ORIGINAL PAPER
Using Health Smart Cards to Check Drug Allergy History:
The Perspective from Taiwan
’s Experiences
Min-Huei Hsu&Ju-Chuan Yen&Wen-Ta Chiu& Shu-Ling Tsai&Chien-Tsai Liu&Yu-Chuan Li
Received: 12 July 2009 / Accepted: 15 October 2009
# Springer Science + Business Media, LLC 2009
Abstract In Taiwan, national health insurance coverage began in 1994, and the Bureau of National Health Insurance has issued health smart cards since 2004. In addition to tracking medical reimbursements, these smart cards store healthcare information, including electronic prescriptions, medical procedure and vaccination records, drug allergy histories, and information about a patient’s willingness to be an organ donor. We conducted this study 4 years after the smart cards had been introduced in order to review how drug allergy history is recorded using this system. Our results reveal that the drug allergy histories are
incomplete in many cases, and the format used to record a patient’s drug allergy history is not consistent. We offer suggestions to promote the standardization of drug allergy history records.
Keywords Health smart cards . National health insurance . Drug allergy history . Hospital information system
Introduction
In 1972, a French inventor named Roland Moreno introduced the concept of the smart card as a medium for electronic commerce [1]. Since then this credit card-sized card, featuring an embedded microprocessor has been used in many ways. The cards have been deployed for mass rapid transportation (MRT), to control access to buildings and offices, as administrative tools for students on campuses, and for electronic payments. Smart cards feature integrated encryption keys that help prevent fraud, and they are equipped with memory chips that can be both read and reprogrammed. Their capacity, however, is usually limited to between 30 and 100 kb.
Taiwan’s Bureau of National Health Insurance (TBNHI) has implemented the National Health Insurance (NHI) program since March 1, 1994. By law, all individuals in Taiwan must be enrolled in the NHI program. Initially, people in Taiwan used a paper-based insurance card to access healthcare services. To help control (contain) costs, facilitate electronic claims, and improve healthcare quality, TBNHI launched a pilot project in November 1999 in Pen-Hu islands, where people can use smart cards instead [2]. The cards were deployed nationwide on January 1, 2004. So far, 23 million patient health cards and 345,000 healthcare professional (providers’) cards have been issued. M.-H. Hsu
Graduate Institute of Medical Sciences, Taipei Medical University, Taipei, Taiwan
M.-H. Hsu
:
C.-T. Liu:
Y.-C. Li (*)Graduate Institute of Biomedical informatics, Taipei Medical University,
250 Wu-Xin Street, Taipei, Taiwan 110
e-mail: d102090010@tmu.edu.tw J.-C. Yen
Graduate Institute of Humanities in Medicine, Taipei Medical University,
Taipei, Taiwan J.-C. Yen
Department of Ophthalmology, Taipei City Hospital, Zhongxiao Branch,
Taipei, Taiwan W.-T. Chiu
School of Medicine, Taipei Medical University, Taipei, Taiwan
S.-L. Tsai
Medical Affairs Division, Bureau of National Health Insurance, Taipei, Taiwan
J Med Syst
Initially, these healthcare smart cards were used mainly to track TBNHI reimbursements, but they are also used to store healthcare data such as electronic prescriptions, medical procedures, vaccination records, drug allergy histories, and information about an individual’s willingness to be an organ donor. Care providers have to use their professional cards as the key to access healthcare data stored on patients’ health smart card.
Before switching to smart cards, TBNHI had used paper cards for 8 years. These paper cards featured six printed spaces, and healthcare providers stamped the date on each patient’s card after every visit. After a patient had visited a healthcare institution six times, the card would be full and had to be renewed to permit continued access to services. Managing this paper-based health insurance system was expensive, and efforts to cut costs were an important motivation for the switch to smart cards. The most important function of smart cards today is to allow healthcare institutions to have their fees reimbursed by the TBNHI [2]. Each visit to a hospital (healthcare provider), a patient must present their cards. The hospital (healthcare provider) reads a visit serial number from and writes the information required by the BNHI into the cards. The visit serial number is used for electronic claims [2].
Medication errors are the most common and costly medical errors. According to Johnson’s 1994 study [3], medication errors in ambulatory settings in the United States cost up to 76.6 billion USD each year. Checking for drug allergies history helps to reduce the risk of preventable medication errors. In their study of prescription errors, Laesar et al. [4] found that up to 12.9% of medication errors occurred when providers missed a patient’s history of allergic reaction to a medication of the same class. Although this constitutes a relatively small percentage of medication errors, the consequences of a drug allergy can be catastrophic and sometimes even deadly. Drug allergy history, therefore, should be a standard component of patient assessment to prevent medication errors.
In Taiwan, individuals are free to visit any medical institution according to their personal preference and willingness to pay. Patients can visit different physicians across various medical institutions as often as they wish. As a result, it can be difficult to reconcile each patient’s drug allergy history, since this history may be documented by a variety of medical institutions throughout Taiwan. The use of health insurance cards that feature drug allergy data might help resolve this issue.
A health smart card can store up to three drug items that may cause allergy to the cardholder. Healthcare providers can read/write from/to the card through a set of application program interfaces (APIs), which are distributed by the BNHI and are free of charge. The APIs are developed on an open platform (Java™). Healthcare providers are free to
develop their own systems and to determine what types of data their systems can record on the cards. Since there is no standard way to record drug allergy information, we decided to conduct a review to the content of drug allergy histories stored on the smart cards after they had been in use for 4 years.
We choose the drug allergy history on the health smart cards as the study target because it is not as complicated as medication record and the drug allergy history is more complete in the recording on health smart cards.
Study design
We obtained consents from individuals who had been admitted to the Taipei Medical University-Wan Fang Hospital from July 1, 2008 to February 28, 2009. The drug allergy histories of a patient can be retrieved by a card reader which requires insertion of both the patient’s smart cards and a health professional card simultaneously for the security reason. A card can store up to three drug allergy records. The retrieved drug allergy data records were pooled in a common depository for further analysis.
Physicians at the Wan Fang Hospital would record patients’ drug allergy histories in the hospital information system (HIS) as well as on the smart cards. The hospital’s records were reviewed and coded by pharmacists. Recording drug allergy history is mandatory in the hospital before using computerized physician order entry (CPOE) system to prescribe any medication. If a patient does not have any known drug allergies, physicians must record “no known drug allergy history” in the hospital information system. In this study, we compared the drug allergy histories recorded on patients’ health smart cards with the records stored in the hospital information system.
This study was approved by the institutional review board at the Wan-Fang Hospital.
Results
In total, 15,124 inpatients were admitted to the Wan Fang Hospital from July 1, 2008 to February 28, 2009, and 14,776 of these individuals held readable smart cards. And totally there were 87,178 records of visits were recorded. Among them, there were 59,122 visits were visits to the Wan Fang Hospital and the other 28,056 visits were those to other healthcare Institutes including the clinics. In average, there were 5.90 records of visit history on the health smart cards which were read by our card reader. Two hundred and eighteen of these cards had data stored about drug allergy history, and 71 cards stated that the patient had no known drug allergies. Drug allergy data were absent in the J Med Syst
remaining 14,558 health smart cards. Drug allergy history, therefore, was recorded on 1.48% of health smart cards. According to the data stored on the smart cards, 11 patients were allergic to more than one medication.
Of the 14,776 patients with readable health smart cards, 737 (4.99%) had a drug allergy history as recorded in the hospital’s information system. Forty-two patients were allergic to more than one medication.
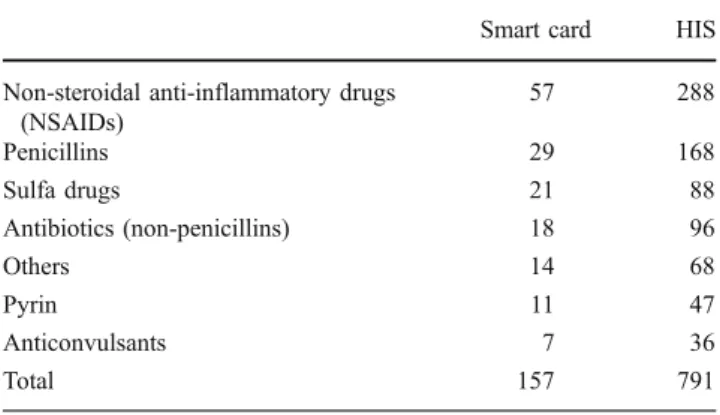
The categories of drug allergy histories as stored on the smart cards and in the HIS are shown on Table1. Allergies to non-steroidal anti-inflammatory drugs (NSAIDs) were the most common, and allergies to penicillin drugs ranked second. According to the HIS, non-penicillin antibiotics ranked third and sulfa-based drugs ranked fourth. Data from the smart cards suggested the opposite ordering. Both systems suggested other drugs, pyrine, and anticonvulsants as the fifth, sixth, and seventh most common allergies, respectively. This discrepancy may indicate that the HIS featured more complete data than the smart cards. However, the cards did feature 18 records of drug allergies that were not found in the HIS.
Drug allergy history records were not consistent on the smart cards. For example, there were nine different ways to express an absence of drug allergies. These were:
1. According to the patient, there exists no drug allergy history.
2. According to the family, there exists no drug allergy history.
3. Nil.
4. NP (Nothing in particular). 5. NKA (No known allergy).
6. No allergic (reaction) to food or drug was noted. 7. None.
8. No.
9. Deny or Denied.
Discussion
Diverse documentation of drug allergy history
The data stored on the smart cards are extremely diverse, and our results suggest information related to drug allergies can be recorded on the cards in a variety of ways. In Kuperman’s 2003 study of three academic medical hospitals, a similar problem was encountered in respect of physicians’ use of either NKA (no known allergy) or NKDA (no known drug allergy) [4].
Inconsistency in drug allergy records
The lack of a consistent approach to drug allergy history records is an important finding of this study. In Kuperman et al.’s study [5], similar variability was noted but this was the result of different information technology systems and physicians’ behavioral patterns. In our study, however, health smart cards are a national standard for electronic medical records. Our study also involved a more compli-cated information exchange process among more institu-tions than Kuperman’s study. A patient’s drug allergy history in electronic medical or health records can be of life-or-death importance in emergency scenarios [6, 7]. Therefore, we reiterate the importance of well-defined guidelines and specifications for how to store drug allergy history data. Such guidelines would facilitate these records to better meet the ultimate goals of reducing costs and improving healthcare quality. We suggest that when the patient does not have a drug allergy history, this informa-tion should be recorded as NKA (No Known Allergy). If the patient does have known allergies, the applicable drugs could be recorded in a format that is compatible with the preset standard anatomical therapeutic chemical (ATC) codes. In addition, the underlying database should include cross-reaction entities. We suggest that such a database be built into the national health insurance system. This would allow healthcare institutions to upload information to TBNHI, keeping the database up-to-date and reducing medication errors and enhance patient safety eventually.
Our data’s representativeness
In our study, the health smart cards were only read at the Wan Fang Hospital. Yet, it could still be representative data in Taiwan because the institute visit history on the health smart card included not only the Wan Fang Hospital (about 2/3) but also other medical institutes (about 1/3). All the other medical institutes could read and write drug allergy history on the health smart cards.
This also explained the inconsistency of data format on health smart cards we found in this study.
Table 1 Frequency of allergic history to different categories of medication on the smart cards and in hospital information system (HIS)
Smart card HIS
Non-steroidal anti-inflammatory drugs (NSAIDs) 57 288 Penicillins 29 168 Sulfa drugs 21 88 Antibiotics (non-penicillins) 18 96 Others 14 68 Pyrin 11 47 Anticonvulsants 7 36 Total 157 791 J Med Syst
Recommendations for the future
The results of this study reveal that the inconsistency of drug allergy history recording may cause confusion in healthcare and could lead to trouble or even some untoward consequences in emergency situations. Drug allergy history should be based on the individual’s health record, and smart cards are therefore a good medium for recording this information. Due to the inconsistency of the recordings, the drug allergy history data would not be as useful as it were expected [8–11]. According to Bates, any drug allergy history should be based on extensive medical knowledge regarding anaphylaxis and the cross-sensitivities of drugs, and must be carefully assessed by physicians who treat patients with known drug intolerances. Second-generation smart cards are currently being developed in Taiwan. We suggest that the capacity for storing drug allergy history be increased, and that the recording method be standardized to promote safety.
Conclusion
The recordings of drug allergy history on health smart cards were inconsistent in Taiwan. The conduction of National Health Insurance program enables personal health informa-tion including drug allergy history could be recorded in a portable smart card and shared among various healthcare providers. However, our study has revealed that drug allergy records on Taiwan’s health smart cards are still not satisfactory. In the future, we recommend drug allergy
records on health smart cards should be standardized in Taiwan.
References
1. McElroy, D., and Turban, E., Using smart cards in electronic commerce. Int. J. Inf. Manage. 18 (No.1):61–72, 1998.
2. Liu, C. T., Yang, P. T., Yeh, Y. T., et al., The impacts of smart cards on hospital information system—An investigation of the first phase of the national health insurance smart card project in
Taiwan. Int. J. Med. Inform. 75:173–181, 2006.
3. Johnson, J. A., and Lyle, B. J., Drug-related morbidity and mortality: A cost-of-illness model. Arch. Intern. Med. 155
(18):1949–1956, 1995.
4. Lesar, T. S., Briceland, L., Stein, D. S., et al., Incidence of adverse drug events and potential adverse drug events: Implications for
prevention. JAMA. 274:29–34, 1995.
5. Kuperman, G. J., Gandhi, T. K., and Bates, D. W., Effective drug allergy checking: Methodological and operational issues. J.
Biomed. Inform. 36:70–79, 2003.
6. Jones, D., Smart cards—The key to secure and flexible health care
provision. Card Technol. 15:8, 2003.
7. Stockman, S., A healthy approach to German smart cards? Chip Talk. Card Technology Today. 19:9, 2007.
8. Kuperman, G. J., Bobb, A., Payne, T. H., et al., Medication-related clinical decision support in computerized provider order entry systems: A review. J. Am. Med. Inform. Assoc. 14:29–40, 2007. 9. Hsu, M. H., Li, Y. C., and Liu, C. T., ADRs and smart health
cards. CMAJ. 175 (4):385, 2006.
10. Lai, J. T., Hou, T. W., Yeh, C. L., and Chao, C. M., Using Healthcare IC Cards to manage the drug doses of chronic disease
patients. Comput. Biol. Med. 37 (2):206–213, 2007.
11. Ernstmann, N., Ommen, O., Neumann, M., Hammer, A., Voltz,
R., and Pfaff, H., Primary care physician’s attitude towards the
German e-health card project—Determinants and implications. J.
Med. Syst. 33 (3):181–188, 2009.