Chinese herbal medicine treatment improves the overall
survival rate of individuals with hypertension among type 2
diabetes patients and modulates in vitro smooth muscle cell
contractility
Short title: Chinese herbal medicine and type 2 diabetes
Ying-Ju Lin1,2¶, Tsung-Jung Ho1,3,4¶, Yi-Chun Yeh5, Chi-Fung Cheng5, Yi-Tzone Shiao6,
Chang-Bi Wang5, Wen-Kuei Chien7, Jin-Hua Chen7,8, Xiang Liu9, Hsinyi Tsang9, Ting-Hsu
Lin2, Chiu-Chu Liao2, Shao-Mei Huang2, Ju-Pi Li1,10, Cheng-Wen Lin11, Hao-Yu Pang11,
Jaung-Geng Lin1, Yu-Ching Lan12 , Yu-Huei Liu2,13 , Shih-Yin Chen1,2 , Fuu-Jen Tsai1,2,14*,
Wen-Miin Liang5*
1 School of Chinese Medicine, China Medical University, Taichung, Taiwan, 2 Genetic
Center, Department of Medical Research, China Medical University Hospital, Taichung, Taiwan, 3 Division of Chinese Medicine, China Medical University Beigang Hospital, Yunlin, Taiwan, 4 Division of Chinese Medicine, Tainan Municipal An-Nan Hospital-China Medical University, Tainan, Taiwan, 5 Graduate Institute of Biostatistics, School of Public Health, China Medical University, Taichung, Taiwan, 6 Heart Center, China Medical University Hospital, Taichung, Taiwan, 7 Biostatistics Center, College of Management, Taipei Medical University, Taipei, Taiwan, 8 School of Health Care Administration, College of Management, Taipei Medical University, Taipei, Taiwan, 9 National Institute of Allergy
and Infectious Diseases, National Institutes of Health, Bethesda, Maryland, USA, 10 Rheumatism Research Center, China Medical University Hospital, Taichung, Taiwan, 11 Department of Medical Laboratory Science and Biotechnology, China Medical University, Taichung, Taiwan, 12 Department of Health Risk Management, China Medical University, Taichung, Taiwan, 13 Graduate Institute of Integrated Medicine, China Medical University, Taichung, Taiwan, 14 Asia University, Taichung, Taiwan
¶Ying-Ju Lin and Tsung-Jung Ho contributed equally to this work.
* Correspondence to Drs Fuu-Jen TSAI and Wen-Miin LIANG, No. 2, Yuh-Der Road,
Taichung, Taiwan. Tel: +886 22062121; fax: +886 22033295; e-mail: d0704@mail.cmuh.org.tw; wmliang.cmu@gmail.com
Abstract
Type 2 diabetes (T2D) is a chronic, multifactorial, and metabolic disorder accounting for 90% diabetes cases worldwide. Among them, almost half of T2D have hypertension, which is responsible for cardiovascular disease, morbidity, and mortality in these patients. The Chinese herbal medicine (CHM) prescription patterns of hypertension individuals among T2D patients have yet to be characterized. This study, therefore, aimed to determine their prescription patterns and evaluate the CHM effect. A cohort of one million randomly sampled cases from the National Health Insurance Research Database (NHIRD) was used to investigate the overall survival rate of CHM users, and prescription patterns. After matching CHM and non-CHM users for age, gender and date of diagnosis of hypertension, 980 subjects for each group were selected. The CHM users were characterized with slightly longer duration time from diabetes to hypertension, and more cases for hyperlipidaemia. The cumulative survival probabilities were higher in CHM users than in non-CHM users. Among these top 12 herbs, Liu-Wei-Di-Huang-Wan, Jia-Wei-Xiao-Yao-San, Dan-Shen, and Ge-Gen were the most common herbs and inhibited in vitro smooth muscle cell contractility. Our study also provides a CHM comprehensive list that may be useful in future investigation of the safety and efficacy for individuals with hypertension among type 2 diabetes patients.
Introduction
Type 2 diabetes (T2D) is a chronic, multifactorial, and metabolic disorder and accounts for 90% of those with diabetes worldwide [1]. In Asia and the eastern Pacific region, China was home to the largest number of adults with diabetes (i.e. 90.0 million, or 9% of the population), followed by India (61.3 million, or 8% of the population) and Bangladesh (8.4 million, or 10% of the population) [2-4]. In Taiwan, T2D is one of the top 10 leading causes of death, suggesting that this disease is one of the most important health problems today. T2D is characterized by abnormally high levels of blood glucose resulting from impaired pancreatic β cell function, decreased insulin sensitivity in target tissues, and increased glucose output from the liver [5, 6]. Chronic hyperglycemia causes multiple organ damage and failure, affecting sites including the blood vessels and heart, eyes, kidneys, and nerves. Diabetes related cardiovascular disease, retinopathy, nephropathy, neuropathy, and peripheral circulatory disorders are believed to be responsible for the symptoms, signs, ill-defined secondary conditions, and mortality observed in patients with diabetes.
Hypertension (high blood pressure, usually > 130/80 mmHg) is very common among T2D patients. Almost half of T2D patients have high blood pressure, which doubles their risk of cardiovascular disease [7, 8]. Diabetes related cardiovascular diseases are believed to be responsible for the high morbidity and mortality rates of this condition [9]. In prospective studies, blood pressure control was twice as effective as glucose control in
preventing diabetes related cardiovascular disease [10-13]. Therefore, both control of blood pressure and glucose levels in order to prevent substantial diabetic related complications and mortality continues to be an important public health concern.
In diabetic patients, significant improvements can be achieved by lifestyle modification [14] and treatment with hypoglycemic or anti-hyperglycemic, insulin sensitizing, and insulin secretion enhancing agents [15-17]. However, side effects are still frequently reported when using these therapeutic regimes. Meta-analyses show increased cardiovascular and mortality risk when using metformin, sulfonylurea, and thiazolidinediones [15-18]. Long-term thiazolidinedione use increases the risk of fracture, lower respiratory tract infection, and bladder cancer among those with diabetes [17, 19, 20]. These reports have prompted the search for alternative and complementary therapies for better management of diabetes and its related complications. Chinese herbal medicine (CHM) has been used in clinical practice for clinical, chronic, and irreversible diseases for hundreds of years. It has also been used in the management of diabetes, as well as diabetes related complications and mortality [21-23].
CHM is an important aspect of health care in Taiwan and is provided by licensed traditional Chinese medicine (TCM) doctors. It has also been covered under the National Health Insurance (NHI) program since 1996 [24, 25]. Residents in Taiwan are able to choose regular medical treatments, CHM, or both. All claims are collected by the National
Health Insurance Research Database (NHIRD). Therefore, this claim database can be used as a platform to explore the utilization and therapeutic effects of Chinese herbal therapies prescribed by these TCM doctors in Taiwan. The characteristics of TCM use in Taiwan have been investigated by population-based studies for several diseases including childhood asthma [26], breast cancer [27], chronic kidney disease [28], diabetes [29], endometriosis [30], primary dysmenorrhea [31], schizophrenia [32], and Sjögren׳s syndrome [33] etc.
In this study, we also used a population-based database to investigate the demographic characteristics, the overall survival analysis and prescription patterns of individuals with hypertension among type 2 diabetes patients according to CHM usage. In addition, we also evaluate the effect of selected herbal formulas and single herbs on smooth muscle cell contractility.
Results
Demographic characteristics and overall survival analysis of
according to CHM usage
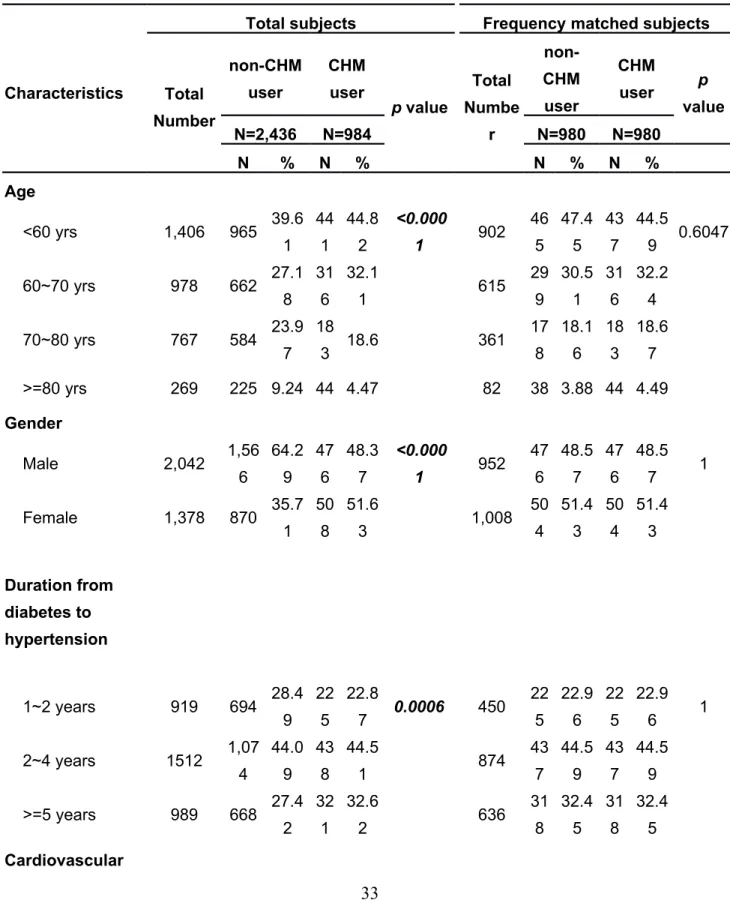
In this study, the database claims identified 984 CHM users and 2,434 non-CHM users with hypertension among type 2 diabetes patients from a cohort of one million randomly sampled cases from the National Health Insurance Research Database (NHIRD) [34] (Fig. 1 A). The demographic characteristics of CHM users versus non-CHM users (total subjects) are shown in the left side of Table 1. There were significant different frequency distributions for age, gender, duration from diabetes to hypertension, comorbidity (cardiovascular disease and hyperlipidaemia), and income for these two groups (p < 0.05). The CHM users (total subjects) were characterized with younger age, more females, longer duration time from diabetes to hypertension, lesser cases for cardiovascular disease, more cases for hyperlipidaemia, and higher incomes. The one-to-one match method was used to match CHM users and non-CHM users. After matching these two groups for age, gender and date of diagnosis of hypertension, CHM and non-CHM users were selected (Fig 1 B and Table 1 right side). There were significant different frequency distributions for duration from diabetes to hypertension, and hyperlipidaemia (p < 0.05). The CHM users were characterized with slightly longer duration time from diabetes to hypertension, and more cases for hyperlipidaemia.
The cumulative survival probability of individuals with hypertension among type 2 diabetes patients according to CHM usage were shown in Fig. 2. The overall survival rate
was different between CHM users and matched non-CHM users (p < 0.001). The cumulative survival probabilities were higher in CHM users than in matched non-CHM users suggesting that CHM may be beneficial for longer survival of hypertension individuals among type 2 diabetes patients.
Twelve most common herbal formulas and single herbs
prescribed by TCM doctors for the treatment of hypertension
individuals among type 2 diabetes patients
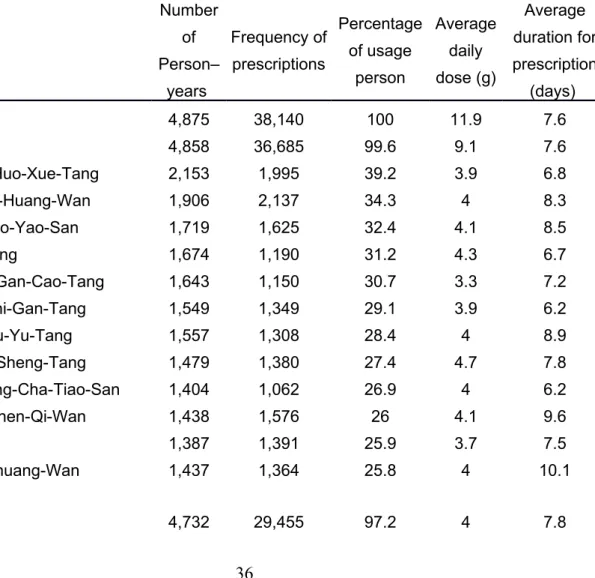
The 12 most common Chinese herbal formulas and single herbs prescribed for the CHM users analyzed in this study are listed in Table 2. The follow-up person-years were from hypertension to the study end as shown in Fig. 1B. The herbal composition of these herbal formulas and single herbs were also shown inTable A in S1 File. Shu-Jing-Huo-Xue-Tang was the most commonly prescribed herbal formula, followed by Liu-Wei-Di-Huang-Wan and Jia-Wei-Xiao-Yao-San. Among the top 12 herbal formulas, Ji-Sheng-Shen-Qi-Wan and Zi-Bai-Di-Huang-Ji-Sheng-Shen-Qi-Wan are 2 derivative formulas of Liu-Wei-Di-Huang-Ji-Sheng-Shen-Qi-Wan. Therefore, Liu-Wei-Di-Huang-Wan and its various derivatives were the most common
herbal formulas prescribed by Chinese medical doctors for the CHM users in this study. Of the 12 most common single herbs, Yan-Hu-Suo was the most commonly prescribed, followed by Dan-Shen and Ge-Gen.
Effect of most common herbal formulas and single herbs on
smooth muscle cell contractility
Smooth muscle cell contractility can be monitored by measuring the phosphorylation of myosin light chain protein [35]. The Y27632 compound (Rho kinase inhibitor) was used as the control for decreased myosin light chain phosphorylation [36]. And the calyculin compound was used as the control for increased myosin light chain phosphorylation [35]. We chose most common used two herbal formulas and two single herbs from these top 12 herbs (herbal formulas: Liu-Wei-Di-Huang-Wan and Jia-Wei-Xiao-Yao-San; single herbs: Dan-Shen and Ge-Gen) according to their frequencies of prescriptions and average duration for prescription. A10 cells (rat smooth muscle cells) were treated with these herbs at the concentrations as indicated (Fig. 3 A and B; S3A and S3B Fig. A and B). As shown, these four herbs reduced phosphorylation of myosin light chain. These herbs inhibited the phosphorylation of myosin light chain protein, suggesting that these most common herbs may be beneficial for smooth muscle cell contractility.
Discussion
In this study, we used a population-based database to investigate the demographic characteristics, the overall survival analysis and prescription patterns of individuals with hypertension among type 2 diabetes patients according to CHM usage. In addition, we also evaluate the effect of two herbal formulas and two single herbs from these top 12 herbs on smooth muscle cell contractility. We found that the cumulative survival probabilities were higher in CHM users than in non-CHM users. We also described the most common prescribed CHMs. The single herbs and the herbal formulas inhibited smooth muscle cell contractility. Our results suggest that adjunctive CHM therapy treatment may improve the overall survival rate of individuals with hypertension among type 2 diabetes patients and some of them modulate smooth muscle cell contractility.
Our results showed that the overall survival rate was higher in CHM users than in non-CHM users from hypertension individuals among type 2 diabetes patients. And we also found that patients treated with any CHM, herbal formulas or single herbs had the trend of lower risks of the death, macrovascular and microvascular diseases as the endpoints after adjusted for age, duration from diabetes to hypertension, and comorbidities by the conditional logistic analysis (Tables B-G in S1 FileTables S2-S7).
showed that there were more patients in non-CHM users who have used anti-diabetes drugs from diabetes to the index date (Table H in S1 File). However, there were no anti-diabetes drug usage differences between these two groups from index date to index date + 365 (Table I in S1 File). As for the anti-hypertension drugs from diabetes to the index day (Table H in S1 File), there were more patients in non-CHM users who have used anti-hypertension drugs- ACEI or ARB (p < 0.05). However, there were more patients in CHM users who have used anti-hypertension drugs- beta blocking agents (p < 0.05). From index date to index date + 365 (Table I in S1 File), there were more patients in non-CHM users who have used anti-hypertension drugs- ACEI or ARB (p < 0.05). CHM has been reported to reduce progression from impaired glucose tolerance to diabetes [37, 38]. Furthermore, CHMs have been used to successfully treat diabetes via increased insulin secretion and sensitivity, enhanced glucose uptake by adipose and muscle tissues, inhibition of glucose absorption by the intestine, inhibition of glucose production by hepatocytes, and anti-inflammatory activity [21-23, 39].
The most common herbal formulas were Liu-Wei-Di-Huang-Wan and Jia-Wei-Xiao-Yao-San. Liu-Wei-Di-Huang-Wan were the most common herbal formula in this study. Its various derivatives (Ji-Sheng-Shen-Qi-Wan, and Zi-Bai-Di-Huang-Wan) were also noted in our herbal formula list. Liu-Wei-Di-Huang-Wan are composed of Rx. Rehmanniae Preparata, Fr. Corni, Rx. Dioscoreae, Poria, Cx. Moutan, and Rz. Alismatis.
Liu-Wei-Di-Huang-Wan has been used to treat diabetes, pre-diabetes, fatigue, and metabolic syndrome [29, 40]. Furthermore, scientific evidence has suggested that Liu-Wei-Di-Huang-Wan can decrease visceral fat deposition [41], increase plasma levels of adiponectin and improve insulin resistance [42], and improve the lipid profile indicating a reduction of cardiovascular risk [43]. And Liu-Wei-Di-Huang-Wan combined with antihypertensive drugs appears to be effective in improving blood pressure and symptoms in patients with essential hypertension [44]. We have found that there were also no significant differences in the osmolarity and cell survival rate of cells among these herbal formulas and single herbs as compared with the cell only control, suggesting that the osmolarity of the Chinese herbal medicine are suitable for the cells in culture (S1A and S1B Fig. A and B). Furthermore, our functional analysis by measuring the phosphorylation of myosin light chain protein and the collage contraction assay (S2A-D Fig. A-D) first showed that smooth muscle cell contractility was inhibited by treatment with Liu-Wei-Di-Huang-Wan, which was in agreement with previous clinical observations [44]. Jia-Wei-Xiao-Yao-San are composed of Rx. Angelicae Sinensis, Rx. Paeoniae Alba, Poria, Rz. Atractylodis Macrocephalae, Rx. Bupleuri, Cx. Moutan, Fr. Gardeniae, and Rx. Gly. Jia-Wei-Xiao-Yao-San is used to treat symptoms including nervousness, palpitations, headache, anorexia, night sweating, dry eyes, hot flashes, and irregular menstruation; it also has hepatoprotective effects [45-49]. However, there were no related literatures related to the effect of Jia-Wei-Xiao-Yao-San on
diabetes or hypertension. To our knowledge, this is the first study to show that Jia-Wei-Xiao-Yao-San can inhibit smooth muscle cell contractility by measuring the phosphorylation of myosin light chain protein and the collage contraction assay (S2A-D Fig. A-D).
Dan-Shen was the most common single herb and composed of Radix Salviae Miltiorrhizae. In previous studies, Dan-Shen has been shown to have protective effects on the cardiovascular system [50-54] and pulmonary arteries [55, 56]. Furthermore, active component (SalB) from Dan-Shen can exhibit antidiabetic activity and inhibit symptoms of diabetes mellitus in rats and these effects may partially be correlated with its insulin sensitivity, glycogen synthesis and antioxidant activities [57-60]. Ge-Gen was composed of Radix Puerariae and contains an isoflavonoid glycoside with hypotensive effects, with excellent clinical results in the treatment of hypertension [61]. Furthermore, puerarin is a major active ingredient of Ge-Gen and exerts significant protective effects against diabetic retinopathy in rats via regulating angiogenesis factors expressions [62]. Interestingly, our results suggest that patients treated with the single herb- Ge-Gen had the statistical significance of lower risk of acute myocardial infarction and nephropathy (Table B and F in S1 File). There were no trends or statistical significance observed from the ischemic stroke, hemorrhagic stroke and amputation as the endpoint (Table C-E in S1 File). We are the first to suggest that Dan-Shen and Ge-Gen were the most common single herbs for individuals with hypertension among type 2 diabetes patients and in vitro functional analysis suggested
that smooth muscle cell contraction was inhibited by treatment with these herbs.
By integrating the National Health Insurance Research Database (NHIRD) review with our in vitro functional data, we were able to investigate the mechanism of action of CHM in the treatment of disease. Limitations of this study included a lack of blood physiological and biochemical measures in this database, such as blood pressure or blood sugar. The NHIRD limitations also include lacks of genetic factors, environmental factors (including levels of job stress and exercise), personal histories (including education and body mass index), and potential disease misclassifications [63-67]. The usage of CHM improves the overall survival rate of individuals with hypertension among type 2 diabetes patients and also these CHM treatment modulates smooth muscle cell contractility. Our study provides a CHM comprehensive list that may be useful in future investigation of the safety and efficacy for individuals with hypertension among type 2 diabetes patients.
Materials and methods
Ethical statement
This study was evaluated and approved for the purchase of the National Health Insurance Research Database (NHIRD) by the Human Studies Committee of China Medical University Hospital, Taichung, Taiwan. No informed consent was required because the data were analyzed anonymously. The cell line rat aortic smooth muscle cell line A10 cells
(BCRC number:60127; used in Fig. 3A and 3B) were purchased from Food Industry
Research and Development Institute in Taiwan
(https://catalog.bcrc.firdi.org.tw/BSAS_cart/controller?
event=SEARCH&bcrc_no=60127&type_id=4&keyword=smooth;;muscle;;cells). These cells were derived from the thoracic aorta of rats and served as a commonly used model of vascular smooth muscle cells [35] and were approved by the Animal Care and Use Committee (IACUC) of China Medical University, Taichung, Taiwan.
National Health Insurance Research Database (NHIRD) resource
in Taiwan
The national health insurance (NHI) program in Taiwan was started in 1995 to make health care available for all residents of Taiwan. As of 2010, over 99% of residents were enrolled in the program [68]. The NHI program provides the National Health Insurance Research Database (NHIRD) resource (http://nhird.nhri.org.tw/en/index.htm) for scientists in Taiwan and only for research purposes. Data for this study were retrieved from the “Longitudinal Health Insurance Database (LHID2000)”, which includes all the original claim data and registration files for 1,000,000 beneficiaries, randomly sampled from the year 2000 Registry for Beneficiaries (n = 23.72 million) under the NHI program. This database
contains information on patient demographics, diagnoses, prescriptions, records of clinical visits and hospitalizations, inpatient orders, ambulatory care, and socio-demographic factors. Disease diagnoses are coded using the International Classification of Disease, 9th
Revision, Clinical Modification (ICD-9-CM). This database also include traditional Chinese medicine services (Chinese herbal medicine (CHM), acupuncture, and manipulative therapies; http://www.nhi.gov.tw/English/webdata/webdata.aspx? menu=11&menu_id=592&WD_ID=592&webdata_id=3161). The data are from the National
Health Insurance Research Database, Taiwan (NHIRD)
http://nhird.nhri.org.tw/en/index.html. Contact nhird@nhri.org.tw for details and data access.
Study population
This study was designed as a population-based retrospective cohort study. In this study, a cohort of one million individuals randomized selected from NHI (Taiwan) was used. The sampled population was representative of all NHI beneficiaries. The study subjects were selected from this cohort and were shown in Fig. 1A. There were 84,032 individuals with diabetes (ICD-9-CM: 250) between 1998 and 2010. The hypertension ICD-9-CM used in this study was from 401-405. Individuals under the age of 20 were excluded. Individuals without hypertension (ICD-9-CM: 401-405), who had hypertension before diabetes, who had hypertension within 1 year after diabetes, and who had hypertension after 2009 were
also excluded. In addition, at least one of the following enrollment criteria had to med for identifying patients with hypertension in the study: (1) one or more inpatient admissions with diagnosis of hypertension, or (2) three or more outpatients visits within one-year period, each with a diagnosis of hypertension. The first date which satisfied the above (1) or (2) criteria was defined as the date of diagnosis of hypertension. After all of these criteria were applied, 10,664 study subjects were included in the study cohort.
Definition of CHM and non-CHM users
Study subjects with a record of cumulative CHM drug days more than 28 within first year after hypertension were defined as CHM users (N=984, Fig. 1B). Study subjects with no recorded of CHM usage were defined as non-CHM users (N=2,434). The date of satisfying the criterion of cumulative 28 drug days of CHM prescription was designated as the index date (Fig 1 B). The one-to-one match method was used to match CHM users and non-CHM users. After matching these two groups for age, gender and date of diagnosis of hypertension, CHM and non-CHM users were selected (Fig 1 B and Table 1 right side). A total of 980 subjects for each group were selected. The study endpoint was as the following: date of death, date of withdrawal from the NHI program, or date of follow-up termination (31 Dec. 2010). This study was designed as a population-based retrospective cohort study and to explore the effect of Chinese Herbal Medicine treatment on the overall
survival rate of individuals with hypertension among type 2 diabetes patients.
Chinese herbal medicine (CHM)
All drug codes for CHM (herbal formulas and single herbs) were collected and grouped according to their name. The frequencies of prescriptions, cumulative drug doses, average durations of per prescription, and follow-up person years were calculated from hypertension to the study end for the CHM users. Herbal formulas usually constituted a combination of 2 to 17 herbs (Table A in S1 File), created by experienced TCM doctors; these formulas have been used for thousands of years. Single herbs were obtained from plant, animal, or mineral material and can be mixed with other herbs to create a formula. The herbal formulas and single herbs in the NHIRD database were all produced by Good Manufacturing Practice (GMP) certified traditional Chinese medicine manufacturers based in Taiwan. These manufacturers included Sun Ten Pharmaceutical Co. Ltd., Shang Chang Pharmaceutical Co. Ltd., Chuang Song Zong Pharmaceutical Co. Ltd., KO DA Pharmaceutical Co. Ltd., and Kaiser Pharmaceutical Co. Ltd.
Study covariates
Urbanization levels in Taiwan are divided into five strata according to the Taiwan National Health Research Institute publications, with level 1 referring to the most urbanized communities and level 5 referring to the least urbanized communities. We identified the diagnoses of comorbidities which defined by following diagnoses recorded before the diagnosis date of hypertension: cardiovascular disease (ICD-9-CM: 430–437), ischaemic heart disease (ICD-9-CM: 410–414), chronic kidney disease (ICD-9-CM: 582–583) and hyperlipidaemia (ICD-9-CM: 272) (Table 1). The diagnosis criteria for each comorbidity were similar to those for hypertension.
We also applied the conditional multivariable logistic regression adjusted for all variables in the table 1 to assess the effect of CHM on the occurrence of blood pressure related disease such as acute myocardial infarction, ischemic stroke, hemorrhagic stroke, amputation, and nephropathy (the results were shown in the supplemental tables S2-S6Tables B-F in S1 File). The covariates included CHM user, age, income, duration from diabetes to hypertension, and comorbidities before hypertension including cardiovascular disease (ICD-9-CM: 430–437), ischaemic heart disease (ICD-9-CM: 410–414), chronic kidney disease (ICD-9-CM: 582–583) and hyperlipidaemia (ICD-9-CM: 272).
Cell culture,
reagents, and Western blotting
Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 100 U/mL penicillin, 100 U/mL streptomycin, and 2 mM L-glutamine (Gibco). Y27632, and calyculin A were purchased from Sigma (St. Louis, MO, USA). A10 cells were treated with Y27632 (10 µM), and calyculin A (50 µg/ml) for 10 min. The treated cells were lysed in RIPA buffer (Thermo Scientific TM) and then were applied to Western blot analysis and staining with
anti-phospho-myosin light chain (MLC) (1:1,000 dilution), anti-total-MLC (1:1,000 dilution), and anti-beta actin (1:1,000 dilution) antibodies (Fig. 3; S3 Fig.). The monoclonal anti-phospho-MLC
(phospho-myosin light chain 2 [Ser19] mouse mAb; catalog number: 3675) and polyclonal
anti-total-MLC (myosin light chain 2 antibody; catalog number: 3672) rabbit antibodies were from Cell Signaling Technology, Inc. The anti-beta actin (actin antibody [mAbGEa]; catalog number: NB100-74340) mouse monoclonal antibody was obtained from Novus Biologicals. The experimental protocol used for Western blotting has been described previously [69, 70]. Briefly, cells were harvested, washed, and lysed in lysis buffer (50 mM Tris-HCl [pH 7.5], 150 mM NaCl, 5 mM EDTA, 1% Triton X-100, 0.1% SDS) supplemented with protease inhibitor cocktail (Roche). The lysates were resolved by 12% SDS-PAGE and transferred to polyvinylidene fluoride membranes (Millipore). The membranes were incubated with primary antibodies overnight at 4°C and then incubated with alkaline phosphatase-conjugated secondary antibodies (Goat anti-Mouse IgG (H+L) Polyclonal Secondary Antibody, HRP conjugate; 1:5000 dilutions; catalog number: A16072; Thermo Fisher
Scientific). Signals were visualized using a SuperSignal West Femto Maximum Sensitivity Substrate Detection Kit; catalog number: 34096; Thermo Fisher Scientific) in accordance with the manufacturer's instructions.
Statistical analysis
We presented demographic data such as age, gender, duration from diabetes to hypertension, comorbidities (cardiovascular disease, ischaemic heart disease, chronic kidney disease, and hyperlipidaemia), income, and urbanization level for both groups (CHM and non-CHM users) using count and percentage for categorical variables, and used chi-squared tests to assess their differences (Table 1). We sorted the cumulative person-years for each herbal formula and single herb and listed the top 12 most common herbal formulas and single herbs (Table 2). We employed Kaplan-Meier method to estimate the cumulative survival probabilities and used the log-rank test to explore the effect of Chinese Herbal Medicine treatment on the overall survival rate of individuals with hypertension among type 2 diabetes patients (CHM and non-CHM users; Fig. 2). We also used conditional logistic analysis to explore the effect of CHM therapy as well as these most commonly used herbs on the reduction of macrovascular and microvascular diseases, and death as the endpoints during follow up (Tables B-G in S1 FileTables S2-S7). All p-values less than 0.05 were considered significant. All data management and statistical analyses were performed using
Statistical Analysis System (SAS) software (version 9.3; SAS Institute, Cary, NC, USA).
References
1. Geneva WHO. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. WHO/NCD/NCS/992. 1999. 2. Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362(12):1090-101. Epub 2010/03/26. doi: 10.1056/NEJMoa0908292 362/12/1090 [pii]. PubMed PMID: 20335585.
3. Saquib N, Saquib J, Ahmed T, Khanam MA, Cullen MR. Cardiovascular diseases and type 2 diabetes in Bangladesh: a systematic review and meta-analysis of studies between 1995 and 2010. BMC Public Health. 2012;12:434. Epub 2012/06/15. doi: 10.1186/1471-2458-12-434
1471-2458-12-434 [pii]. PubMed PMID: 22694854; PubMed Central PMCID: PMC3487781.
4. Shera AS, Rafique G, Khawaja IA, Baqai S, King H. Pakistan National Diabetes Survey: prevalence of glucose intolerance and associated factors in Baluchistan province. Diabetes Res Clin Pract. 1999;44(1):49-58. Epub 1999/07/22. doi: S0168-8227(99)00017-0 [pii]. PubMed PMID: 10414940.
5. Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365(9467):1333-46. Epub 2005/04/13. doi: S0140-6736(05)61032-X [pii] 10.1016/S0140-6736(05)61032-X. PubMed PMID: 15823385.
6. Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444(7121):840-6. Epub 2006/12/15. doi: nature05482 [pii]
10.1038/nature05482. PubMed PMID: 17167471.
7. Wang B, Ni Y, Zhong J, Sun F. Effects of incretins on blood pressure: a promising therapy for type 2 diabetes mellitus with hypertension. J Diabetes. 2012;4(1):22-9. Epub 2011/11/02. doi: 10.1111/j.1753-0407.2011.00167.x. PubMed PMID: 22040104.
8. Lin K, Lloyd-Jones DM, Li D, Carr JC. Quantitative imaging biomarkers for the evaluation of cardiovascular complications in type 2 diabetes mellitus. J Diabetes Complications. 2014;28(2):234-42. Epub 2013/12/07. doi: S1056-8727(13)00211-0 [pii]
10.1016/j.jdiacomp.2013.09.008. PubMed PMID: 24309215.
9. Lebovitz HE. Etiology and pathogenesis of diabetes mellitus. Pediatr Clin North Am. 1984;31(3):521-30. Epub 1984/06/01. PubMed PMID: 6374587.
10. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837-53. Epub 1998/09/22. doi:
S0140673698070196 [pii]. PubMed PMID: 9742976.
11. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317(7160):703-13. Epub 1998/09/11. PubMed PMID: 9732337; PubMed Central PMCID: PMC28659.
12. Mehler PS, Coll JR, Estacio R, Esler A, Schrier RW, Hiatt WR. Intensive blood pressure control reduces the risk of cardiovascular events in patients with peripheral arterial disease and type 2 diabetes. Circulation. 2003;107(5):753-6. Epub 2003/02/13. PubMed PMID: 12578880.
13. Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes Care. 2000;23 Suppl 2:B54-64. Epub 2000/06/22. PubMed PMID: 10860192.
14. Li S, Culver B, Ren J. Benefit and risk of exercise on myocardial function in diabetes. Pharmacol Res. 2003;48(2):127-32. Epub 2003/06/12. doi: S1043661803000999 [pii]. PubMed PMID: 12798664.
15. Rao AD, Kuhadiya N, Reynolds K, Fonseca VA. Is the combination of sulfonylureas and metformin associated with an increased risk of cardiovascular disease or all-cause mortality?: a meta-analysis of observational studies. Diabetes Care. 2008;31(8):1672-8. Epub 2008/05/07. doi: 10.2337/dc08-0167
dc08-0167 [pii]. PubMed PMID: 18458139; PubMed Central PMCID: PMC2494623.
16. Roumie CL, Hung AM, Greevy RA, Grijalva CG, Liu X, Murff HJ, et al. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann Intern Med. 2012;157(9):601-10. Epub 2012/11/07. doi: 10.7326/0003-4819-157-9-201211060-00003
1389845 [pii]. PubMed PMID: 23128859.
17. Loke YK, Singh S, Furberg CD. Long-term use of thiazolidinediones and fractures in type 2 diabetes: a meta-analysis. CMAJ. 2009;180(1):32-9. Epub 2008/12/17. doi: 10.1503/cmaj.080486 cmaj.080486 [pii]. PubMed PMID: 19073651; PubMed Central PMCID: PMC2612065.
18. Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007;298(10):1180-8. Epub 2007/09/13. doi: 298/10/1180 [pii]
10.1001/jama.298.10.1180. PubMed PMID: 17848652.
19. Singh S, Loke YK, Furberg CD. Long-term use of thiazolidinediones and the associated risk of pneumonia or lower respiratory tract infection: systematic review and meta-analysis. Thorax. 2011;66(5):383-8. Epub 2011/02/18. doi: 10.1136/thx.2010.152777
thx.2010.152777 [pii]. PubMed PMID: 21325145.
20. Turner RM, Kwok CS, Chen-Turner C, Maduakor CA, Singh S, Loke YK. Thiazolidinediones and associated risk of Bladder Cancer: a Systematic Review and Meta-analysis. Br J Clin Pharmacol. 2013. Epub 2013/12/12. doi: 10.1111/bcp.12306. PubMed PMID: 24325197.
management of diabetes. Adv Exp Med Biol. 2012;771:396-413. Epub 2013/02/09. PubMed PMID: 23393692.
22. Ceylan-Isik AF, Fliethman RM, Wold LE, Ren J. Herbal and traditional Chinese medicine for the treatment of cardiovascular complications in diabetes mellitus. Curr Diabetes Rev. 2008;4(4):320-8. Epub 2008/11/11. PubMed PMID: 18991600.
23. Li WL, Zheng HC, Bukuru J, De Kimpe N. Natural medicines used in the traditional Chinese medical system for therapy of diabetes mellitus. J Ethnopharmacol. 2004;92(1):1-21. Epub 2004/04/22. doi: 10.1016/j.jep.2003.12.031
S0378874104000315 [pii]. PubMed PMID: 15099842.
24. Lee YC, Huang YT, Tsai YW, Huang SM, Kuo KN, McKee M, et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010;10:225. Epub 2010/08/05. doi: 10.1186/1472-6963-10-225
1472-6963-10-225 [pii]. PubMed PMID: 20682077; PubMed Central PMCID: PMC2924329.
25. Chen FP, Chen TJ, Kung YY, Chen YC, Chou LF, Chen FJ, et al. Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv Res. 2007;7:26. Epub 2007/02/27. doi: 1472-6963-7-26 [pii]
10.1186/1472-6963-7-26. PubMed PMID: 17319950; PubMed Central PMCID: PMC1810531. 26. Huang TP, Liu PH, Lien AS, Yang SL, Chang HH, Yen HR. Characteristics of traditional Chinese medicine use in children with asthma: a nationwide population-based study. Allergy. 2013;68(12):1610-3. Epub 2013/10/15. doi: 10.1111/all.12273. PubMed PMID: 24117783.
27. Lai JN, Wu CT, Wang JD. Prescription pattern of chinese herbal products for breast cancer in taiwan: a population-based study. Evid Based Complement Alternat Med. 2012;2012:891893. Epub 2012/06/12. doi: 10.1155/2012/891893. PubMed PMID: 22685488; PubMed Central PMCID: PMC3368194.
28. Hsieh CF, Huang SL, Chen CL, Chen WT, Chang HC, Yang CC. Non-aristolochic acid prescribed Chinese herbal medicines and the risk of mortality in patients with chronic kidney disease: results from a population-based follow-up study. BMJ Open. 2014;4(2):e004033. Epub 2014/02/25. doi: 10.1136/bmjopen-2013-004033
bmjopen-2013-004033 [pii]. PubMed PMID: 24561496; PubMed Central PMCID: PMC3931999. 29. Huang CY, Tsai YT, Lai JN, Hsu FL. Prescription pattern of chinese herbal products for diabetes mellitus in taiwan: a population-based study. Evid Based Complement Alternat Med. 2013;2013:201329. Epub 2013/07/12. doi: 10.1155/2013/201329. PubMed PMID: 23843864; PubMed Central PMCID: PMC3703417.
30. Fang RC, Tsai YT, Lai JN, Yeh CH, Wu CT. The traditional chinese medicine prescription pattern of endometriosis patients in taiwan: a population-based study. Evid Based Complement Alternat Med. 2012;2012:591391. Epub 2012/10/12. doi: 10.1155/2012/591391. PubMed PMID: 23056141; PubMed Central PMCID: PMC3463977.
pattern of patients with primary dysmenorrhea in Taiwan: a large-scale cross sectional survey. J Ethnopharmacol. 2014;152(2):314-9. Epub 2014/01/15. doi: 10.1016/j.jep.2014.01.002
S0378-8741(14)00011-7 [pii]. PubMed PMID: 24417866.
32. Lin HC, Yang WC, Lee HC. Traditional Chinese medicine usage among schizophrenia patients. Complement Ther Med. 2008;16(6):336-42. Epub 2008/11/26. doi: 10.1016/j.ctim.2007.11.001 S0965-2299(07)00113-6 [pii]. PubMed PMID: 19028334.
33. Yu MC, Lin SK, Lai JN, Wei JC, Cheng CY. The traditional Chinese medicine prescription patterns of Sjogrens patients in Taiwan: A population-based study. J Ethnopharmacol. 2014. Epub 2014/06/07. doi: S0378-8741(14)00418-8 [pii]
10.1016/j.jep.2014.05.049. PubMed PMID: 24905866.
34. Lin CH, Sheu WH. Hypoglycaemic episodes and risk of dementia in diabetes mellitus: 7-year follow-up study. J Intern Med. 2013;273(1):102-10. Epub 2012/09/26. doi: 10.1111/joim.12000. PubMed PMID: 23003116.
35. Bhadriraju K, Elliott JT, Nguyen M, Plant AL. Quantifying myosin light chain phosphorylation in single adherent cells with automated fluorescence microscopy. BMC Cell Biol. 2007;8:43. Epub 2007/10/19. doi: 1471-2121-8-43 [pii]
10.1186/1471-2121-8-43. PubMed PMID: 17941977; PubMed Central PMCID: PMC2213650. 36. Uehata M, Ishizaki T, Satoh H, Ono T, Kawahara T, Morishita T, et al. Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature. 1997;389(6654):990-4. Epub 1997/11/14. doi: 10.1038/40187. PubMed PMID: 9353125.
37. Lian F, Li G, Chen X, Wang X, Piao C, Wang J, et al. Chinese herbal medicine Tianqi reduces progression from impaired glucose tolerance to diabetes: a double-blind, randomized, placebo-controlled, multicenter trial. J Clin Endocrinol Metab. 2014;99(2):648-55. Epub 2014/01/18. doi: 10.1210/jc.2013-3276. PubMed PMID: 24432995.
38. Grant SJ, Bensoussan A, Chang D, Kiat H, Klupp NL, Liu JP, et al. Chinese herbal medicines for people with impaired glucose tolerance or impaired fasting blood glucose. Cochrane Database Syst Rev. 2009;(4):CD006690. Epub 2009/10/13. doi: 10.1002/14651858.CD006690.pub2. PubMed PMID: 19821382; PubMed Central PMCID: PMC3191296.
39. Hui H, Tang G, Go VL. Hypoglycemic herbs and their action mechanisms. Chin Med. 2009;4:11. Epub 2009/06/16. doi: 10.1186/1749-8546-4-11
1749-8546-4-11 [pii]. PubMed PMID: 19523223; PubMed Central PMCID: PMC2704217.
40. Qian Y, Xue YM, Li J, Zhu B, Pan YH, Zhang Y. [Effect of Liuweidihuang pills in preventing diabetes mellitus in OLETF rats]. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30(1):21-4. Epub 2010/02/02. PubMed PMID: 20117976.
41. Xue YM, Luo R, Zhu B, Zhang Y, Pan YH, Li CZ. [Liuweidihuang pills reduces visceral fat deposition in Otsuka Long-Evans Tokushima Fatty rats]. Nan Fang Yi Ke Da Xue Xue Bao. 2006;26(10):1446-8. Epub 2006/10/26. PubMed PMID: 17062348.
rats]. Nan Fang Yi Ke Da Xue Xue Bao. 2008;28(1):34-6. Epub 2008/01/30. PubMed PMID: 18227021.
43. van Wietmarschen HA, van der Greef J, Schroen Y, Wang M. Evaluation of symptom, clinical chemistry and metabolomics profiles during Rehmannia six formula (R6) treatment: an integrated and personalized data analysis approach. J Ethnopharmacol. 2013;150(3):851-9. Epub 2013/10/15. doi: 10.1016/j.jep.2013.09.041
S0378-8741(13)00688-0 [pii]. PubMed PMID: 24120517.
44. Wang J, Yao K, Yang X, Liu W, Feng B, Ma J, et al. Chinese patent medicine liu wei di huang wan combined with antihypertensive drugs, a new integrative medicine therapy, for the treatment of essential hypertension: a systematic review of randomized controlled trials. Evid Based Complement Alternat Med. 2012;2012:714805. Epub 2012/12/22. doi: 10.1155/2012/714805. PubMed PMID: 23258998; PubMed Central PMCID: PMC3520441.
45. Qu Y, Gan HQ, Mei QB, Liu L. Study on the effect of Jia-Wei-Xiao-Yao-San decoction on patients with functional dyspepsia. Phytother Res. 2010;24(2):245-8. Epub 2009/07/18. doi: 10.1002/ptr.2920. PubMed PMID: 19610028.
46. Chao TH, Fu PK, Chang CH, Chang SN, Chiahung Mao F, Lin CH. Prescription patterns of Chinese herbal products for post-surgery colon cancer patients in Taiwan. J Ethnopharmacol. 2014;155(1):702-8. Epub 2014/06/20. doi: 10.1016/j.jep.2014.06.012
S0378-8741(14)00460-7 [pii]. PubMed PMID: 24945402.
47. Wang BR, Chang YL, Chen TJ, Chiu JH, Wu JC, Wu MS, et al. Coprescription of Chinese herbal medicine and Western medication among female patients with breast cancer in Taiwan: analysis of national insurance claims. Patient Prefer Adherence. 2014;8:671-82. Epub 2014/05/24. doi: 10.2147/PPA.S61280
ppa-8-671 [pii]. PubMed PMID: 24855343; PubMed Central PMCID: PMC4019611.
48. Chen LC, Tsao YT, Yen KY, Chen YF, Chou MH, Lin MF. A pilot study comparing the clinical effects of Jia-Wey Shiau-Yau San, a traditional Chinese herbal prescription, and a continuous combined hormone replacement therapy in postmenopausal women with climacteric symptoms. Maturitas. 2003;44(1):55-62. Epub 2003/02/06. doi: S0378512202003146 [pii]. PubMed PMID: 12568736.
49. Chien SC, Chang WC, Lin PH, Chang WP, Hsu SC, Chang JC, et al. A chinese herbal medicine, jia-wei-xiao-yao-san, prevents dimethylnitrosamine-induced hepatic fibrosis in rats. ScientificWorldJournal. 2014;2014:217525. Epub 2014/07/06. doi: 10.1155/2014/217525. PubMed PMID: 24995353; PubMed Central PMCID: PMC4065731.
50. Zhang T, Xu J, Li D, Chen J, Shen X, Xu F, et al. Salvianolic acid A, a matrix metalloproteinase-9 inhibitor of Salvia miltiorrhiza, attenuates aortic aneurysm formation in apolipoprotein E-deficient mice. Phytomedicine. 2014;21(10):1137-45. Epub 2014/06/12. doi: 10.1016/j.phymed.2014.05.003
51. Jiang B, Li D, Deng Y, Teng F, Chen J, Xue S, et al. Salvianolic acid A, a novel matrix metalloproteinase-9 inhibitor, prevents cardiac remodeling in spontaneously hypertensive rats. PLoS One. 2013;8(3):e59621. Epub 2013/03/28. doi: 10.1371/journal.pone.0059621
PONE-D-12-35832 [pii]. PubMed PMID: 23533637; PubMed Central PMCID: PMC3606118. 52. Woo KS, Yip TW, Chook P, Kwong SK, Szeto CC, Li JK, et al. Cardiovascular Protective Effects of Adjunctive Alternative Medicine (Salvia miltiorrhiza and Pueraria lobata) in High-Risk Hypertension. Evid Based Complement Alternat Med. 2013;2013:132912. Epub 2013/03/28. doi: 10.1155/2013/132912. PubMed PMID: 23533460; PubMed Central PMCID: PMC3606734.
53. Hu F, Koon CM, Chan JY, Lau KM, Kwan YW, Fung KP. Involvements of calcium channel and potassium channel in Danshen and Gegen decoction induced vasodilation in porcine coronary LAD artery. Phytomedicine. 2012;19(12):1051-8. Epub 2012/08/15. doi: 10.1016/j.phymed.2012.07.007
S0944-7113(12)00217-6 [pii]. PubMed PMID: 22889578.
54. Yang TY, Wei JC, Lee MY, Chen CM, Ueng KC. A randomized, double-blind, placebo-controlled study to evaluate the efficacy and tolerability of Fufang Danshen (Salvia miltiorrhiza) as add-on antihypertensive therapy in Taiwanese patients with uncontrolled hypertension. Phytother Res. 2012;26(2):291-8. Epub 2011/09/03. doi: 10.1002/ptr.3548. PubMed PMID: 21887804.
55. Wang J, Lu W, Wang W, Zhang N, Wu H, Liu C, et al. Promising therapeutic effects of sodium tanshinone IIA sulfonate towards pulmonary arterial hypertension in patients. J Thorac Dis. 2013;5(2):169-72. Epub 2013/04/16. doi: 10.3978/j.issn.2072-1439.2013.02.04
jtd-05-02-169 [pii]. PubMed PMID: 23585945; PubMed Central PMCID: PMC3621926.
56. Wang J, Jiang Q, Wan L, Yang K, Zhang Y, Chen Y, et al. Sodium tanshinone IIA sulfonate inhibits canonical transient receptor potential expression in pulmonary arterial smooth muscle from pulmonary hypertensive rats. Am J Respir Cell Mol Biol. 2013;48(1):125-34. Epub 2012/10/16. doi: 10.1165/rcmb.2012-0071OC
rcmb.2012-0071OC [pii]. PubMed PMID: 23065131; PubMed Central PMCID: PMC3547081. 57. Huang M, Wang P, Xu S, Xu W, Chu K, Lu J. Biological activities of salvianolic acid B from Salvia miltiorrhiza on type 2 diabetes induced by high-fat diet and streptozotocin. Pharm Biol. 2015;53(7):1058-65. Epub 2015/01/24. doi: 10.3109/13880209.2014.959611. PubMed PMID: 25612777.
58. Raoufi S, Baluchnejadmojarad T, Roghani M, Ghazanfari T, Khojasteh F, Mansouri M. Antidiabetic potential of salvianolic acid B in multiple low-dose streptozotocin-induced diabetes. Pharm Biol. 2015;53(12):1803-9. Epub 2015/04/18. doi: 10.3109/13880209.2015.1008148. PubMed PMID: 25885938.
59. Lian F, Wu L, Tian J, Jin M, Zhou S, Zhao M, et al. The effectiveness and safety of a danshen-containing Chinese herbal medicine for diabetic retinopathy: a randomized, double-blind, placebo-controlled multicenter clinical trial. J Ethnopharmacol. 2015;164:71-7. Epub 2015/02/11. doi: 10.1016/j.jep.2015.01.048
S0378-8741(15)00063-X [pii]. PubMed PMID: 25666427.
60. Cai H, Lian L, Wang Y, Yu Y, Liu W. Protective effects of injection against learning and memory impairments in streptozotocin-induced diabetic rats. Exp Ther Med. 2014;8(4):1127-30. Epub 2014/09/05. doi: 10.3892/etm.2014.1919
etm-08-04-1127 [pii]. PubMed PMID: 25187809; PubMed Central PMCID: PMC4151631.
61. Qicheng F. Some current study and research approaches relating to the use of plants in the traditional Chinese medicine. J Ethnopharmacol. 1980;2(1):57-63. Epub 1980/03/01. PubMed PMID: 7464185.
62. Teng Y, Cui H, Yang M, Song H, Zhang Q, Su Y, et al. Protective effect of puerarin on diabetic retinopathy in rats. Mol Biol Rep. 2009;36(5):1129-33. Epub 2008/07/01. doi: 10.1007/s11033-008-9288-2. PubMed PMID: 18587665.
63. Koo M, Chen CH, Tsai KW, Lu MC, Lin SC. Ambulatory medical services utilization for menstrual disorders among female personnel of different medical professions in Taiwan: a nationwide retrospective cohort study. BMC Womens Health. 2015;15(1):66. doi: 10.1186/s12905-015-0220-3. PubMed PMID: 26306618; PubMed Central PMCID: PMCPMC4550071.
64. Chen MJ, Tsan YT, Liou JM, Lee YC, Wu MS, Chiu HM, et al. Statins and the risk of pancreatic cancer in Type 2 diabetic patients-A population-based cohort study. Int J Cancer. 2015. doi: 10.1002/ijc.29813. PubMed PMID: 26296262.
65. Wang SH, Chen DY, Lin YS, Mao CT, Tsai ML, Hsieh MJ, et al. Cardiovascular Outcomes of Sitagliptin in Type 2 Diabetic Patients with Acute Myocardial Infarction, a Population-Based Cohort Study in Taiwan. PLoS One. 2015;10(6):e0131122. doi: 10.1371/journal.pone.0131122. PubMed PMID: 26115092; PubMed Central PMCID: PMCPMC4482692.
66. Chang CH, Chen SJ, Liu CY. Risk of Developing Depressive Disorders following Hepatocellular Carcinoma: A Nationwide Population-Based Study. PLoS One. 2015;10(8):e0135417. doi: 10.1371/journal.pone.0135417. PubMed PMID: 26295711; PubMed Central PMCID: PMCPMC4546687.
67. Chen YC, Kok VC, Chien CH, Horng JT, Tsai JJ. Cancer risk in patients aged 30 years and above with type 2 diabetes receiving antidiabetic monotherapy: a cohort study using metformin as the comparator. Ther Clin Risk Manag. 2015;11:1315-23. doi: 10.2147/TCRM.S91513. PubMed PMID: 26357479; PubMed Central PMCID: PMCPMC4559233.
68. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047-53. Epub 2004/04/28. PubMed PMID: 15111519.
69. Liu X, Feng R. Inhibition of epithelial to mesenchymal transition in metastatic breast carcinoma cells by c-Src suppression. Acta Biochim Biophys Sin (Shanghai). 2010;42(7):496-501. Epub 2010/08/14. doi: 10.1093/abbs/gmq043
gmq043 [pii]. PubMed PMID: 20705589.
PP2-induced apoptosis in human breast cancer MCF-7 cells. FEBS Lett. 2010;584(14):3185-92. Epub 2010/06/15. doi: 10.1016/j.febslet.2010.06.002
S0014-5793(10)00483-7 [pii]. PubMed PMID: 20541551.
Acknowledgments
The authors wish to thank the Division of Chinese Medicine, China Medical University Beigang Hospital for administrative assistance and consultation and the Aim for Top University Plan of the Ministry of Education, Taiwan at the China Medical University. We also thank Drs. Ya-Hui Chi, Kuan-Teh Jeang, Yuan-Chia Chang, and Willy W.L. Hong for technical help and suggestions.
Author contributions
YJL, TJH, FJT, and WML conceived and designed the experiments. THL, CCL, and SMH performed the experiments. CBW, WKC, JHC, YCY, YTS, YCL, and CFC analyzed the data. XL, HT, JPL, CWL, HYP, JGL, YHL, SYC, and WML contributed reagents/materials/analysis tools. YJL and WML wrote the manuscript. All the authors have read and approved the final manuscript.
Competing financial interests:
The authors declare no competing financial interests.Figure Legends
Fig. 1 Flow recruitment diagram.
A: Chart showing the protocol for enrollmentof study subjects. B: Follow-up time for CHM and matched non-CHM users.
Fig. 2 Cumulative survival curves of individuals with
hypertension among type 2 diabetes patients according to
Chinese herbal medicine (CHM) usage.
Fig. 3 Effect of the four most common herbal formulas and
(MLC) protein.
Briefly, A10 cells were treated with herbal formulas (A) or single herbs (B). Y27632 (Y10; 10 µM) and calyculin A (A50; 50 µg/ml) were used as negative and positive controls. Western blot analysis and staining with anti-phospho-MLC, anti-total-MLC, and anti-beta actin antibodies was then performed. Phospho-MLC, total-MLC, and beta actin were all obtained with their appropriate protein size bands. The relative Phospho-MLC intensity (%) was expressed as [(Phospho-MLC/total-MLC)drug treated/(Phospho-MLC/total-MLC)cell only x 100%]. The Mean±SEM values for at least three independent experiments
Table 1. Demographic characteristics of total subjects and frequency matched subjects with hypertension among type 2 diabetes patients according to CHM usage
Characteristics
Total subjects Frequency matched subjects
Total Number non-CHM user CHM user p value Total Numbe r non-CHM user CHM user p value N=2,436 N=984 N=980 N=980 N % N % N % N % Age <60 yrs 1,406 965 39.6 1 44 1 44.8 2 <0.000 1 902 46 5 47.4 5 43 7 44.5 9 0.6047 60~70 yrs 978 662 27.1 8 31 6 32.1 1 615 29 9 30.5 1 31 6 32.2 4 70~80 yrs 767 584 23.9 7 18 3 18.6 361 17 8 18.1 6 18 3 18.6 7 >=80 yrs 269 225 9.24 44 4.47 82 38 3.88 44 4.49 Gender Male 2,042 1,56 6 64.2 9 47 6 48.3 7 <0.000 1 952 47 6 48.5 7 47 6 48.5 7 1 Female 1,378 870 35.7 1 50 8 51.6 3 1,008 50 4 51.4 3 50 4 51.4 3 Duration from diabetes to hypertension 1~2 years 919 694 28.4 9 22 5 22.8 7 0.0006 450 22 5 22.9 6 22 5 22.9 6 1 2~4 years 1512 1,07 4 44.0 9 43 8 44.5 1 874 43 7 44.5 9 43 7 44.5 9 >=5 years 989 668 27.4 2 32 1 32.6 2 636 31 8 32.4 5 31 8 32.4 5 Cardiovascular
disease No 2,852 1,99 9 82.0 6 85 3 86.6 9 0.001 1,680 83 1 84.8 84 9 86.6 3 0.2453 Yes 568 437 17.9 4 13 1 13.3 1 280 14 9 15.2 13 1 13.3 7 Ischaemic heart disease No 2,664 1,88 9 77.5 5 77 5 78.7 6 0.4382 1,540 76 9 78.4 7 77 1 78.6 7 0.9123 Yes 756 547 22.4 5 20 9 21.2 4 420 21 1 21.5 3 20 9 21.3 3 Chronic kidney disease No 3,225 2,28 8 93.9 2 93 7 95.2 2 0.1692 1,858 92 4 94.2 9 93 4 95.3 1 0.3092 Yes 195 148 6.08 47 4.78 102 56 5.71 46 4.69 Hyperlipidaemia No 1,964 1,46 8 60.2 6 49 6 50.4 1 <0.0001 1,042 54 8 55.9 2 49 4 50.4 1 0.0145 Yes 1,456 968 39.7 4 48 8 49.5 9 918 43 2 44.0 8 48 6 49.5 9 Obesity No 3,374 2,40 9 98.8 9 96 5 98.0 7 0.0587 1,927 96 6 98.5 7 96 1 98.0 6 0.38 Yes 46 27 1.11 19 1.93 33 14 1.43 19 1.94 Alcohol-related illness No 3,369 2,39 7 98.4 97 2 98.7 8 0.4047 1,931 96 3 98.2 7 96 8 98.7 8 0.3496 Yes 51 39 1.6 12 1.22 29 17 1.73 12 1.22 Tobacco use No 3,401 2,42 6 99.5 9 97 5 99.0 9 0.0726 1,948 97 7 99.6 9 97 1 99.0 8 0.0823 Yes 19 10 0.41 9 0.91 12 3 0.31 9 0.92 INCOME
<NT20000 739 582 23.8 9 15 7 15.9 6 <0.000 1 359 20 2 20.6 1 15 7 16.0 2 0.0072 NT20000~NT3000 0 677 491 20.1 6 18 6 18.9 381 19 6 20 18 5 18.8 8 NT30000~NT4000 0 1,438 982 40.3 1 45 6 46.3 4 894 44 1 45 45 3 46.2 2 >=NT40000 566 381 15.6 4 18 5 18.8 326 14 1 14.3 9 18 5 18.8 8 Urbanization level 1 817 574 23.5 6 24 3 24.7 0.3331 488 24 5 25 24 3 24.8 0.4303 2 1,033 739 30.3 4 29 4 29.8 8 605 31 3 31.9 4 29 2 29.8 3 497 340 13.9 6 15 7 15.9 6 290 13 3 13.5 7 15 7 16.0 2 4 585 421 17.2 8 16 4 16.6 7 314 15 1 15.4 1 16 3 16.6 3 5 488 362 14.8 6 12 6 12.8 263 13 8 14.0 8 12 5 12.7 6
CHM, Chinese herbal medicine; N, number; NT, new Taiwan dollars.
Urbanization level: 1 indicates the hightest level of urbanization and 5 is the lowest level.
p values were obtained by chi-square test.
Table 2. Twelve most common herbal formulas and single herbs prescribed by TCM doctors for the treatment of hypertension individuals among type 2 diabetes patients
Number of Person– years Frequency of prescriptions Percentage of usage person Average daily dose (g) Average duration for prescription (days) Total 4,875 38,140 100 11.9 7.6 Herbal formula 4,858 36,685 99.6 9.1 7.6 Shu-Jing-Huo-Xue-Tang 2,153 1,995 39.2 3.9 6.8 Liu-Wei-Di-Huang-Wan 1,906 2,137 34.3 4 8.3 Jia-Wei-Xiao-Yao-San 1,719 1,625 32.4 4.1 8.5 Ge-Gen-Tang 1,674 1,190 31.2 4.3 6.7 Shao-Yao-Gan-Cao-Tang 1,643 1,150 30.7 3.3 7.2 Ma-Xing-Shi-Gan-Tang 1,549 1,349 29.1 3.9 6.2 Xue-Fu-Zhu-Yu-Tang 1,557 1,308 28.4 4 8.9 Du-Huo-Ji-Sheng-Tang 1,479 1,380 27.4 4.7 7.8 Chuan-Xiong-Cha-Tiao-San 1,404 1,062 26.9 4 6.2 Ji-Sheng-Shen-Qi-Wan 1,438 1,576 26 4.1 9.6 Gan-Lu-Yin 1,387 1,391 25.9 3.7 7.5 Zhi-Bai-Di-huang-Wan 1,437 1,364 25.8 4 10.1 Single herb 4,732 29,455 97.2 4 7.8
Yan-Hu-Suo 1,830 1,665 35.2 1.1 7.6 Ge-Gen 1,716 1,596 34.4 1.4 8.2 Dan-Shen 1,798 2,179 34.3 1.3 10.3 Tian-Hua-Fen 1,751 1,697 33.2 1.1 9.2 Jie-Geng 1,715 1,413 33 1 6.6 Bei-Mu 1,618 1,436 31.5 1.1 6.9 Huang-Qin 1,607 1,409 31.5 1.1 8 Niu-Xi 1,635 1,345 30.6 0.9 7.9 Mai-Men-Dong 1,516 1,287 28.6 1.2 8.9 Huang-Qi 1,473 1,807 28.3 1.4 8.8 Xuan-Shen 1,496 1,157 28.2 1.2 9 Xing-Ren 1,472 1,057 27.9 1.1 6.7
TCM, traditional Chinese medicine.
Captions for supporting Information files:
S1 Fig. Osmolarity and cell survival rate of cells treated with Chinese herbal medicine. (A)
Detection of the osmolarity from the cell culture medium as shown above by using Vapro TM Osmometer, Model 5520. The standard 290 and the concentrations of NaCl (0%, 0.5%, 1%, and 2%)
were used as the controls. Cells were in the presence of cells only, Y10 (Y27632 at 10 µM), single herbs- Dan-Shen and Ge-Gen, and herbal formula- Liu-Wei-Di-Huang-Wan and Jia-Wei-Xiao-Yao-San (5 and 10 µg/ml). Similar results were obtained in three independent experiments. Values represent the mean± S.D. (B) % of cell survival rate of cells treated with Chinese herbal medicine. Cells were in the presence of cells only, Y10 (Y27632 at 10 µM), single herbs- Dan-Shen and Ge-Gen, and herbal formula- Liu-Wei-Di-Huang-Wan and Jia-Wei-Xiao-Yao-San (5 and 10 µg/ml) for 24 h and were detected by using the WST-1 assay. Similar results were obtained in three independent experiments. Values represent the mean± S.D.
S2 Fig. Effect of Chinese herbs on contraction of collagen gels. Cell-embedded collagen gels
were prepared according to the manufacturer‘s instructions (CELL BIOLABS, INC., cell contraction assay (catalog number CBA-201-T). (A) The surface area of collagen gels was calculated at 24 h, 48 h, and 120 h in the presence of cells only, Y10 (Y27632 at 10 µM), 1X BDM-contraction inhibitor as the controls. The surface area of collagen gels of single herbs- Dan-Shen and Ge-Gen, and herbal formula- Liu-Wei-Di-Huang-Wan and Jia-Wei-Xiao-Yao-San (5 and 10 µg/ml) was also calculated. The contraction of collagen gel was expressed in a percentage, with the surface area of the cells only serving as 100%. Similar results were obtained in three independent experiments. Values represent the mean± S.D. (B) The surface area of collagen gels was shown at 24 h in the presence of cells only (No. 1), Y10 (No. 2; Y27632 at 10 µM), 1X BDM-contraction inhibitor (No. 3) as the controls. The surface area of collagen gels of single herbs- Dan-Shen (No. 4; 5 µg/ml) and Ge-Gen (No. 5; 5
µg/ml), and herbal formula- Liu-Wei-Di-Huang-Wan (No. 6; 5 µg/ml) and Jia-Wei-Xiao-Yao-San (No. 7; 5 µg/ml) was also shown. (C) The surface area of collagen gels was shown at 48 h in the presence of cells only (No. 1), Y10 (No. 2; Y27632 at 10 µM), 1X BDM-contraction inhibitor (No. 3) as the controls. The surface area of collagen gels of single herbs- Dan-Shen (No. 4; 5 µg/ml) and Ge-Gen (No. 5; 5 µg/ml), and herbal formula- Liu-Wei-Di-Huang-Wan (No. 6; 5 µg/ml) and Jia-Wei-Xiao-Yao-San (No. 7; 5 µg/ml) was also shown. (D) The surface area of collagen gels was shown at 120 h in the presence of cells only (No. 1), Y10 (No. 2; Y27632 at 10 µM), 1X BDM-contraction inhibitor (No. 3) as the controls. The surface area of collagen gels of single herbs- Dan-Shen (No. 4; 5 µg/ml) and Ge-Gen (No. 5; 5 µg/ml), and herbal formula- Liu-Wei-Di-Huang-Wan (No. 6; 5 µg/ml) and Jia-Wei-Xiao-Yao-San (No. 7; 5 µg/ml) was also shown.
S3 Fig. Original uncropped and unadjusted blots of Fig. 3. (A) herbal formulas; (B) single herbs. The
antibodies (anti-Phospho-MLC, anti- Total-MLC, and anti-β-actin) used here were shown in the left of the S3 Fig.
S1 File. Supporting tables for Chinese herbal medicine treatment in hypertension individuals among type 2 diabetes patients. Herbal composition of twelve most common herbal formulas and single herbs prescribed by TCM doctors for the treatment of hypertension individuals among type 2 diabetes patients (Table A). Results of conditional multivariable logistic regression on the occurrence of acute myocardial infarction (Table B). Results of conditional
multivariable logistic regression on the occurrence of ischemic stroke (Table C). Results of conditional multivariable logistic regression on the occurrence of hemorrhagic stroke (Table D).Results of conditional multivariable logistic regression on the occurrence of amputation (Table E).Results of conditional multivariable logistic regression on the occurrence of nephropathy (Table F).Results of conditional multivariable logistic regression on the occurrence of death (Table G).Regular medical treatment (from diabetes to index day) among type 2 diabetes patients according to CHM usage (Table H).Regular medical treatment (from index day to index day +365) among type 2 diabetes patients according to CHM usage (Table I).