Background and Purpose: Quality of life (QOL) is the paramount goal of end-of-life care. However, there is no Chinese language instrument for measuring QOL that has been shown to have adequate psychometric properties for Taiwanese patients with terminal cancer. The purpose of this study was to examine the psychometric properties of a Chinese language version of the McGill Quality of Life questionnaire (MQOL-Taiwan version).
Methods: The original English version of the MQOL questionnaire was translated into Chinese, and administered to 64 Taiwanese patients with terminal cancer for psychometric testing (factor structures and various types of reliability and validity). The cultural equivalence of the translation was tested by content validity index. Statistical analysis included exploratory factor analysis, Pearson’s product moment correlation coefficient, and the calculation of Cronbach’s alpha (α).
Results: Findings on the validity and reliability of the MQOL-Taiwan version were as follows. The value of content validity was 0.98. The range of the correlations between an item and its domain was 0.59 to 0.96 (all p < 0.05), and for inter-domain was 0.28 to 0.52 (all p < 0.05). The 4 domains of the original MQOL emerged as the 4 dominant factors (64% total variance explained) in the MQOL-Taiwan version, namely the domains of physical symptoms, psychological symptoms, existential well-being, and support. The internal consistency (Cronbach’s α) coefficient of the whole MQOL-Taiwan version was 0.83, and those for the 4 domains ranged from 0.69 to 0.90. For the convergent and divergent validity, the MQOL-Taiwan version physical domain was moderately and significantly (r = -0.44, p < 0.05) correlated with the performance status rating of the Eastern Cooperative Oncology Group-Performance Status Rating (ECOG-PSR). The MQOL-Taiwan version psychological, existential, and support domains were not significantly correlated to the ECOG-PSR.
Conclusions: The MQOL-Taiwan version demonstrated an acceptable level of reliability, validity and equivalency in the initial cross-cultural validation. These findings indicate the suitability of this QOL measure for clinical and research use in Taiwanese patients with terminal cancer.
Key words: Quality of life; Neoplasms; Palliative care; Psychometrics; Taiwan.
J Formos Med Assoc 2003;102:97-104
1School of Nursing, College of Medicine and Hospital, The National Taiwan University, Taipei; 2School of Nursing,
University of Washington, USA; 3Departments of Family Medicine and Social Medicine, College of Medicine and Hospital,
The National Taiwan University, Taipei, Taiwan.
Received: 6 June 2002 Revised: 4 July 2002 Accepted: 10 December 2002
Reprint requests and correspondence to: Wen-Yu Hu, School of Nursing, College of Medicine, The National Taiwan University, No. 1, Jen-Ai Road, Sec. 1, Taipei, Taiwan.
P
SYCHOMETRIC
T
ESTING
OF
THE
T
RANSLATED
M
C
G
ILL
Q
UALITY
OF
L
IFE
Q
UESTIONNAIRE
-T
AIWAN
V
ERSION
IN
P
ATIENTS
W
ITH
T
ERMINAL
C
ANCER
Wen-Yu Hu,1 Yu-Tzu Dai,1 Donna Berry,2 and Tai-Yuan Chiu3
Cancer has been the leading cause of death in Taiwan since 1982. Currently, around 30,000 people die of cancer each year.1 Huang estimated that the demand for terminal cancer care in Taiwan would be 3 times the present amount by 2012.2 The ultimate goal of palliative care is the achievement of the best quality of life (QOL) for patients and their families.3 There-fore, when a cure or the prolongation of life is no longer possible, QOL becomes the most appropriate and important indicator of outcome for evaluating the effectiveness of hospice and palliative care pro-grams.4 Unfortunately, there is no Chinese-language
version of a valid and reliable QOL instrument specific-ally designed for terminal patients in Taiwan.5,6
To offer an appropriate and culturally sensitive QOL instrument for Taiwanese patients with terminal cancer and to help healthcare providers in Taiwan to make better clinical decisions, a Chinese-language version of a QOL instrument with adequate reliability and validity is needed. Previously, we used the 8 key attributes of health status and QOL instruments and the criteria developed by the Scientific Advisory Com-mittee of the Medical Outcomes Trust to evaluate the suitability of existing QOL instruments for application
in Taiwan, and selected the McGill Quality of Life questionnaire (MQOL) for use in this study.7–14
Considering the exacting requirements of cross-cultural adaptation and language translation,a cross-cultural validation of the MQOL is needed before it can be applied in Taiwan.15,16 The purposes of this study were as follows: 1) to establish evidence regard-ing the conceptual and lregard-inguistic equivalency of the translated MQOL (MQOL-Taiwan version) and the English version of the MQOL during the translation process; 2) to construct the subscale structure of the translated MQOL-Taiwan version questionnaire; and 3) to establish the psychometric properties (validity and reliability) of the MQOL-Taiwan version used in terminal cancer patients through psychometric testing.
M
ethods
Subjects
A purposive sampling method was used to select patients with terminal illness in the palliative care unit and oncology wards of National Taiwan University Hospital. Patients who met the following inclusion criteria were considered eligible for the study: 1) advanced stages of cancer, not responsive to curative treatment; 2) life expectancy less than 6 months based on the primary physician’s judgement; 3) the patient was conscious and could communicate readily; 4) the patient gave meaningful informed consent; and 5) the patient was not so weak that the completion of the questionnaire became a burden. The physicians and the primary nurses involved in the care of the patients determined the eligibility based on these criteria. Although 154 terminal cancer patients were initially considered eligible for the study, only 74 of them (48.1%) and their families accepted the person-al interview. However, 10 of these patients could not complete the process of interview due to deterioration of their physical condition. Thus, 64 of the 74 patients (86.5%) completed the interview.
Data collection procedure
Interviewers explained the process of the study in detail and obtained voluntary agreement from the patients through written or oral consent. Patients chose whether to complete the questionnaire with-out assistance or by having the questions read aloud by the interviewers. Demographic information was collected from the patients’ charts, nurses, physicians, and/or from the patients themselves. Patients could end an interview at any time. The average time required to complete a questionnaire was 30 minutes (range, 15 to 45 minutes).
Instruments
The instruments used consisted of 4 parts: demo-graphic data; data on the physical symptoms checklist17; the Eastern Cooperative Oncology Group-Performance Status Rating (ECOG-PSR); and the McGill Quality of Life questionnaire (MQOL).
The McGill Quality of Life Questionnaire was developed by Cohen and Mount (1995) and has been shown to have good acceptability, internal consistency, test/retest reliability, and validity. The responsiveness to changes in life quality of this instrument has also been demonstrated,9 especially for palliative care patients. It is a self-reported instrument and consists of 16 items concerning issues that have had an impact on a patient’s QOL over the previous 2 days. A complete list of items on the MQOL questionnaire is provided in Appendix A. The response categories are based on a numerical rating scale, ranging from “0” (the least desirable) to “10” (the most desirable). Scores of items 1 to 3 and 5 to 8 are transposed. The MQOL includes 4 domains: physical symptoms; psychological well-being; existential well-being; and support.11
The Eastern Cooperative Oncology Group (ECOG) developed the ECOG-PSR in 1982 to evaluate the performance status of patients during therapy. It is ordinal in nature and on a scale from 0 (normal) to 4 (totally confined to the bed or chair).18 The ECOG-PSR, which is easier to use and more commonly used to assess the changes in the performance status of terminal cancer patients than the MQOL, was chosen in this study to reflect the extent to which the MQOL-Taiwan version correlated with similar and dissimilar constructs of other established measures of QOL.
Validation process for the translated MQOL
Permission was obtained from the original authors to use the English version of the MQOL questionnaire. One of the investigators in our study, who is bilingual in Chinese and English, made an initial direct trans-lation from the original English questionnaire. The Chinese translation sought to maintain the meaning and scale of the original. A bilingual (English and Chinese) and bicultural (US and Taiwan) physician working in our palliative care unit, then assessed the accuracy of the Chinese language version. This physician, who had previously lived in the US for 8 years and studied in an English language environment during her formal education, also performed a ‘back-translation’ of the MQOL, from Chinese to English. Finally, 2 measures of comparison — comparability of language and similarity of interpretability — were used to evaluate the success of the translation process. A native English-speaking American nun, specializ-ing in nursspecializ-ing and who had lived in Taiwan for more than 10 years, and 5 fluent English speakers who
had expertise in palliative care, were also invited to compare the formal similarity of words, phrases, sentences, and meaning between the original ques-tionnaire and the back-translated English version.
The cultural/language equivalence of each item in the MQOL-Taiwan version was appraised by use of the Likert scale ranging from 1 (not at all comparable and similar) to 5 (extremely comparable and similar). The means of the 16 items were above 4.0 with standard deviations of less than 1.0. Except for item 15, all other 15 items in the MQOL were rated 4 or 5, which yielded a 100% agreement for these 15 items. This result is very comparable in language (form) and very similar in interpretation (meaning) to the original instrument. Conflicting meanings in the questionnaire were revised. It was then success-fully back-translated from Chinese into English. The equivalence of the English and Chinese language versions was verified. Prior to this study, 11 experts, including 4 physicians, 4 nurses, 1 psychologist, 1 social worker, and 1 chaplain (Buddhist), were invited to rate how adequately the items in the MQOL-Taiwan version matched the dimension of QOL for content validity.
Validity testing methods
A content validity index (CVI), using a Likert scale ranging from 1 (not relevant) to 5 (very relevant and succinct), was used to determine the content validity of the MQOL-Taiwan version. The CVI score was computed by summing the percentage of agreement of all items that were given a rating of “4” or “5” by the experts.19 Prior to data analysis, scores for items 1 to 3 and 5 to 8 were transposed, so that a score of “0” always indicated the least desirable situation and “10” the most desirable situation. Data analysis was carried out using Statistical Package for Social Sciences (SPSS) version 10.0 for Windows statistical software. The MQOL total and subscales data were screened and found to have a normal distribution, indicating the appropriateness of parametric statistics.
Exploratory factor analysis (EFA) using principal components analysis with orthogonal varimax rotation was performed for all the MQOL-Taiwan version items scores, to extract the domains and examine the con-struct validity. Cronbach’s α value was used to evaluate the internal consistency (reliability) of MQOL and its domains. Convergent and divergent validity, the important components of construct validity, reflect the extent to which the translated MQOL-Taiwan version correlates with similar and different con-structs of another established measure of QOL. The Pearson’s correlation coefficients were used to examine the correlation among the domains of the MQOL-Taiwan version with physical function
performance status of the ECOG-PSR. The content validity was evaluated by calculating Pearson’s cor-relation coefficients between each item and its domain and inter-domains.20 The level of significance was set at p < 0.05.
R
esults
Characteristics of the study participants
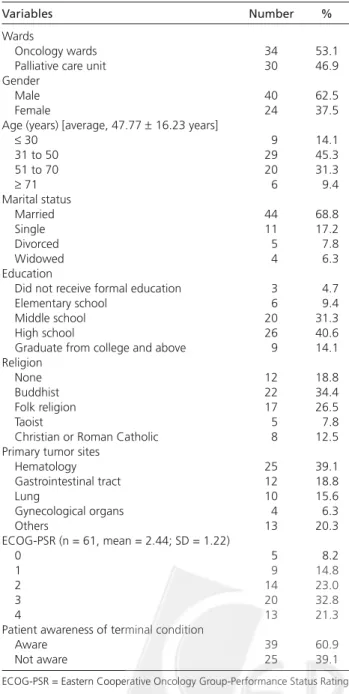
Table 1 shows the demographic characteristics of the participants. The 64 patients were almost equally divided between the palliative care unit (46.9%) and the oncology wards (53.1%). The participants were Table 1. Demographic characteristics of patients with
terminal cancer (n = 64).
Variables Number %
Wards
Oncology wards 34 53.1
Palliative care unit 30 46.9 Gender
Male 40 62.5
Female 24 37.5
Age (years) [average, 47.77 ± 16.23 years]
≤ 30 9 14.1 31 to 50 29 45.3 51 to 70 20 31.3 ≥ 71 6 9.4 Marital status Married 44 68.8 Single 11 17.2 Divorced 5 7.8 Widowed 4 6.3 Education
Did not receive formal education 3 4.7
Elementary school 6 9.4
Middle school 20 31.3
High school 26 40.6
Graduate from college and above 9 14.1 Religion
None 12 18.8
Buddhist 22 34.4
Folk religion 17 26.5
Taoist 5 7.8
Christian or Roman Catholic 8 12.5 Primary tumor sites
Hematology 25 39.1 Gastrointestinal tract 12 18.8 Lung 10 15.6 Gynecological organs 4 6.3 Others 13 20.3 ECOG-PSR (n = 61, mean = 2.44; SD = 1.22) 0 5 8.2 1 9 14.8 2 14 23.0 3 20 32.8 4 13 21.3
Patient awareness of terminal condition
Aware 39 60.9
Not aware 25 39.1
Table 3. Descriptive statistics for MQOL subscales and items
and SIS (n = 64).
Global QOL scores and items* Mean score (SD) Rank Physical symptoms 4.2 (3.2)
1) First physical problem 2.8 (3.2) 16 2) Second physical problem 4.1 (3.4) 15 3) Third physical problem 5.5 (3.5) 10.5 Physical well-being 4.2 (2.8)
4) Physically well/terrible 4.2 (2.8) 14 Psychological symptoms† 6.1 (2.0)
5) Depressed 6.3 (2.6) 7
6) Nervous and worried 5.8 (2.9) 9
7) Time did 6.4 (2.3) 5.5 8) Fear future 6.1 (2.9) 8 Existential well-being‡ 6.1 (2.0) 9) Existence meaningful 5.5 (2.9) 10.5 10) Achieving goals 4.9 (3.2) 13 11) Life worthless 6.4 (2.4) 5.5 12) Control over time 5.1 (3.2) 12 13) Like self§ 7.4 (2.5) 3.5
14) Every day is a gift 7.4 (2.8) 3.5
Support❘❘ 8.0 (2.0)
15) World is caring 7.6 (2.6) 2 16) Felt supported 8.4 (2.0) 1
* Score ranges are 0 to 10 except where indicated. †1 to 10. ‡1.6 to 10. §0 to
9.5. ❘❘2.7 to 10.
MQOL = McGill Quality of Life questionnaire; QOL = quality of life; SIS = single-item scale.
mostly male (62.5%), with an average age of 47.8 years. The patients mostly practiced Buddhism (34.4%) or a folk religion (26.5%). Only 60.1% of the participants were fully aware and knowledgeable of the terminal nature of their disease and their prognosis. The pri-mary sites of cancer were: hematological (39.1%); the gastrointestinal tract (18.8%); the lungs (15.6%); and the gynecological organs (6.3%). The 10 most frequent physical symptoms measured by the 26-item physical symptoms checklist are shown in Table 2. These 10 in descending order of occurrence are: pain (51.6%); weakness or fatigue (40.6%); dry mouth (39.1%); abdominal distension (29.7%); dyspnea (25.0%); anorexia (21.9%); constipation (21.9%); insomnia (21.9%); fever (21.9%); and nausea/ vomiting (21.9%). The mean value of the ECOG-PSR was 2.44.
Descriptive statistics of the MQOL-Taiwan
version
Data for the domains and each item of the MQOL-Taiwan version are shown in Table 3. The mean value of the MQOL total score was 6.1 ± 1.5. The mean values of the MQOL subscales ranked from highest to lowest were: support (8.0 ± 2.0); existential well-being (6.1 ± 2.0); psychological symptoms (6.1 ± 2.0); physical symptoms (4.2 ± 3.2); and physical well-being (4.2 ± 2.8). The item with the highest mean score was the item: “felt support” (8.4 ± 2.0), and the lowest mean score was the item on the first physical symptom (2.8 ± 3.2).
Psychometric properties of the
MQOL-Taiwan version
1. Validity
The CVI score of the MQOL-Taiwan version is 0.984 (relevant and succinct), computed by summing 0.327 from the “4” ratings and 0.657 from the “5” ratings on all items. Except for items 7 (90.0%) and 14 (81.8%), all of the other 14 items were rated 4 or 5, yielding 100% agreement. The range of the correlations
between each item and its domain was 0.59 to 0.96 (all p < 0.01), and for inter-domains was in the range 0.28 to 0.52 (all p < 0.05). These results show that the MQOL-Taiwan version has good content validity.
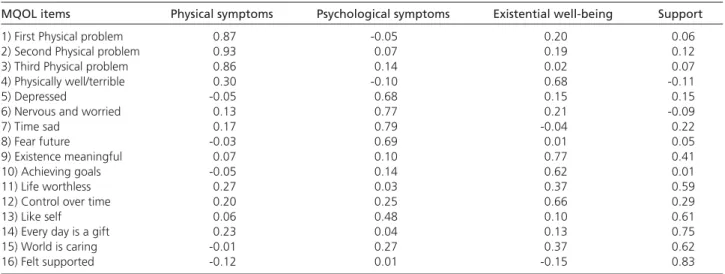
Bartlett’s test of sphericity (BT) and the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy were performed initially for exploratory factor analysis (EFA). The results showed that the data were appro-priate for EFA (KMO = 0.72; BT = 447.35, p < 0.001). Principal components analysis with orthogonal varimax rotation was performed on the 16 items of the MQOL-Taiwan version, excluding the single-item scale.
The number of factors to be extracted was deter-mined by the examination of Eigen values (greater than 1.0) and the Cattell’s screen test. Based on these results and considering the theoretical basis of previous literature for QOL, 4 domains (physical symptoms, psychological being, existential well-being, and support) were extracted (Table 4). These 4 domains accounted for 64% of the total variance of the variables. The EFA result was slightly different from the English version of the MQOL. Items 13 and 14 had comparatively relatively larger factor loadings on the psychological symptoms domain (0.48) and support domain (0.75), respectively, although they originally belonged to the existential well-being domain. However, items 13 and 14 demonstrated a higher correlation with the existential well-being domain than with the psychological symptoms domain Table 2. Frequency and the degree of disturbance of physical
symptoms (n = 64).
Symptoms Frequency Degree of disturbance n (%) Rank Mean (SD) Rank Pain 33 (51.6) 1 1.31 (1.27) 1 Weakness or fatigue 26 (40.6) 2 1.11 (1.31) 3 Dry mouth 25 (39.1) 3 1.13 (1.45) 2 Abdominal distension 19 (29.7) 4 0.92 (1.33) 4 Anorexia 14 (21.9) 6.2 0.82 (1.28) 5 Constipation 14 (21.9) 6.2 0.72 (1.18) 6 Dyspnea 16 (25.0) 5 0.71 (1.20) 7 Insomnia 14 (21.9) 6.2 0.67 (1.26) 8 Fever 14 (21.9) 6.2 0.60 (1.12) 9 Nausea and vomiting 14 (21.9) 6.2 0.54 (0.99) 10
(r = 0.65 vs r = 0.45) and the support domain (r = 0.68
vs r = 0.43), respectively. These results imply that
items 13 and 14 should remain grouped under the existential well-being domain in the MQOL-Taiwan version.
2. Reliability
The internal consistency (reliability) of the MQOL total score and each MQOL domain was calculated using Cronbach’s α value. The internal consistency of MQOL domains and the 16-item questionnaire were respectable (α > 0.70), with the exception of the support domain (16-item MQOL, α = 0.83; physical symptoms, α = 0.90; psychological symptoms, α = 0.77; existential well-being, α = 0.73; support, α = 0.69). The overall Cronbach’s α coefficient for the 16-item
Table 4. Varimax rotated factor matrix for the translated MQOL-Taiwan version items (n = 64).
MQOL items Physical symptoms Psychological symptoms Existential well-being Support
1) First Physical problem 0.87 -0.05 0.20 0.06
2) Second Physical problem 0.93 0.07 0.19 0.12
3) Third Physical problem 0.86 0.14 0.02 0.07
4) Physically well/terrible 0.30 -0.10 0.68 -0.11
5) Depressed -0.05 0.68 0.15 0.15
6) Nervous and worried 0.13 0.77 0.21 -0.09
7) Time sad 0.17 0.79 -0.04 0.22
8) Fear future -0.03 0.69 0.01 0.05
9) Existence meaningful 0.07 0.10 0.77 0.41
10) Achieving goals -0.05 0.14 0.62 0.01
11) Life worthless 0.27 0.03 0.37 0.59
12) Control over time 0.20 0.25 0.66 0.29
13) Like self 0.06 0.48 0.10 0.61
14) Every day is a gift 0.23 0.04 0.13 0.75
15) World is caring -0.01 0.27 0.37 0.62
16) Felt supported -0.12 0.01 -0.15 0.83
MQOL = McGill Quality of Life questionnaire.
scale was 0.83 (Table 5). The results of the EFA for the construct validity of the translated MQOL-Taiwan ver-sion was acceptable, and corresponded to the results of studies by Cohen et al for palliative care patients.8
The underlying hypotheses of this study included that the physical domain has a moderate or high correlation with the performance status of ECOG-PSR, and that the psychological, existential, and support domains have low or no correlation with ECOG-PSR. As expected, the results showed that the MQOL physical domain was moderately and significantly correlated with the performance status rating of ECOG-PSR(r = -0.44, p < 0.001). The MQOL psychological, existential, and support domains did not have significant correlations to the ECOG-PSR in performance status (r = -0.06, p > 0.05; r = 0.04, Table 5. Summary of the psychometric properties of the translated MQOL-Taiwan version.
Reliability Internal consistency Physical symptoms Cronbach’s α: 0.90 Psychological well-being Cronbach’s α: 0.77 Existential well-being Cronbach’s α: 0.73 Support Cronbach’s α: 0.69 MQOL total score Cronbach’s α: 0.83
Validity Language/cultural Each item (16 items) 100% agreement that were given a rating of “4” or “5” equivalency (comparable and similar) by 5 experts except for SIS (80%) and
item 15 (80%)
Content validity Each item (16 items) 100% agreement (very relevant and succinct) by 11 experts except for item 7 (90%) and item 14 (81.8%)
Whole questionnaire CVI = 0.984
Item/hypothesized domain r = 0.59 to 0.86 (p < 0.01) Inter-domain r = 0.28 to 0.52 (p < 0.05) Diversity/convergent
validity Each domains/ECOG-PSR Psychological, existential and support subscales uncorrelated with ECOG-PSR; physical symptoms subscale significantly correlated with ECOG-PSR (r = -0.44, p < 0.01)
Construct validity EFA Four factors were extracted 64% total of variance was explained
MQOL = McGill Quality of Life questionnaire; SIS = single-item scale; CVI = content validity index; ECOG-PSR = Eastern Cooperative Oncology Group-Performance Status Rating; EFA = exploratory factor analysis.
p > 0.05; r = -0.17, p > 0.05). Summary data of the
psychometric analyses of reliability and validity of the translated MQOL-Taiwan version are shown in Table 5.
D
iscussion
The translated MQOL-Taiwan version had good content validity from the results of CVI and item/ domain values, and had respectable construct validity in the results of EFA. The EFA result was slightly different from the MQOL’s original English version. Items 13 and 14 were also significantly correlated with psychological symptoms and support domains, in addition to the existential well-being domain. This difference may represent potential genuine differences between eastern and western cultures. The experiences from our interview process indicated that the English phrase “as a person” in item 13 translations into the Mandarin terms “shian-ge-ren”, was not easily understood and that patients with terminal illness emphasized their “appearance or outlook like a person” more than their “bio-psycho-social-spiritual concept of a unitary person”. Therefore, declining body functions and body image alterations lead to anxiety and depression, indicating that item 13 should be categorized as a psychological symptom in this study. The English word “a gift” in item 14 was considered by our patients to present enough external support to be “fu-bau” (Mandarin) in this terminal stage of illness. Therefore, in this study we viewed item 14 as part of the support domain. If items 13 and 14 belong to the existential well-being domain, translations into the Mandarin terms “hwo-de-shian-ge-ren” and “fu-chih”, respectively, may be more appropriate. Item 4 on the physical well-being domain was also treated as a single item corresponding to the English version, since this item did not load clearly with any factor in the MQOL.9,11 But it could be grouped under physical symptoms or existential well-being domain in the MQOL-Taiwan version. Pearson’s correlation coefficient of item 4 correlated somewhat better with the symptoms domain than with the exist-ential well-being domain (r = 0.34, p < 0.01; r = 0.32,
p = 0.011).
The purpose of factor analysis is to reduce the complexity of variables for convenient application in clinical practice. Using the 4 domains of physical, psychological, existential, and support, the interpret-ation and clinical applicinterpret-ations are done more easily. The results of this study suggest that item 4 be considered a physical symptoms factor because its internally consistent reliability is still acceptable (Cronbach’s α = 0.82).
As expected, 3 of the 4 MQOL domains (psycho-logical, existential, and support) showed divergent validity, but did not demonstrate convergent validity. Because the ECOG-PSR did not measure the psycho-logical, existential and support domains, so the MQOL did not correlate significantly with a dissimilar construct on the ECOG-PSR, and the ECOG-PSR did not measure the psychological, existential, and support domains. However, the physical symptoms domain showed convergent validity, but it did not demonstrate diversity validity, since the physical domain correlated significantly with a similar con-struct on the ECOG-PSR, and the ECOG-PSR did not measure the psychological, existential and support domains. Ideally, the data showing moderate to high correlation between the MQOL-Taiwan version and the established measure of a similar construct should give evidence of convergent validity, while divergent validity is demonstrated by data showing low cor-relation between the MQOL-Taiwan version with measures of different constructs. In this study, the evidence of convergent and divergent validity of the translated MQOL-Taiwan version was not adequate and was limited by the absence of correlation between the measures of the unrelated constructs.
According to the mean scores of the MQOL domains, rankings from high to low were: support; existential well-being; psychological symptoms; and physical symptoms. Although these patients with terminal illness suffered from physical symptoms that were “tremendous problems”, they still felt their lives were purposeful/meaningful/worthwhile. Terminal cancer patients are able to maintain their relationships with family, friends, and God, even in the face of remarkable functional difficulties and troublesome physical symptoms. These results suggest it is possible to maintain one’s QOL with appropriate care and to relieve suffering for those who are at the threshold of death. It is clear that QOL related to physical function and physical symptoms will inevitably decline, but the QOL in other domains may improve, as noted in other studies.20 The philosophy of palliative care is also mentioned; the patient’s physical status declines but psychological and spiritual well-being has the potential for growth.
Comparing the mean values of MQOL total and subscale scores in this study to those of Cohen et al in terminal cancer patients at 8 Canadian palliative care services11 showed similarities, except for scores on physical and existential well-being, which were lower in this study (4.2 ± 2.8 vs 5.5 ± 2.4 and 6.1 ± 2.0 vs 6.9 ± 1.7, respectively). For reasons already stated, not telling the truth and late referrals for palliative care are common among terminal cancer patients in Taiwan. Nearly 40% of the terminal patients in this
study were not fully aware and knowledgeable of the terminal nature of their disease and prognosis. Several reasons may explain this. Chinese culture is especially influenced by the Confucian thinking, which has been dominant for 5000 years. To quote the Analects of
Confucius, “if you do not recognize through to life,
how can you recognize through to death?” “Death” is also a taboo concept for Taiwanese, and death educa-tion is not popular in the medical curriculum, which emphasizes only cures over caring and considers death to be a failure of medical treatment.
The translated MQOL-Taiwan version had statis-tically sufficient (acceptable to respectable) levels of reliability, validity, and equivalency in its psycho-metrical testing to be applicable for future use in Taiwan. Validation is a continuous process.21 There-fore, future research should systematically test the diversity/convergent validity and applicability, select the similar and dissimilar construct measurements (the multitrait-multimethod matrix), and compare correlations of constructs between measures. This will enable the division of covariation into “method” and “construct” sources, allowing more precise statements about construct validity.
Construct validity verified by confirmatory factor analysis can be performed to confirm the factor struc-ture when a satisfactory sample size is available. Longi-tudinal study should be performed to demonstrate sufficient stability (test-retest reliability) and respon-siveness of the MQOL questionnaire in Taiwanese subjects.
Any instrument translated from a different language may not reflect certain cultural characteris-tics or connotative meanings of the original version. A limitation of this study may have been that the translated MQOL-Taiwan version fails to appreciate the same linguistic meanings of the translated items for various Taiwanese linguistic subgroups, such as lay Taiwanese and Hakka. We found some native items which could be included for cross-cultural and within-cultural comparisons during the interviewing process, that might be used in the development of a modified MQOL-Taiwan version in future. Alternatively, inclus-ion of some native items from qualitative research for cross-cultural and within-cultural comparisons could be used to develop a modified MQOL-Taiwan version. Development of a short-form of the MQOL-Taiwan version would be desirable in being faster and easier to use, and would also avoid placing excessive burden on these physically frail patients in clinical care.
ACKNOWLEDGMENTS: Support for this study was
provided by the National Science Council of Taiwan. The authors would like to thank Dr. Robin Cohen and her team for their permission to translate the
English version MQOL into Taiwanese. We also appreciate the useful comments and help from statistical consultant Dr. Kevin Cain of the University of Washington, as well as Professor Ching-Yu Chen, Professor Chang-Yao Hsieh, Professor Yueh-Chih Chen, Professor Grace Yao, and Professor Jung-Der Wang of the National Taiwan University. We would like to thank the 64 patients who participated in the research.
R
eferences
1. Department of Health, The Executive Yuan, Republic of China. Vital Statistics, Republic of China 1998. Taipei: Department of Health, The Executive Yuan, Republic of China; 1999. 2. Huang FY: The estimation of palliative/hospice care demand for
terminal cancer patients [dissertation]. Chia-Yi National Chung Chen University; 1994. [In Chinese].
3. World Health Organization. Cancer pain relief and palliative care: report of a WHO expert Committee. Geneva, Switzerland: World Health Organization; 1990.
4. Zimbelman J: Good life, good death, and the right to die: ethical considerations for decisions at the end of life. J Prof Nurs 1994; 10:22-37.
5. Luh DL: An overview of quality-of-life research in Taiwan. Chinese
Journal of Public Health (Taipei) 1998;17:442-57. [In Chinese;
English abstract].
6. Hu WY: Assessment of quality-of-life with advanced cancer patient. Taiwan Journal of Hospice Palliative Care (Taipei) 1998; 10:3-10. [In Chinese; English abstract].
7. The Scientific Advisory Committee of the Medical Outcomes Trust: Assessing health status and quality-of-life instruments: attributes and review criteria. Quality of Life Research 2002;11: 193-205.
8. Cohen SR, Mount BM, Bruera E, et al: Validity of the McGill Quality of Life Questionnaire in the palliative care setting: a multi-centre Canadian study demonstrating the importance of the existential domain. Palliat Med 1997;11:3-20.
9. Cohen SR, Mount BM: Quality of life in terminal illness: defining and measuring subjective well-being in the dying. J Palliat Care 1992;8:40-5.
10. Cohen SR, Mount BM, Tomas JJ, et al: Existential well-being is an important determinant of quality of life. Evidence from the McGill Quality of Life Questionnaire. Cancer 1996;77:576-86. 11. Hu WY, Chiu TY, Bhikkhu HM, et al: Spiritual needs of terminal
cancer patients from the viewpoint of medical professionals.
Formosan J Med (Taipei) 1999;3:8-19. [In Chinese; English
abstract].
12. Cohen SR, Boston P, Mount BM, et al: Changes in quality of life following admission to palliative care units. Palliat Med 2001; 15:361-71.
13. McMillan SC, Weitzner M: Quality of life in cancer patients: Use of a revised hospice index. Cancer Pract 1998;6:282-8. 14. Pratheepawanit N, Salek MS, Finlay IG: The applicability of
quality-of-life assessment in palliative care: comparing two quality-of-life measures. Palliat Med 1999;13:325-34. 15. Sperber AD, Devellis RF, Boehlecke B: Cross-cultural translation:
methodology and validation. J Cross Cult Psychol 1994;25: 501-24.
16. Nunnaly JC: Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994 p. 445-541.
17. Chiu TY, Hu WY, Chen CY: Prevalence and severity of symptoms in terminal cancer patients: A study in Taiwan. Support Care
Cancer 2000;8:311-3.
Appendix A. Items of the McGill Quality of Life questionnaire.
Domain Item no. Item content
D1. Physical symptoms 1 One troublesome symptom has been: no problem/tremendous problem 2 Another troublesome symptom has been: no problem/tremendous problem 3 A third troublesome symptom has been: no problem/tremendous problem 4 I have felt: physically terrible/physically well
D2. Psychological well-being 5 I have been depressed: not at all/extremely 6 I have been nervous or worried: not at all/extremely 7 How much of the time did you feel sad?: never/always 8 When I thought of the future, I was: not afraid/terrified
D3. Existential well-being 9 My life has been: utterly meaningless and without purpose/very purposeful and meaningful 10 When I thought about my whole life, I felt that in achieving life goals I have:
made no progress whatsoever / progressed to complete fulfillment 11 When I thought about my life, I felt that my life to this point has been:
completely worthless/very worthwhile
12 I have felt that I have: no control over my life/complete control over my life 13 I felt good about myself as a person: completely disagree/completely agree 14 To me, the past two (2) days were: a burden / a gift
D4. Support 15 The world has been: an impersonal unfeeling place/caring and responsive to my needs 16 I have felt supported: not at all/completely
18. Oken MM, Creech RH, Tormey DC, et al: Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol 1982;5:649-55.
19. Lynn MR: Determination and quantification of content validity.
Nurs Res 1986;35:382-5.
20. Yang KP, Yin TJ: Defining the content domain health-related quality of life for terminally ill cancer patients. Nurs Research
(Taipei) 1999;7:129-143. [In Chinese; English abstract].
21. Goodwin LD, Goodwin WL: Focus on psychometrics: estimating construct validity. Res Nurs Health 1991;14:235-43.