行政院國家科學委員會專題研究計畫 成果報告
探討不同吸入性麻醉劑於重新灌流局部腦缺血時於大白鼠
之影響
計畫類別: 個別型計畫 計畫編號: NSC91-2314-B-006-091- 執行期間: 91 年 08 月 01 日至 92 年 12 月 31 日 執行單位: 國立成功大學醫學系麻醉科 計畫主持人: 陳宗鷹 計畫參與人員: 籃國懋; 蔡東穎; 李佳穎; 蘇芳儀; 吳天赏;教授 報告類型: 精簡報告 處理方式: 本計畫可公開查詢中 華 民 國 93 年 2 月 3 日
政院國家科學委員會補助專題研究計畫成果報告
※※※※※※※※※※※※※※※※※※※※※※※※※
Effects of different inhalation anesthetics halothane,
isoflurane, and sevoflurane on the reperfusion focal
cerebral ischemia in rats.
※※※※※※※※※※※※※※※※※※※※※※※※※※ 計畫類別:▓個別型計畫 □整合型計畫 計畫編號:NSC 91-2314-B006-091 執行期間:91 年 08 月 01 日至 92 年 12 月 31 日 計畫主持人:陳 宗 鷹 醫師 共同主持人:李 宜 堅 醫師 計畫參與人員:籃 國 懋; 蔡 東 穎 李佳穎 蘇芳儀 吳天赏教授 本成果報告包括以下應繳交之附件: □赴國外出差或研習心得報告一份 □赴大陸地區出差或研習心得報告一份 □出席國際學術會議發表之論文一份 □國際合作研究計畫國外研究報告書一份 執行單位:國立成功大學醫學院醫學系麻醉學科 中 華 民 國 93 年 01 月 10 日
Effects of Different Inhalation Anesthetics Halothane, Isoflurane,
and Sevoflurane on the Reperfusion Focal Cerebral Ischemia in
Rats.
Tsung-Ying Chen1, M.D.; E.-Jian Lee1, M.D.; Chia-Chih Tseng1, M.D.; Fang-Yi Su, Tian-Shung Wu2, Ph.D.
1
Anesthesiology & Neurosurgery, National Chung-Kung University Medical Center and Medical School, Tainan, Taiwan. 2Institute of Chemistry, National Cheng Kung University, Tainan, Taiwan.
Introduction:
It has been postulated that inhalation anesthetics isoflurane that reduces cerebral
metabolic rate will protect the brain against ischemia.1 Warner et al. demonstrated that
halothane and sevoflurane both substantially reduce the focal ischemic brain damage in
the rat.2, 3。Masahiko et al. showed that isoflurane delays but does not prevent cerebral
infarction in rats subjected to focal ischemia4。Their results showed that isoflurane
reduced the extent of infarction accessed 2 days after focal ischemia in rat. At 14 days,
however, only selective neuronal necrosis, but not infarction was reduced by isoflurane.
In these studies volatile anesthetic-mediated neuroprotection was shown after a survival
period of 16 h to 7 days after ischemia.
There are also many literatures described about the neuroprotection of the volatile
neuroanesthesia. But it is still controversial. 5-8 The neuroprotection of the different
inhalation anesthetics are s still not compared. From our previous studies, we try to
evaluate the neuroprotective effects of different inhalation anesthetics on the focal
permanent cerebral ischemia.
Methods and Materials:
The experimental protocol was approved by the National Cheng Kung University
Animal Care and Use Committee. Male Sprague-Dawley rats, weighing 200-260 g, were
supplied by the University laboratory Animal Center, and were allowed free access to
food and water before and after surgery. Animals were anesthetized with different
inhalation anesthetics in enriched oxygen. During surgery, body temperature was
maintained at 37 ± 0.5ºC using a heating lamp. The right femoral artery was cannulated
for measuring arterial blood gases, glucose, hematocrit and blood pressure.
Cortical perfusion was measured by using laser Doppler flowmetry (LDF) (Model
DRT4; Moor Instruments Ltd., Devon, UK). The skull was thinned with a high-speed
drill over the right parietal cortex (coordinates: 2 mm posterior and 6 mm lateral to the
bregma) for placement of the LDF probe. To allow continuous monitoring of LDF, the
headpiece of a specially designed cradle was modified to allow for free rotation around
the longitudinal axis of the rat and was equipped with a snout mask for spontaneous
area devoid of large cortical blood vessels, and its position was not changed throughout
the experiment. The LDF signal was allowed to stabilize over a 30-min period before
baseline measurements were recorded.
Permanent focal ischemia was produced by middle cerebral artery occlusion (MCAO)
by using an intraluminal suture technique. Briefly, the right common carotid artery was
exposed through a lateral incision, and the external carotid artery was ligated. The
internal carotid artery (ICA) was separated from the vagus nerve. Ischemia was produced
by advancing a 4-O monofilament nylon suture, with its distal tip rounded by application
of heat, into the ICA through a puncture in the common carotid artery until the LDF
signal displayed a significant reduction. After placement, the intraluminal suture was
secured with a 4-O silk suture tied around the ICA. From the previous literature, we
demonstrated that a reduction to < 40% of the baseline LDF signal is critical in producing
consistent infarction volume in our model of MCAO.9-11 Rats that did not demonstrate
reduction of the LDF signal to <40% of the baseline was excluded from the study. LDF
measurements were recorded at immediate occlusion, 15 min and 30 min. After 30 min
stable, the rat was leave the filament and closed the would. The femoral artery catheter
was removed and let the animal recovery.
All rats received a single inhalation anesthetics: in group A, Halothane, n=11; in group
procedure. Sacrifice was performed 22-24 h after permanent MCA occlusion by
decapitation. The brain was then rapidly removed, cut into 2 mm coronal sections using a
rat brain matrix (RBM 2000C, ASI Instrument, Inc., Warren, MI) and stained according
to the standard 2, 3, 5-triphenyltetrazolium chloride (TTC) method. The infarction
volumes were determined by a quantitative image analysis of TTC stained brain sections.
Results:
Mean arterial blood pressure, partial carbon dioxide (PaCO2) and oxygen (PaO2), pH
and hematocrit were within normal physiological ranges in all animals at baseline and
during MCAO. (Table 1) Cerebral perfusion, as determined by LDF signal, was not
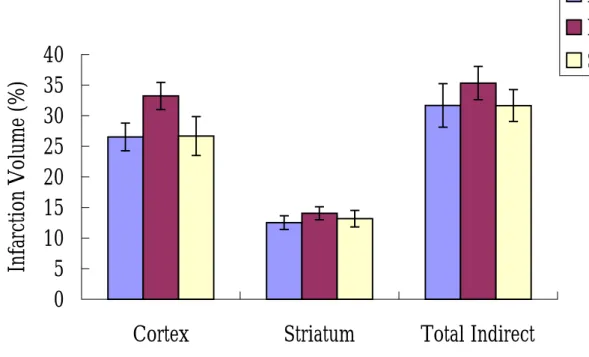
different in various treatment groups (Table 1). In experiments, the infarct volume was
not significant among three different anesthetics groups.
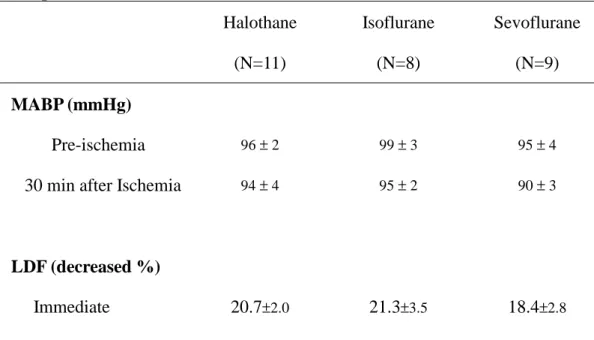
Table 1. Physiological variables at baseline (pre-ischemia), 30 min after ischemia in the experiment Halothane (N=11) Isoflurane (N=8) Sevoflurane (N=9) MABP (mmHg) Pre-ischemia 96 ± 2 99 ± 3 95 ± 4 30 min after Ischemia 94 ± 4 95 ± 2 90 ± 3
LDF (decreased %)
-ischemia
30 min after Ischemia 29.6±2.2 31.3±1.8 35.1±2.0
PH
Pre-ischemia 7.30 ± 0.02 7.39±0.01 7.39 ± 0.03 30 min after Ischemia 7.26 ± 0.03 7.35±0.01 7.28 ± 0.04
PaCO2 (mmHg)
Pre-ischemia 56.2 ± 2.4 44.7±1.6 45.8 ±3.3 30 min after Ischemia 61.9 ± 3.5 46.3±1.7 57.3 ± 5.3
PaO2 (mmHg)
Pre-ischemia 222±25 294±13 284 ± 19 30 min after Ischemia 228 ± 37 319±16 307± 19
Hct(%)
Pre-ischemia 37 ± 1 45±9 33 ±2
30 min after Ischemia 37 ± 1 37±1 32 ±1
Values are presented as mean ± SEM
0
5
10
15
20
25
30
35
40
Cortex
Striatum
Total Indirect
Infa
rc
tion V
olume
(%
)
Hal
Iso
Sevo
Figure 1. Treatment with different inhalation anesthetics during middle cerebral artery
(MCA) occlusion
Conclusion:
Present study demonstrated that used different inhalation anesthetics might not provide
significant difference neuroprotection during permanent MCAO procedure. However, we
cannot show inhalation anesthetics can provide neuroprotection or not in this experiment.
If we want to show more evidence of the inhalation anesthetics have the neuroprotection
and different anesthetics have different effects, we need to do more experiments such as
reperfusion injury.
Acknowledgments:
This research was supported by grants from the National Science Council of Taiwan
(91-2314-B-006-091).
References:
1. Newberg LA, Milde JH, Michenfelder JD. The cerebral metabolic effects of isoflurane at and above concentrations that suppress cortical electrical activity. Anesthesiology 59: 23-8, 1983.
2. Warner DS, McFarlane C, Todd MM, Ludwing P, McAllister AM: Sevoflurane and halthane reduce focal ischemic brain damage in the rat: Possible influence on thermoregulation. Anesthesiology 79: 985-92, 1993.
3. Baughman VL, Hoffman WE, Milettich DJ, Albrecht RF, and Thomas C: Neuroolgic oucome in rats following incomplete cerebral ischemia during halthane, isoflurane or N2O. Anesthesiology 69: 192-8, 1988.
4. Baughman VL, Hoffman WE, Thomas C, Milettich DJ, and Albrecht RF: Comparsion of methohexital and isoflurane on neurologic outcome and histopothology following incomplete ischemia in rats. Anesthesiology 72: 85-94, 1990.
5. Miura Y, Grocott HP, Bart RD, Pearlstein RD, Dexter F, Warner DS: Different effects of anesthetic agents on outcome form near-complete but not incomplete global ischemia in the rat. Anesthesiology 89: 391-400, 1998.
6. Warner DS, Deshpandle JK, Weiloch T. The effect of isoflurane on neuronal necronal necrosis following near-complete forebrain ischemia in the rat. Anesthesiology 64: 19-23, 1986.
7. Nehls DG, Todd MM, Drummond JC, et al. Acomparsion of the cerebral protective effects of isoflurane and barbiturates during ischemia in primates. Anesthesiology 66: 453-64, 1987.
8. John RA, Moscicki JC, DiFazioCA. Nitric oxide synthase inhibitor
dose-dependently and reversibly reduces the threshold for halothane anesthesia. Anesthesiology 1992; 77: 779-784.
9. TY Chen, EJ Lee, CC Tseng, AK Lan, JT Cheng, CL Chang: Nitric oxide Scavenger reduces Infarction Volume of Permanent Middle Cerebral artery occlusion modle in Rat and Mice. 2001 Scientific Meeting of Anesthesiology Annual Congress SAROC. Acta Anaesthesiologica. Sin. No. 3 (S) 39: F2, September 2001.
10. TY Chen, EJ Lee, CC Tseng, HY Chen, and TS Wu: Delayed treatment with carboxy-PTIO reduced brain infarction in permanent focal cerebral ischemia in mice. Anesthesiology; 96: A801, 2002
11. E-Jian Lee, Tian-Shung Wu, Ming-Yang Lee, Tsung-Ying Chen, Yi-Yin Tsai, Jih-Ing Chuang and Guan-Liang Chang. Delayed treatment with melatonin enhances electrophysiological recovery following transient focal cerebral ischemia in rats. J Pineal Res. 2004; 36:33-42..