h after intratracheal instillation. BAL fluid was collected by washing the airway with a phosphate-buffered saline solution (PBS, pH = 7.4, 28 ml/kg body weight) five times. Lavage fluid was used to determine the total number of cells and cell differential counts. Macrophage, lymphocyte, neutrophils, eosinophils and basophiles were counted under light microscopy (200 cells/slide). The remaining lavage fluid was used for the analysis of total protein and LDH activity. LDH activity was determined by autoanalyzer at National Taiwan University Hospital. Total protein was determined using total protein assay kit (BioRad Co.). Cytokine IL-6 protein and TNF-αwerealso determined using specific ELISA kit (R&D Systems, Minneapolis, MN).
Determination of total glutathione (GSH)
Quantitative colormetric determination of total glutathione of lung tissue were determined according to manufactures instructions (GSH-420, OxisResearch, U.S.A.). Briefly, lung tissues were homogenized in precipitation reagent at a ratio of 1 to 20 (w/v), then centrifuge homogenate at 3000 g for 10 minutes at 4 ℃. Upper aqueous layer was collected for assay. Internal calibrators ranged from 75 to 175μM.Theabsorbancewasmeasured using a spectrophotometric plate reader at 420 nm wavelength.
Determination of plasma 8-OHdG level
Plasma samples were used for the determination of 8-OHdG levels with a competitive ELISA kit (Japan Institute for the Control of Aging, Japan). The determination range was 0.5-200 ng/ml. The 8-OHdG monoclonal antibody and plasma sample were loaded at 50 l on a microtiter plate which has been coated with 8-OHdG, and incubated
instructions of the manufacturer. After washing, the antibodies that remained bound to the 8-OHdG in the sample were further bound with the horseradish peroxidase-conjugated secondary antibody. Subsequent addition of 3,3’,5,5’-tetramethylbenzidine resulted in the development of color intensity proportional to the amount of antibody bound to the plate. The color reaction was terminated by stop solution (phosphoric acid) and the absorbance was measured using a spectrophotometric plate reader at 450 nm wavelength.
Statistical analysis
SAS software package, version 8, was used for statistical analysis. Students’ t-test was used to analyze difference in each particle size and concentration. Type I error rate was set at 0.05 for significance.
Results
At both 100 and 50 μg/ml of IT particles caused significant increase in total cells in bronchoalveolar lavage and percentage of neutrophils with the 64-nm particles compared to the control and larger particle diameters (Fig 1, p < 0.05). In contrast, no significant effects were observed in 535-nm particles on total cells and percentage of neutrophils in both concentrations compared to the control.
An evident increase in bronchoalveolar lavage total protein and LDH activity in pulmonary hypertensiveratswith 100μg/mlof64-nm particles compared to the control and larger particle diameters (Fig 2, p < 0.05). No significant difference in size dependent effect was observed at treatment with 50μg/ml. Similar results were observed in bronchoalveolar laveage IL-6 protein and TNF-α(Fig 3).
Fig 4 showed that a significant depletion of totalGSH in lung tissuein ratswith 100μg/mlof 64-nm particles compared to the control groups. However, when all the GSH data were plotted against the surface area of particles instilled in the 100 and 50μg/ml dose, a decrease of GSH with increasing surface area was observed.
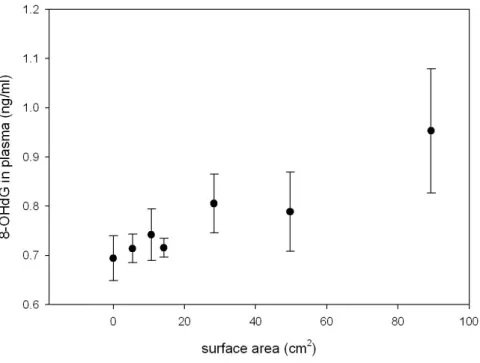
Fig 5 illustrated that all the 8-OHdG data plotted against the surface area of particles. Although the dose response relationship is not as a straight line, plasma 8-OHdG increased with the increasing surface area of particles instilled dose.
Cytokine level of A549 cell after polystyrene particle exposure was illustrated in Fig 6. We observed that ultrafine polystyrene particles induced higher levels of cytokine IL-8 as compared to
4
Discussion
The results showed that instillation with 100 and 50μg/ml of ultrafine polystyrene particle can induce increased inflammation compared to fine polystyrene particle at same mass concentration in pulmonary hypertensive rats. We also observed that ultrafine polystyrene demonstrate significant higher proinflammatory cytokine IL-6 and TNF-α as compared to fine particles. Furthermore, the result revealed that the depletion of total GSH and formation of plasma 8-OHdG were associated with surface area of particles instilled.
In order to investigate the effect of particle size and surface area, polystyrene microspheres have been used as a model of particle without complications of transition metals and chemical property. Recent studies have reported that inert ultrafine polystyrene have proinflammatory activity at high concentration in normal rats (Brown et al., 2001). Our study further demonstrated that ultrafine polystyrene can cause marked inflammation and lung injury at much lower dose in susceptible diseased animals.
Ultrafine particles have been shown to generate free radicals and induce oxidative stress (Donaldson et al., 1996; Stone et al., 1998; Brown et al., 2001). It is generally accepted that ultrafine particles cause inflammation through a cascade of interactions via oxidative stress or interactions with surface receptors on alveolar macrophages or epithelium cell to activate signal transcription (Churg A., 1996; Donladon et el., 2002). Furthermore, this study showed that the difference in oxidative stress was attributed to the surface area of the ultrafine particles. In addition to direct depletion of antioxidant GSH, the formation of 8-OHdG has been shown to increase with surface area instilled. A recent epidemiology study suggested that long-term exposure to combustion-related particle is an important risk factor for lung cancer mortality (Pope et al., 2002). A genotoxic effect of air particulate matters is also observed in an in vitro study (Carero et al., 2001). It is believed that surface properties of particulate matter play a critical role in its ability to form ROS, which are implicated in DNA damage and carcinogenesis. ROS such as hydrogen peroxide, superoxide anions and hydroxy radicals can directly or indirectly damage cellular DNA or protein. Among these ROS, the hydroxyl radicals are generally assumed to be the critical ROS that directly attack DNA. DNA damage caused by ROS includes DNA strand breaks (Hartwig et al., 2002) and base modifications, such as 8-OHdG (Lawrence, 2002). Our results provide evidence that surface area instilled of ultraifne particles are significant
associated with 8-OHdG, therefore, 8-OHdG may applied as an oxidative stress marker of ultrafine particle exposure.
In conclusion, we found inert ultrafine polystyrene may cause inflammatory effects on disease animals, and the formation of ROS was associated with instilled surface area dose. The exact mechanism warrants further study.
References
Brown D.M., Stone V., Findlay P., MacNee W., Donaldson K. Increased inflammation and intracellular calcium caused by ultrafine carbon black is independent of transition metals or other soluble components. Occup. Enviorn. Med. 57:685-691, 2000
Brown D.M., Wilson M.R., MacNee W., Stone V., Donaldson K. Size-dependent proinflammatory effects of ultrafine polystyrene particle: a role for surface area and oxidative stress in the enhanced activity of ultrafines. Toxicol. Appl. Phamacol. 175:191-199, 2001
Carero A DP., Hoet P.H.M., Verschaeve L., Schoeters G., Nemery B. Genotoxic effects of carbon black particles, diesel exhaust particles, and urban air particulates and their extracts on a human alveolar epithelial cell line (A549) and a human monocytic cell line (THP-1). Environ Mol Mutagen 37:155-163, 2001 Churg A. The uptake of mineral particles by
pulmonary epithelial cell. Am. J. Respir. Crit. Care Med. 154:1124-1140, 1996
Donaldson K., Beswich PH., Glimour PS., Free radical activity associated with the surface of particles: a unifying factor in determining biological activity? Toxicol Lett 88: 293-298, 1996
Donaldson K., Brown D., Clouter A., Duffin R., MacNee W., Renwick L., Tran L., Stone V. The pulmonary toxicology of ultrafine particles. J Aerosol Med 15:213-220, 2002
Dreher, K., Jaskot, R., Lehmann, J., Richards, J., McGee, J., Ghio, A., Costa, D. (1997). Soluble transition metals mediate residual oil fly ash induced acute injury, J Toxicol Environ Health 50, 285-305
Ferin J., Oberdorster G.., Penny D.P. Pulmonary retention of ultrafine and fine particle in rats. Am. J. Respir. Crit. Care Med. 6:535-543, 1992 Hartwig A. Role of DNA repair in paritlce- and fiber-induced lung injury. Inhal Toxicl. 14:91-100, 2002
Kodavanti, U. P., Costa, D. L., Bromnerg, P.A. (1998). Rodent models of cardiovascular disease: their potential applicability in studies of air pollutant susceptibility, Environ Health
Perspect 106 (suppl1), 111-130
Kodavanti, U. P., Jackson, M. C., Ledbetter, A. D., Richards, J. R., Gardner, S. Y., Watkinson. W. P., Costa, D. L. (1999). Lung injury from intrtracheal and inhalation exposures to residual oil fly ash in a rat model of monocrotaline-induced pulmonary hypertension, Toxicol Environ Health A 57, 543-563
Lawrence J.M. Oxyradicals and DNA damage. Carcinogenesis 21:361-370, 2000
Li X.Y., Brown D., Smith S., MacNee W., Donaldson K. Inflammatory responses following intratracheal instillation of fine and ultrafine carbon black in rats. Inhal Toxicol. 11:709-731, 1999
Loft S., Poulsen H.E, Cancer risk and oxidative DNA damage in man, J. Mol. Med. 74 :297-312, 1996
MacNee W., Li XY., Glimour PS., Donaldson K, Pro-inflammatory effect of particulate air pollution (PM10) in vivo and in vitro. Ann Occup Hyg 41 (Suppl I): 7-13, 1997
Meister A., and Anderson ME, Glutathione, Annual Review of Biochemistry, 52:711-760, 1983 Oberdorster G., Gelein R-M., Ferin J., Weiss B.
Association of particle air pollution and acute mortality: involvement of ultrafine paricles? Inhal Toxicl. 7:111-124, 1995
Oberdorster G., Pulmonary effects of inhaled ultrafine particles, Int Arch Occup Environ Health. 74:1-8, 2001
Pope III, C. A., Dockery, D. W. (1999). Epidemiology of particle effects. In: Air Pollution and Health (Holgate ST, Samet JM, Koren HS, Maynard RL, eds.). London: Academic Press 673-705.
Pope III, C. A., Burnett, R. T., Thun, M. J., Calle, E. E., Krewski, D., Ito, K. (2002). Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution, JAMA 287, 1132-1141.
Samet, J. M., Dominici, F., Curriero, F. C., Coursac, I., Zeger, S. L. (2000). Fine particulate air pollution and mortality in 20 U.S. cities, 1987-1994, N Engl J Med 343, 1742-1749. Stone V., Shaw J., Brown D.M., MacNee W., Faux
S.P., Donaldosn K. The role of oxidative stress in the prolonged inhibitory effect of ultrafine carbon black on epithelial cell function. Toxicology in Vitro 12:649-659, 1998
6
5.4cm
210.7cm
2535
14.2cm
228.3cm
2202
49.7cm
289.3cm
264
50μg
100μg
Diameter (nm)
Dose (μg/ml)
Surface area(cm
2)5.4cm
210.7cm
2535
14.2cm
228.3cm
2202
49.7cm
289.3cm
264
50μg
100μg
Diameter (nm)
Dose (μg/ml)
Surface area(cm
2) Table 1Fig 1
Total cells and percentage of neutrophils in bronchoalveolar lavage in pulmonary hypertensive ratsafterinstillation of100 and 50 μg/mlofpolystyreneparticles. (* p < 0.05)
Fig 2
Totalprotein and LDH activity in bronchoalveolarlavagein pulmonary hypertensiveratsafterinstillation of100 and 50 μg/mlofpolystyrene particles. (* p < 0.05) Particle (nm) 64nm 202nm 535nm control T o ta l c e lls in B A L (/ m l) 0 1x106 2x106 3x106 4x106 5x106 6x106 7x106 100ug/ml 50ug/ml PBS Particle (nm) 64nm 202nm 535nm control % o f n e u tr o p h ils 0.0 0.1 0.2 0.3 0.4 100ug/ml 50ug/ml PBS
*
*
*
*
X Data 64nm 202nm 535nm control T o ta l p ro te in in B A L (m g /m l) 0.0 0.2 0.4 0.6 0.8 100ug/ml 50ug/ml PBS Particle (nm) 64nm 202nm 535nm control L D H a c ti v it y (U /L ) 0 10 20 30 40 100ug/ml 50ug/ml*
*
8
Fig 3
Proinflammatory cytokine IL-6 and TNF-αin bronchoalveolarlavagein pulmonary hypertensiveratsafterinstillation of100 and 50 μg/mlofpolystyreneparticles. (* p < 0.05) Particle (nm) 64nm 202nm 535nm control IL -6 (p g /m l) 0 20 40 60 80 100 120 140 160 100ug/ml 50mg/ml Particle (nm) 64nm 202nm 535nm control T N F - 0 5 10 15 20 25 100ug/ml 50ug/ml
*
*
Fig 4
TotalGSH in lung tissueafterinstillation of100 and 50 μg/mlofpolystyreneparticlesin pulmonary hypertensiverats,and replotted againstinstillation surfacearea.
Particle (nm) 64nm 202nm 535nm control G S H (u M ) 0 500 1000 1500 2000 2500 3000 100ug/ml 50ug/ml
*
10
A549 cells treated for 4 h with polystyrene particles Particle (nm) control 64 109 202 IL -8 (p g /m l) 0 200 400 600 800 1000 Fig 6
12
奈米微粒與健康風險研究-子計畫五:疾病動物模式奈米微粒毒性探討
(II)(1/2)
計畫編號:NSC 92-2621-Z-002-014 執行期限:2003 年 8 月 1 日至 2004 年 7 月 31 日 主持人:鄭尊仁 國立台灣大學職業醫學與工業衛生研究所 計畫參與人員:雷侑蓁、鄭伊玲 國立台灣大學職業醫學與工業衛生研究所 中文摘要 近年來,許多流行病學研究指出,空氣污染 中氣懸微粒的增加,與呼吸系統疾病和心血管疾 病死亡率增加有關,這些死亡大都發生於已經有 心肺疾病的個人,然而確實致病機轉仍不清楚。 流行病學研究亦指出,長期暴露於懸浮微粒會增 加肺癌死亡的風險。相關研究指出,奈米微粒 (ultrafineparticle,<0.1μm)可能是呼吸與心血管疾 病死亡率及致病率增加的重要原因之一。根據微 粒成分與毒性研究顯示,相同重量下,同材質的 奈米微粒毒性較粗微粒高,可能與奈米微粒的數 目及總表面積皆較粗微粒高出許多,引起氧化壓 力相對較大有關;此外,奈米微粒在肺泡具有高 沈積率,亦具有穿透肺泡間質,經血液循環通透 至身體其他器官之特性,因此奈米微粒的暴露在 健康風險上扮演極重要之角色。近年,已有一些 研究針對奈米微粒與細胞毒性的關係進行探討, 主要著重在奈米微粒造成的發炎反應,但是對於 奈米微粒引起的呼吸道變化及心血管系統效應之 間的關係並不清楚。本研究目的為:(1)探討肺部 上皮內襯液體對於奈米微粒引起細胞氧化傷害的 影響,評估奈米微粒與細胞反應後產生之 ROS 及 評估細胞 DNA 單股斷裂情形。(2)以糖尿病大鼠 模式進行奈米微粒毒性試驗,以氣管灌注方式進 行 125 及 500μg/ml奈米碳黑暴露,觀察其肺部發 炎及周邊血液發炎反應、內皮細胞功能標記之變 化。研究結果顯示,在非細胞系統中,奈米碳黑 產生的 ROS 有隨暴露濃度及暴露時間增加呈現 上升的趨勢。碳黑微粒在添加 ELF 的環境下能顯 著降低 ROS 產生,同時,ELF 亦能減少 DNA 單 股斷裂的情形。在糖尿病大鼠模式中,我們發現 暴露於奈米碳黑導致顯著的肺部發炎及傷害反 應,奈米碳黑在糖尿病大鼠造成顯著的周邊發炎 反應增加,血管內皮素升高及血液一氧化氮降 低,奈米微粒暴露可能與糖尿病有共同的的病理 生理作用途徑,造成心血管疾病增加的風險。 關鍵詞:奈米微粒、糖尿病大鼠、肺部上皮內襯 液體、 反應性氧化物種、心肺疾病 AbstractEpidemiologic studies have shown consistent associations between the exposure to particulate air pollution and acute increase in morbidity and mortality, especially for susceptible subjects with pre-existing respiratory and cardiovascular disease. Furthermore, it has been reported that long-term exposure to combustion-related fine particles may be associated with lung cancer mortality. However, the exact mechanism remains unclear. It is believed that ultrafine particles may have a greater inflammatory effect than larger particles at the same mass concentration because of larger surface area and oxidative stress. In addition, ultrafine particles deposited in alveolar region may translocate into other organs. Thus, ambient ultrafine particles play critical role in health risk assessment. However, the role of ultrafine particles on cardiopulmonary events is not clear.
The goal of this study was: (1) to investigate the effect of epithelium lining fluids (ELF) on ultrafine particle-induced ROS generation. Ultrafine carbon black induced-ROS generation and DNA single strand breaks were evaluated. (2) to evaluate the effect of ultrafine carbon black on lung inflammation, systemic inflammation and endothelial dysfunction in STZ-diabetic rats. Our results revealed that in cell free system, the amounts of ROS increased with exposure concentration and exposure time. ELF significantly decreased ROS 90% as compared to culture medium after ufCB exposure. Furthermore, ELF also decreased DNA single-strand breakage after ufCB exposure. In diseased animal study, we found ufCB caused significant increase in pulmonary inflammation. We also observed significant alteration in systemic inflammation and endothelial dysfunction in diabetic rats exposed to ufCB. We suggest that ufCB
and diabetes may share the common pathway which may be related to cardiovascular events.
Keywords: ultrafine particles, diabetic rats, epithelium lining fluid, reactive oxygen species, cardiopulmonary disease
Introduction
Epidemiologic studies have shown consistent associations between the exposure to particulate air pollution and acute increase in morbidity and mortality, especially for susceptible subjects with pre-existing respiratory and cardiovascular disease (Pope and Dockery 1999; Samet et al., 2000; Pope et al., 2002). These epidemiologic studies also document that particles with a diameter below 2.5μm (PM2.5) have greater adverse health outcomes as compared to particles with a diameter below 10μm (PM10). Recent studies further indicate that the ultrafine particles (< 100 nm) may have an increased toxicity relative to larger particles under the same mass concentration (Ferin et al., 1992; Oberdorster et al., 1995; 2001). Many mechanisms of ultrafine particle-induced toxicity have been proposed, including greater number concentration, larger surface area and transition metals on particles (Oberdorster, 2001).
Since ultrafine particles have greater surface area compared to fine or coarse particles of same mass, greater reactive oxygen species (ROS) may be generated by the ultrafine particles. Ultrafine particles have been shown to generate ROS and cause oxidative stress (Stone et al., 1998). Several studies have demonstrated that ultrafine particles induce production of ROS both in vitro and in vitro (Stone et al., 1998; Wilson et al., 2002). Furthermore, various ultrafine particle have been demonstrated to generate more free radicals and ROS than fine particles (Stone et al., 1998; Wilson et al., 2000). Then, ROS may elicit transcription of proinflammatory cytokines and result in a cascade of inflammation events (Stone et al., 1998).
In order to investigate the effect of ultrafine particles on health effects, an in vitro study and an in vivo study were conducted in this report.
First, we investigated if airway lining fluid affects the ROS generated by ultrafine particle and subsequent DNA damage. Pulmonary epithelial lining fluid(ELF)consists of various antioxidants, which can protect lung cells against the oxidative damage of PM. However the exact mechanism remains unclear. The aim of this study was to determine the effect of ELF on PM-induced
susceptible subjects tend to have lower antioxidant in the peripheral blood and airway lining fluid. Animal studies also demonstrated that those deficient in antioxidants are more susceptible to PM exposure (Norwood et al., 2001). Those with deficiency in antioxidants are more likely to be affected by PM. Airway lining fluid contains antioxidants including Vitamin C and E and glutathione as well as enzymes including superoxide dismutase, glutathione peroxidase and catalase. Previous studies have shown that antioxidants in lining fluid decreased after PM exposure. Although the antioxidation effects have been demonstrated in cell free system, it is not clear if these changes also result in the reduction in the subsequent DNA damage. In this study, we investigated if airway lining fluid affects the ROS generated by ultrafine particle and subsequent DNA damage.
Second, we used diabetic rats to investigate the cardiovascular effect of ultrafine particles. The association between ambient particulate matter (PM) and cardiovascular diseases has been demonstrated in epidemiological studies (Pope and Dockery, 1999; Samet et al., 2000; Pope et al., 2002). Subjects with existing cardiovascular diseases including ischemic heart disease and congestive heart failure are found to be more susceptible to ambient PM exposure (Pope et al., 2002). Recently, some researchers have also suggested that diabetic patients are another sub-population at risk for PM-associated cardiovascular events (Goldberg et al., 2001; Zanobetti et al., 2001, 2002). Diabetes has been reported as an effect modifier of air pollution related hospital admissions for heart disease in elder person (Zanobetti et al., 2001), doubling the risk of a PM10-associated cardiovascular admission compared with non-diabetics (Zanobetti et al., 2002). Diabetes mellitus is a common disease, and has been associated with cardiovascular morbidity and mortality (Resnick et al, 2001). PM is also reported to affect cardiovascular diseases (Pope et al., 2004). However, the mechanisms through which ultrafine particle enhances the risks of cardiovascular disease in diabetics remain unclear. We hypothesize that diabetes and ultrafine particles may share common pathway and act synergistically in the development of cardiovascular diseases.
Hyperglycemia of diabetics has been associated with increased reactive oxygen species (ROS) formation (Maritim et al., 2003). Diabetic patients usually have significantly elevated concentrations of 8-OHdG in their serum (Nishikawa et al., 2003) and decreased levels of glutathione (GSH) (Dincer et al., 2002). It is proposed that increased ROS may induce inflammation in endothelium, alter endothelium function, and increase coagulability (Beckman et al.,
14
2002). Inflammation activity also increased in individuals with diabetes, as shown by increased levels of C-reactive protein (CRP) (Jager et al., 1999; Schalkwijk et al., 1999), interleukin-6 (IL-6)(Schram et al., 2003), and tumor necrosis factor (TNF-α) (Lechleitner et al., 2000). Hyperglycemia also inhibits the production of nitric oxide (NO) by blocking eNOS synthase activation and increasing the production of ROS in endothelial and vascular smooth muscle cells (De Vriese et al., 2000). In addition to reducing concentration of NO, diabetes increases the production of vasoconstrictors, most importantly, endothelin-1 (ET-1). Reports on endothelial dysfunction in patients with diabetes have been widely studied, including increased ET-1 and decreased NO (Haak et al., 1992; Williams et al., 1996).
The exact mechanisms through which ambient PM causes cardiovascular diseases remain unclear. PM exposure is associated with increased generation of ROS (Tao et al., 2003). It is proposed that PM may increase the oxidative stress related to cardiovascular disease in peripheral blood (Sorensen et al., 2003). PM exposure is also associated with elevated levels of C-reactive protein (Peters et al., 2001; Pope et al., 2003), enhanced production of proinflammatory cytokines (Ghio and Devlin 2001; Seaton et al., 1999; Schwartz 2001; Peters et al., 2001) and increased blood viscosity (Seaton et al., 1995; Peters et al., 1997) in epidemiological studies. In animal studies, the association between PM exposure and increased ET-1 has also been reported (Bouthillier et al., 1998; Vincent et al., 2001). It appears that PM and diabetes share common pathway in the development of cardiovascular diseases. Thus, we hypothesize exposure to PM may potentiate the cardiovascular diseases of diabetes through the enhanced production of oxidative stress and endothelial dysfunction.
In order to test the effects of ambient particles on diabetics, we exposed streptozotocin (STZ)-induced diabetic rats to PM. Streptozotocin is a metabolite of the soil organism streptomyces achromogenes and was first reported to be diabetogenic in studies of dogs and rats in 1963 (Bell et al., 1983). Diabetes is caused by a direct toxic effect of streptozotocin on the pancreatic beta cell. After the administration of streptozotocin, there is a characteristic increase in blood glucose, which is maintained at the level of 400mg/dL or greater. This diabetic animal model has been used in many studies of diabetes pathophysiology for years (Vural et al., 2002; Ryu et al., 2003; Zang et al., 2003)
Material and Methods
In vitro study Chemical reagents
Albumin (BSA), lysozyme (chicken egg white), apotransferrin (human), glutathione (GSH), uric acid (UA), α-tocopherol (AT), ascorbic acid (AA), catalase (CAT, bovine liver), superoxide dismutase (SOD, in bovine erythrocytes), glutathione peroxidase (GPx, bovine erythrocytes), Phosphatidylcholine (egg) , 2,7-dichlorofluorescin diacetate(DCFH-DA)were obtained from Sigma Chemical (St. Louis, MO). All chemicals were reagent grade or of higher purity.
A549 cell culture
The human A549 cell line was from American Type Culture Collection and cultured in a humidified 37oC environment in F12-K medium supplemented with 10% fetal calf serum and 1% penicillin and streptomycin. This cell line, derived from a patient with alveolar cell carcinoma of the lung, has been used as a model of human alveolar type II cells. A549 cells were cultured in six well transwell.
Particles preparation
The particles used in this study was ultrafine carbon black particles (14 nm, Degussa, Printex 90), suspended in culture medium in 50 and 150 μg/ml.
Preparation of ELF
ELF was formulated based on method of Guobin (2001) and Andre (1990). The components in ELF were listed in Table 1. Apotransferrin was used as a surrogate for lactoferrin because it has similar iron-binding qualities yet is more readily available. The following is the procedure for preparation of 100 ml of complete ELF. 1.0 ml of AT in chloroform (0.1 mg/ml) was added to a 100ml glass tube that contained 40ml idd water. The mixture was evaporated under nitrogen at room temperature. Next, 50 ml of medium were added, and the mixture was ultrasonicated in a water-ice bath., a solution of proteins (740 mg of albumin, 240 mg of lysozyme, and 20 mg of apotransferrin in 30 ml of medium) was added to this solution slowly. Finally, UA (0.5 mg/ml, 5.0 ml), AA (5 mg/ml, 1.0 ml), CAT(4 U/ml), SOD (40U/ml), GPx (0.05U/ml) and GSH (5 mg/ml, 1.0 ml) were added, and RPMI1640 was added to a final volume of 100 ml. The ELF was adjusted to pH 7.4 using NaOH (0.2 M) and H3PO4 (0.2 M).The ELFs were stored at -80°C.
Determination of ROS generation
Generation of ROS in the exposed solution of cell and free system was determined using the probe DCFH-DA(2,7-dichlorofluorescin diacetate). The
diacetate form of the probe is both lipid soluble and nonfluorescent. Incubation of DCFH-DA with serum containing medium results in cleavage of the diacetate group by esterase enzymes to yield a relatively lipid insoluble, nonfluorescent probe (DCFH). Subsequent oxidation of DCFH by ROS yields the highly fluorescent compound 2,7-dichlorofluorescein (DCF), which can be quantified by microplate reader with excitation wavelength at 485nm(bandwidth 20nm)and an emission wavelength at 530 nm(bandwidth 25nm) DCFH-DA (final concentration 20M) was incubated for 15 min at 37°C in cell culture medium (10% FBS) in order to cleave the DCFH-DA precursor to DCFH. Suspensions of particles were prepared in RPMI1640 medium, mixed by vortexing, and then sonicated for 10 min. After exposure of the DCFH to the particles for 30 min(37℃),DCF fluorescence intensity was determined by Cytofluor 2300 microplate reader (Millipore, Bedford, MA, USA).
Determination of DNA single strand breaks by comet assay
Quantitiesof20 μlofA549 suspensions(105 cells/ml) were mixed with 1 ml 1.5% low melting agarose and gelled to frost slides pretreated with 0.1 % normal melting agarose on ice. After gelling, the slides were immersed in lysis buffer then washed with PBS. They were then placed in alkaline buffer for electrophoresisat 21 V and 190 mA for 20 min. Slides were rinsed and stained in sybr green. Individual cells were examined under microscope with photomicrographic system. All slides were coded and read blindly. The images were then recorded for further image analysis.
A proprietary image processing software, which has been used in previous studies (Ma et al., 1996) was applied to calculate the distribution of DNA on the agarose. Images of 100 randomly selected cells from each set of experiment were analyzed under a fluorescence microscope adapted with an excitation of 515-560 nm and a barrier filter of 590 nm. Parameters used in the analysis were tail length (%), tail intensity (%) and tail moment. Tail length (%) was defined as the propertion of tail length in whole comet length, tail intensity (%) was defined as the proportion of tail intensity in total comet intensity, and tail moment was defined as the product of tail length and tail intensity. We used % of the tail length and intensity because of their ease in measurement (Ma et al., 1996).
In vivo studies Particles preparation
The particles used in this study was ultrafine carbon black particles (14 nm, Degussa, Printex 90), μg/ml
Diabetic animals and intratracheal instillation of ufCB
Male Sprague-Dawley rats, weighing 200~250 g, were obtained from the National Laboratory Animal Breeding and Research Center, Taiwan. They were housed in plastic cages on Aspen chip bedding, and provided with Lab Diet 5001, water ad lib, except during the exposure. Animals were maintained on a 12-hour light/dark cycle at 22 + 1C and 55 + 10 % relative humidity. A single intraperitoneal (IP) injection of streptozotocin (STZ, Sigma Chemical Co., 60mg/kg body weight, dissolved in citric acid buffer, pH 4.5) was administered to eight animals to induce diabetes (Bell et al., 1983). Rats were randomly divided into ultrafine carbon black exposure groups (125 and 500 μg/ml)and controlgroup (PBS).Allprotocols used in this experiment were approved by National Taiwan University’sanimalcareand usecommittee.
Bronchoalveolar lavage analysis
Rats were sacrificed 24h after intratracheal instillation. BAL fluid was collected by washing the airway with a phosphate-buffered saline solution (PBS, pH = 7.4, 28 ml/kg body weight) five times. Lavage fluid was used to determine the total number of cells and cell differential counts. Macrophage, lymphocyte, neutrophils, eosinophils and basophiles were counted under light microscopy (200 cells/slide). The remaining lavage fluid was used for the analysis of total protein and LDH activity. LDH activity was determined by autoanalyzer at National Taiwan University Hospital. Total protein was determined using total protein assay kit (BioRad Co.)
Determination of blood glucose, oxidative stress, inflammation and endothelial dysfunction
A total of 15 ml whole blood was recovered from aorta. Immediately, 1 ml of whole blood was collected in citrate tube for blood glucose analysis using autoanalyzer (Glucometer 3, blood glucose meter; Miles Inc.) at National Taiwan University Hospital. 10ml whole blood was collected in ethylenediamine tetraacetic acid (EDTA) tubes. After centrifuged at 1200 rpm for 10 minutes, plasma aliquots were stored at -80℃until analysis. The remaining 4 ml whole blood was collected in glass tube. Circulating inflammation markers were represented by cytokine IL-6 and TNF-α. Plasma levels of IL-6 and TNF-α were measured using ELISA kits (R&D Systems, U.S.A). Plasma ET-1 and NO were used to represent endothelial function. ET-1 was measured by ELISA (R&D Systems) with human ET-1 as standard (Bouthillier et al., 1998). Nitric oxide synthase assay kit with the Griess
16
reagent (CALBIOCHEM Inc., U.S.A.) was used to determine plasma NO. The plasma concentration of NO was calculated as the sum of nitrite (NO2-) and nitrate (NO3-) concentrations.
Statistical analysis
SAS software package, version 8, was used for statistical analysis.
Results and Discussion
In vitro studies
Ultrafine carbon black (UfCB) induced a significant increase in DCF fluorescence at 50 and 150μg/ml as compared to control (Figure 1, p < 0.05).Similarly,A549 cellsexposed to 50μg/mlor 150μg/ml, and then incubated with DCFH for 30 min, exhibited a significant greater fluorescence than control (Figure 1, p<0.05). In cell-free system and with A549, ELF addition result in significant decrease in DCF fluorescence induced by UfCB (Figure 1). Further, increasing oxidative DNA damage was observed with increased UfCB concentration (figure 2). Again, with ELF, the oxidative DNA damage was reduced. Our results found that UfCB could induce ROS in cell free system. It appears that surface of UfCB may react with water and induced ROS, which can cause DNA damage in A549 cells. Because ELF can decrease total ROS and DNA damage induced by UfCB, this further supports that ROS plays an important role in ultrafine particles related toxicity. However, the exact mechanisms through which ultrafine particles induce toxicity needs further study.
In vivo studies
Characteristics of study animals were described in Table 2. Body weight of diabetic rats was lower than that of non-diabetic rats (510.5 g vs. 580.2 g). The mean plasma glucose level was 150.5 mg/dl in non-diabetic rats, and 350.5 mg/dl in diabetic rats (p < 0.05).
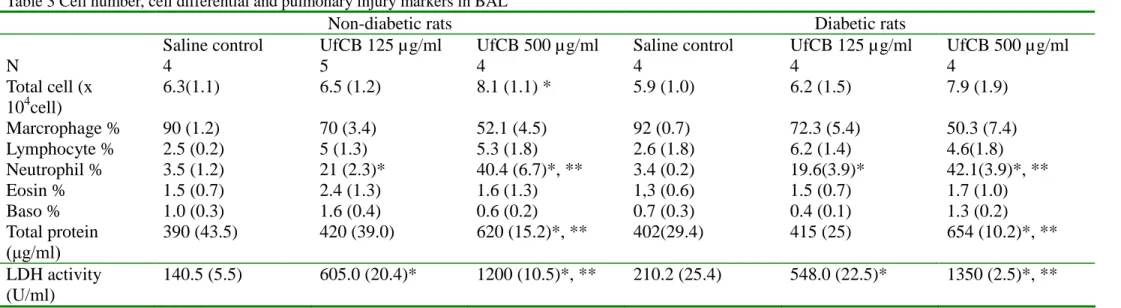
Diabetes had no effect on total cells, percentage of neutrophils, total protein and LDH activity in BAL (Table 3). In plasma analysis, diabetic rats demonstrated significantly greater cytokine IL-6 as compared with non-diabetic rats (p <0.05). Furthermore, diabetic rats had significantly increased level of plasma ET-1 (p < 0.05), and decreased level of plasma NO (p < 0.05).
In non-diabetic rats, ufCB caused significant increases in total cells and proportion of neutrophils in bronchoalveolar lavage (Table 3, p < 0.05). Elevated total protein and LDH activity in bronchoalveolar lavage were also observed after ufCB exposure (p<0.05). Plasma IL-6 level also showed significant increase after ufCB exposure
(Table 4, p < 0.05). Furthermore, ufCB exposure caused a significant reduction of plasma NO (p<0.05). However, there was no significant ufCB effect on plasma ET-1 in non-diabetic rats.
In STZ-diabetic rats, significant increases in pulmonary inflammation and injury markers were observed after ufCB exposure (Table 3, p<0.05). Plasma IL-6 and cytokine TNF-α significantly increased in diabetic rats after exposure to ufCB (Table 4, p < 0.05). In assessing endothelial function, we found a significant elevation of plasma ET-1 and a significant decrease in plasma NO after exposure to ufCB (p < 0.05).
Similar findings were observed in our previous study in which, CAPs enhanced the endothelial dysfunction in diabetic rats as compared to non-diabetic rats. In this study, we further observed that ultrafine particles have similar effects. It is not clear whether ultrafine particles penetrate into circulation then directly cause endothelial dysfunction, or indirectly affect endothelium as a result of lung inflammation. Thus, more studies are needed to investigate the underlying mechanisms. We conclude that ufCB exposure may enhance the risk of cardiovascular diseases through the synergistic interaction between ufCB and diabetes in endothelium.
References
Andre M. Cantin, Gerald A. Fells, Richard C. Hubbard, and Ronald G. Crystal.1990 Antioxidant macromolecules in the epithelial lining fluid of the normal human lower respiratory tract. The Journal of Clinical Investigation.86:962-971.
Amos AF, McCatry DJ, Zimmet P. 1997. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med. 14 (suppl 5):S1-S85.
Batalha JR, Saldiva PH, Clarke RW, Coull BA, Stearns RC, Lawrence J, Murthy CG, Koutrakis P, Godleski JJ. 2002 Concentrated ambient air particles induce vasoconstriction of small pulmonary arteries in rats. Environ Health Perspect. 110:1191-1197
Backes JM, Howard PA, Moriarty PM. 2004. Role of C-reactive protein in cardiovascular disease.Ann Pharmacother 38:110-118.
Becher R, Hetland RB, Refsnes M, Dahl JE, Dahlman HJ, Schwarze PE. 2001 Rat lung inflammatory responses after in vivo and in vitro exposure to various stone particles. Inhal Toxicol. 13:789-805.
Beckman JA, Creager MA, Libby P. 2002. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 15:
287:2570-2581.
Bell RH, Hye RJ.1983. Animal models of diabetes mellitus: physiology and pathology. J Surgical Res 35:433-460.
Blackford JA Jr, Jones W, Dey RD, Castranova
V.
1997. Comparison of inducible nitric oxide synthase gene expression and lung inflammation following intratracheal instillation of silica, coal, carbonyl iron, or titanium dioxide in rats. J Toxicol Environ Health.51:203-218.Blake GJ, Ridker PM. 2002. Inflammatory bio-markers and cardiovascular risk prediction. J Intern Med. 252:283-294.
Bouthillier L, Vincent R, Goegan P, Adamson IY, Bjarnason S, Stewart M, Guenette J, Potvin M, Kumarathasan P. 1998. Acute effects of inhaled urban particles and ozone: lung morphology, macrophage activity, and plasma endothelin-1. Am J Pathol. 153:1873-1884.
Clarke R. W, Catalane, PJ, Koutrakis P, Krishna M, Sioiutas C, Paulauskis SJ. 1999. Urban air particulate inhalation alters pulmonary function and induces pulmonary inflammation in a rat model of chronic bronchitis. Inhal Toxicol 11: 637-656.
Catheart R., Schwiers E., Ames BN.(1983) Detection of picomole levels of hydroperoxides using fluorescent dichlorofluorescein assay. Anal. Biochem.134:111-6.
Clarke RW, Coull B, Reinisch U, Catalano P, Killingsworth CR, Koutrakis P, Kavouras I, Murthy GG, Lawrence J, Lovett E, Wolfson JM, Verrier RL, Godleski JJ. 2000. Inhaled concentrated ambient particles are associated with hematologic and bronchoalveolar lavage changes in canines. Environ Health Perspect. 108:1179-87.
De Vriese AS, Verbeuren TJ, Van de Voorde J, Lameire NH, Vanhoutte PM. 2000. Endothelial dysfunction in diabetes. Br J Pharmacol. 130:963-974.
Dincer Y, Akcay T, Alademir Z, Ilkova H. 2003. Assessment of DNA base oxidation and glutathione level in patients with type 2 diabetes. Mutat Res.525:129-130.
Ghio AJ, Devlin RB. 2001. Inflammatory lung injury after bronchial instillation of air pollution particles. Am J Respir Crit Care Med.164:704-708.
Goldberg MS, Burnett RT, Bailar JC III, et al., 2001. The association between daily mortality and ambient air particle pollution in Montreal, Quebec. 2. Cause-specific mortality. Environ Res. 86:26-36.
Gordon T., Nadziejko C, Schlesinger R, Chen LC, 1998. Pulmonary and cardiovascular effects of
acute exposure to concentrated ambient particulate matter in rats. Toxicol. Letters. 96, 97: 285-288.
Guzik TJ, Korbut R, Adamek-Guzik T 2003. Nitric oxide and superoxide in inflammation and immune regulation. J Physiol Pharmacol. 54:469-487.
Haak T, Jungmann E, Felber A, Hillmann U, Usadel KH. 1992. Increased plasma levels of endothelin in diabetic patients with hypertension. Am J Hypertens. 5:161-166. Jager A, van Hinsbergh VW, Kostense PJ, Emeis JJ,
Yudkin JS, Nijpels G, Dekker JM, Heine RJ, Bouter LM, Stehouwer CD. 1999. von Willebrand factor, C-reactive protein, and 5-year mortality in diabetic and nondiabetic subjects: the Hoorn Study. Arterioscler Thromb Vasc Biol. 19:3071-3078.
Keston. A. S., and R. Brandt. 1965. The fluorometric analysis of ultramicro quantities of hydrogen peroxide. Anal. Biochem. 11 :1. Lechleitner M, Koch T, Herold M, Dzien A,
Hoppichler F. 2000. Tumour necrosis factor-alpha plasma level in patients with type 1 diabetes mellitus and its association with glycaemic control and cardiovascular risk factors. J Intern Med. 248:67-76.
Lerman A, Edwards BS, Hallett JW, Heublein DM, Sanberg SM, Burnett JC. 1991. Circulating and tissue endothelin immunoreactivity in advanced atherosclerosis. N. Engl J Med 325: 997-1001.
Lei YC, Chan CC, Wang PY, Lee CT, Cheng TJ. 2004. Effects of dust storm particles on inflammation markers in peripheral blood and bronchoalveolar lavage in pulmonary hypertensive rats. Environ Res. 95:71-76. Martin R. Wilson, Janet H. Lightbody, Ken
Donalson, Jill Sales, Vicki Stone. ( 2002 ) Interaction between ultrafine particle and transition metals in vivo and in vitro. Toxicology and Applied Pharmacology 184: 172-179.
Maritim AC, Sanders RA, Watkins JB. 2003. Diabetes, oxidative stress, and antioxidants: a review. J Biochem Mol Toxicol. 17:24-38. Michael JR, Markewitz BA. 1996. Endothelins and
the lung. Am J Respir Crit Care Med 154: 555-581.
Nemmar A, Vanbilloen H, Hoylaerts MF, Hoet PH, Verbruggen A, Nemery B. 2001. Passage of intratracheally instilled ultrafine particles from the lung into the systemic circulation in hamster. Am J Respir Crit Care Med. 164:1665-1668.
Nemmar A, Hoet PH, Vanquickenborne B, Dinsdale D, Thomeer M, Hoylaerts MF, Vanbilloen H,
18
Mortelmans L, Nemery B. 2002. Passage of inhaled particles into the blood circulation in humans. Circulation. 105:411-414.
Nishikawa T, Sasahara T, Kiritoshi S, Sonoda K, Senokuchi T, Matsuo T, Kukidome D, Wake N, Matsumura T, Miyamura N, Sakakida M, Kishikawa H, Araki E. 2003. Evaluation of urinary 8-hydroxydeoxy-guanosine as a novel biomarker of macrovascular complications in type 2 diabetes. Diabetes Care. 26:1507-1512. Packer R, Bergler-Klein J, Globits S, Teufelsbauer
H, Schuller M, Krauter A, Ogris E, Rodler S, Wutte M, Hartter E. 1993. Plasma big endothelin-1 concentrations in or congestive heart failure patients with or without systemic hypertension. Am J Cardiol 71: 1293-1299. Peters A, Doring A, Wichmann HE, Koenig W. 1997.
Increased plasma viscosity during the1985 air pollution episode: a link to mortality? Lancet 349:1582-1587.
Peters A, Frohlich M, Doring A et al., 2001. Particulate air pollution is associated with an acute phase response in men: results from the MONICA-Augsbrug study. Eur Heart J 22:1198-1204.
Pickup JC. 2004. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care 27:813-823.
Pope III CA, Dockery DW. 1999. Epidemiology of particle effects. In: Air Pollution and Health (Holgate ST, Samet JM, Koren HS, Maynard RL, eds.). London: Academic Press 673-705. Pope III CA, Burnett RT, Thun MJ, Calle EE,
Krewski D, Ito K.2002.Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution, JAMA 287: 1132-1141.
Pope III CA , Hansen ML, Long RW, Nielsen KR, Eatough NL, Wilson WE, Eatough DJ. 2004. Ambient particulate air pollution, heart rate variability, and blood markers of inflammation in a panel of elderly subjects. Environ Health Perspect. 112:339-345.
Prahalad AK, Soukup JM, Inmon J, Willis R, Ghio AJ, Becker S, Gallagher JE. 1999. Ambient air particles: effects on cellular oxidant radical generation in relation to particulate elemental chemistry. Toxicol Appl Pharmacol. 158:81-91. Rankin JA. 2004. Biological mediators of acute
inflammation. AACN Clin Issues. 15:3-17. Resnick HE, Howard BV. 2002. Diabetes and
cardiovascular disease. Annu Rev Med. 53:245-267.
Ryu JK, Kim DJ, Lee T, Kang YS, Yoon SM, Suh JK. 2003. The role of free radical in the pathogenesis of impotence in streptozotocin-induced diabetic rats. Yonsei
Med J. 44:236-241,
Samet JM, Dominici F, Curriero FC, Coursac I, Zeger SL. 2000. Fine particulate air pollution and mortality in 20 U.S. cities, 1987-1994, N Engl J Med 343: 1742-1749.
Schalkwijk CG, Poland DC, van Dijk W, Kok A, Emeis JJ, Drager AM, Doni A, van Hinsbergh VW, Stehouwer CD. 1999. Plasma concentration of C-reactive protein is increased in type I diabetic patients without clinical macroangiopathy and correlates with markers of endothelial dysfunction: evidence for chronic inflammation. Diabetologia. 42:351-357
Schiffrin EL, Intengan HD, Thibault G, .Touyz RM. 1997. Clinical significance of endothelin in cardiovascular disease. Curr Opin Cardiol 12:354-367.
Schram MT, Chaturvedi N, Schalkwijk C, Giorgino F, Ebeling P, Fuller JH, Stehouwer CD; EURODIAB Prospective Complications Study. 2003. Vascular risk factors and markers of endothelial function as determinants of inflammatory markers in type 1 diabetes: the EURODIAB Prospective Complications Study. Diabetes Care.26:2165-2173.
Schwartz J. 2001. Air pollution and blood markers of cardiovascular risk. Environ Health Perspect 109:405-409.
Seaton A, MacNee W, Donaldon K, Godden D. 1995. Particulate air pollution and acute health effects. Lancet 345: 176-178.
Seaton A, Soutar A, Crawford V, Elton R, McNerlan S, Cherrie J, Watt M, Agius R, 1999. Stout R.Particulate air pollution and the blood. Thorax. 54: 1027-1032.
Sioutas C, Kim S, Chang M. 1999. Development and evaluation of a prototype ultra-fine particle concentrator, J Aerosol Med 30:1001-1017. Sorensen M, Daneshvar B, Hansen M, Dragsted LO,
Hertel O, Knudsen L, Loft S. 2003. Personal PM2.5 exposure and markers of oxidative stress in blood. Environ Health Perspect. 111:161-166.
Spranger J, Kroke A, Mohlig M, Hoffmann K, Bergmann MM, Ristow M, Boeing H, Pfeiffer AF. 2003. Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Diabetes. 52:812-817.
Sun, Guobin, Kay Crissman, Joel Norwood, Judy Richards, Ralph Slade, and Gary E. Hatch. Oxidative interactions of synthetic lung epithelial lining fluid with
Lung Cell Mol Physiol 281: L807–L815, 2001. Tao F, Gonzalez-Flecha B, Kobzik L. 2003.
Reactive oxygen species in pulmonary inflammation by ambient particulates. Free Radical biology and medicine 35:327-340.
Zang L, Zalewski A, Liu Y, Mazurek T, Cowan
S, Martin JL, Hofmann SM, Vlassara H,
Shi Y.
2003. Diabetes-induced oxidative stress and low-grade inflammation in porcine coronary arteries. Circulation. 108:472-478. Zanobetti A, Schwartz J, Gold DR. 2001. Arediabetes more susceptible to the health effects of airborne particles? Am J Respir Crit Care Med 164:831-833.
Zanobetti A, Schwartz J. 2002. Cardiovascular damage by airborne particles: are diabetes more susceptible? Epidemiology 13:588-592. Ulrich MM, Alink GM, Kumarathasan P, Vincent R,
Boere AJ, Cassee FR. 2002. Health effects and time course of particulate matter on the cardiopulmonary system in rats with lung inflammation. J Toxicol Environ Health A 25;65:1571-1595.
Vincent R, Kumarathasan P, Goegan P, Bjarnason SG, Guenette J, Berube D, Adamson IY, Desjardins S, Burnett RT, Miller FJ, Battistini B. 2001. Inhalation toxicology of urban ambient particulate matter: acute cardiovascular effects in rats. Res Rep Health Eff Inst. (104):5-54; discussion 55-62.
Vural P, Cevik A, Curgunlu A, Canbaz M. 2002. Effects of diabetes mellitus and acute hypertension on plasma nitric oxide and endothelin concentrations in rats. Clin Chim Acta. 320:43-47.
Williams SB, Cusco JA, Roddy MA, Johnstone MT, Creager MA. 1996. Impaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J Am Coll Cardiol.27:567-574.
Wilson MR, Lightbody JH, Donaldson K, Sales J, Stone V. 2002. Interactions between ultrafine particles and transition metals in vivo and in vitro. Toxicol Appl Pharmacol. 184:172-179.
20
Table 1 components and concentrations of ELFs
Constituents of synthetic lung epithelial ling fluid
components
concentration
Serum albumin, mg/ml
7.4
Phosphatidylcholine (egg), mg/ml
10
Lysozyme, mg/ml
2.5
Apotransferrin , mg/ml
0.2
Ascorbic acid ( AA),
g/ml
50
Gl
ut
a
t
hi
one
r
e
duce
d
(
GSH)
,
g/
ml
50
Ur
i
c
a
c
i
d
(
UA)
,
g/
ml
25
a-tocopherol (AT),
g/ml
1
Catalase, U/ml
4
Glutathione peroxidase (GPx) U/ml
0.05
Figure 1
Effect of ultrafine carbon black on the oxidation of DCFH to DCF in (a) a cell free system, (b) a A549 cells system with orwithoutELF.* p<0.05 compared to control;**p<0.05 compared to 50μg/ml.
M e a n F lu o re s c e n c e 0 100 200 300 400 500 600 control 50g/ml ufCB 150g/ml ufCB (a) cell free system
ELF non-ELF 0.3 5.6 373 400 (b) cell system * * ** * M e a n F lu o re s c e n c e 0 100 200 300 400 500 600 control 50g/ml ufCB 150g/ml ufCB ELF non-ELF 3.3 9.1 41.2 83.7
22 ELF non-ELF ta il m o m e n t 0 100 200 300 400 500 600 control 50ug/ml ufCB 150ug/ml ufCB (c) DNA SSB 21.6 30.6 2.12 0.4 Figure 2
Table 2 Basic characteristics of experimental animals
Non-diabetic rats (n=13)
STZ-diabetic rats (n=12)
Body weight (g)
510.5±8.3
580.2±29.7*
Blood glucose (mg/dL)
150.5±9.7
350.5±9.7*
* Mean + standard deviation, * p<0.05 as compared to non-diabetic rats Table 3 Cell number, cell differential and pulmonary injury markers in BAL
Non-diabetic rats
Diabetic rats
Saline control
UfCB 125 µg/ml
UfCB 500 µg/ml
Saline control
UfCB 125 µg/ml
UfCB 500 µg/ml
N
4
5
4
4
4
4
Total cell (x
10
4cell)
6.3(1.1)
6.5 (1.2)
8.1 (1.1) *
5.9 (1.0)
6.2 (1.5)
7.9 (1.9)
Marcrophage %
90 (1.2)
70 (3.4)
52.1 (4.5)
92 (0.7)
72.3 (5.4)
50.3 (7.4)
Lymphocyte %
2.5 (0.2)
5 (1.3)
5.3 (1.8)
2.6 (1.8)
6.2 (1.4)
4.6(1.8)
Neutrophil %
3.5 (1.2)
21 (2.3)*
40.4 (6.7)*, **
3.4 (0.2)
19.6(3.9)*
42.1(3.9)*, **
Eosin %
1.5 (0.7)
2.4 (1.3)
1.6 (1.3)
1,3 (0.6)
1.5 (0.7)
1.7 (1.0)
Baso %
1.0 (0.3)
1.6 (0.4)
0.6 (0.2)
0.7 (0.3)
0.4 (0.1)
1.3 (0.2)
Total protein
(
μg/
ml
)
390 (43.5)
420 (39.0)
620 (15.2)*, **
402(29.4)
415 (25)
654 (10.2)*, **
LDH activity
(U/ml)
140.5 (5.5)
605.0 (20.4)*
1200 (10.5)*, **
210.2 (25.4)
548.0 (22.5)*
1350 (2.5)*, **
* p<0.05 as compared to each saline control** p<0.05 as compared to 125 µg/ml exposure group Table 4
Systemic inflammatory and endothelial dysfunction markers in plasma
Non-diabetic rats
Diabetic rats
Saline control
125 µg/ml
500 µg/ml
Saline control
125 µg/ml
500 µg/ml
N
4
5
4
4
4
4
Systemic
inflmmation
Plasma IL-6
(pg/ml)
30.5 (8.1)
39.8 (4.5)
50.2 (2.7) *, **
41.2 (5.2)
50.8 (4.7)
65.0 (7.5) *
24
Plasma TNF-α
(pg/ml)
4.6 (2.5)
4.3 (3.2)
6.8 (1.1)
5.1 (1.2)
4.9 (1.5)
8.2 (0.7) *, **
Endothelial
dysfunction
Plasma ET-1
(pg/ml)
Plasma NO (µM)
1.3 (0.5)
89.4 (4.7)
1.9 (0.4)
90.5 (1.8)
2.0 (0.8)
85.8 (5.0)
1.9 (0.3)
80.5 (2.0)
2.1 (0.7)
75.2 (3.9)
2.9 (0.1)*
72.2 (1.5)*
* p<0.05 as compared to each saline control