行政院國家科學委員會專題研究計畫 期中進度報告
拇指在施行後前向滑動治療技術時關節受力狀況之生物力 學分析(1/2)
計畫類別: 個別型計畫
計畫編號: NSC93-2320-B-006-063-
執行期間: 93 年 08 月 01 日至 94 年 07 月 31 日 執行單位: 國立成功大學物理治療學系
計畫主持人: 徐阿田
共同主持人: 蘇芳慶,張冠諒,張志涵,官大紳
報告類型: 精簡報告
處理方式: 本計畫可公開查詢
中 華 民 國 94 年 5 月 31 日
行政院國家科學委員會補助專題研究計畫 □ 成 果 報 告
■期中進度報告
拇指在施行後前向滑動治療技術時關節受力之生物力學分析
In Vivo and In Vitro Biomechanical Analyses of the Thumb while Performing Postero-Anterior Glide Techniques
計畫類別:█ 個別型計畫 □ 整合型計畫 計畫編號:NSC 93-2320-B-006-063-
執行期間: 93 年 8 月 1 日至 95 年 7 月 31 日
計畫主持人:徐阿田
共同主持人:蘇芳慶 官大紳 張冠諒 張志涵 計畫參與人員: 胡孟慈 林世偉 張茹茵
成果報告類型(依經費核定清單規定繳交):█精簡報告 □完整報告
本成果報告包括以下應繳交之附件:
□赴國外出差或研習心得報告一份
□赴大陸地區出差或研習心得報告一份
□出席國際學術會議心得報告及發表之論文各一份
□國際合作研究計畫國外研究報告書一份
處理方式:除產學合作研究計畫、提升產業技術及人才培育研究計畫、
列管計畫及下列情形者外,得立即公開查詢
□涉及專利或其他智慧財產權,□一年□二年後可公開查詢
執行單位:國立成功大學物理治療學系
中 華 民 國 94 年 5 月
I
ABSTRACT
Background and Purpose: Pain in the joints of the thumb is one of the major occupation-
related disorders for orthopaedic physical therapists. Extensive manual tasks involved in their daily activity menu appear to be the major culprits, among them are the anteroposterior (PA) glide techniques. Different PA glide techniques are commonly employed by manual therapists in the clinics. However, several PA techniques are used clinically and their differential effects on the kinematics, kinetics of the thumb and the EMG activities of the related muscles have not yet been studied. The purpose of this study is to investigate the variability of 3 forms PA glide techniques, in a simulated setting, through kinematical, kinetic and electromyographic analyses in subjects who are novice to the techniques of manual therapy and those who are experienced.Part I: Surface EMG and Joint Kinematic Study
Methods: Fifteen novice subjects (4 males and 11 females, mean aged 21.9±2.2 yrs) with no
clinical experience and fifteen clinical physical therapists (5 males and 10 females, mean aged 28.0±2.1 yrs) who had no pain or disorder involving the use of thumb in the past years participated in this study. Each subject performed three different PA glide techniques (PA glide with the thumb unsupported, PA glide with digital support and the PA glide with IP supported by the index) on a force plate while interphalangeal (IP), metacarpophalangeal (MCP) and carpometacarpal (CMC) joints kinematics were tracked by a motion analysis system. The joint angles, maximum thumb-tip force, surface EMG activities of 8 thumb muscles and the Beighton score of each subject were recorded for analyses.Results: The MCP angle was negatively correlated with the IP angle (p<.05) except PA glide with
IP support in experienced group and such trend was also found between MCP angle and CMC angle. There was a negative correlation between the Beighton score and the maximum thumb-tip force (p<.01). The thumb-tip force and EMG activity of the first dorsal interosseous muscle during PA glide with IP support were greater than those of the other two techniques (p<.05).EMG activities of the extensor pollicis longus, abductor pollicis longus and extensor pollicis brevis were greater during the unsupported PA glide (p=.017).
Conclusions: The results of the present study revealed a relationship reverse in direction between
IP and MCP joint angles and between MCP and CMC. However, no such correlation exits between CMC and IP or MCP joint. Subjects with more rigid thumbs (smaller Beighton score) or using IP support are capable of exerting greater thumb-tip force. Experienced group exhibited less EMG activities and, thus, more efficiency comparing with their novice counterparts in maintaining the stability of the thumb joints.Clinical Relevance: Physical therapists with excessive thumb flexibility are advised to perform
the PA glide with IP joint supported to protect the thumb joints from injury.Part II: Intramuscular EMG and Kinetic Analysis of the Thumb
The instrumentation for the fine wire EMG has been assembled and is currently undergoing hardware and software testing. The procedures of wire electrode manufacturing and sterilization have work out and expected to finish this part of the study in June 2005.
Key Words: Thumb, Manipulation, Flexibility, Thumb tip force, Electromyography
II
中文摘要
背景與實驗目的: 對骨科物理治療師而言,大拇指關節疼痛是常見職業傷害之一。而引起 傷害牽涉到治療師常用的徒手治療手法,特別是後前向滑動徒手技巧。不同的手法經常被 治療師運用在臨床的工作上,然而,到目前為止,尚未有人針對物理治療師這個族群去探 討其使用不同手法的後前向徒手治療技巧時,對大拇指所造成的影響。所以,本篇研究主 要想針對沒有經驗及有臨床經驗的治療師,探討大拇指在不同柔軟度及不同的治療手法的 動力學及肌電學的影響。
實驗一 表面 EMG 與拇指運動學之研究
實驗方法: 15 位(4 男 11 女,平均年齡 21.9±2.2 歲)尚未有臨床經驗的初學者; 15 位(5 男 10 女,平均年齡 28.0±2.1 歲)至少 3 年骨科臨床經驗的物理治療師,這些受試者使用大拇指不 能有疼痛的情形。每位受試者在六軸力版上表現 3 種不同的後前向滑動徒手技巧(不支撐後 前向滑動,四根手指支撐之後前向滑動,大拇指指間關節支撐之後前向滑動),藉由動作分 析系統同步收取 IP 關節、MCP 關節及 CMC 關節動力學資料,每個大拇指關節角度、指尖 的力量、8 塊大姆指肌肉的表面肌電圖以及每位受試者的柔軟度分數。
結果: 除了有經驗受試者在指間關節支撐之後前向滑動技巧以外,MCP 與 IP 角度之間都呈 現負相關的情形(p< .05),而在 MCP 和 CMC 之間也有呈現相同的趨勢。至於柔軟度與產生 的最大指尖力量也是負相關的結果。指尖最大力量、1stDI 的肌電圖活動,都顯示在表現指 間關節支撐之後前向滑動技巧時有顯著較大的力量(p< .05)與肌電活動(p< .017)。而 EPL, APL 及 EPB 則顯示在表現不支撐後前向滑動技巧時有較大的肌電圖活動(p< .017)。
結論: 結果顯示在 IP 及 MCP 之間與 MCP 及 CMC 之間都呈現負相關的趨勢,也就是當 IP 處在比較伸直的姿勢時,MCP 就會呈現彎曲的姿勢,而 CMC 會表現伸直的趨勢。柔軟度 較小的受試者或是使用指間關節支撐之後前向滑動技巧都能夠產生較大的力量。至於有經 驗的族群比初學者更能有效率的使用肌肉活動來維持大拇指關節的穩定度。
臨床意義: 初學者或是關節柔軟度較大的治療師建議使用指間關節支撐之後前向滑動技巧 來減少徒手治療所造成的職業傷害。
實驗二 Fine-Wire EMG 與拇指動力學之研究
此部份之研究儀器(Fine Wire EMG 系統已招標組裝完成,目前正進行硬體與軟體測試,預 計六月底可完成實驗。
關鍵詞: 拇指、操作治療、柔軟度、拇指尖應力、肌電圖
III
目錄
ABSTRACT --- I
中文摘要 ---II
目錄 --- III
INTRODUCTION --- 1
PURPOSE --- 1
LITERATURE REVIEW --- 2
METHODS --- 3
RESULTS --- 6
DISCUSSIONS --- 10
CONCLUSSION --- 12
REFERENCE --- 12
1
INTRODUCTION
One of the most common musculoskeletal complains in physical therapists is the pain over the basal joint of the thumb especially when performing the palpatory and manipulative procedures. Certain techniques drastically increase the long axis compression force along the longitudinal axis of the first ray. If there is insufficient ligamentous or musculotendinous support to withstand the external force, injury thumb may occur.
As a profession dependent upon manual work, physical therapists are susceptible to a variety of occupational musculoskeletal injuries. Bork et al.1 reported that pain in the wrist and hands among therapist is common with a prevalence rating of 29.6%, second only to low back pain (45%) from a sample of 928 respondents.
PURPOSE
Physical therapists are prone to thumb injuries especially when extensive manual techniques are involved as part of their daily menu of therapeutic activities in the clinics. There was no study had ever reported the kinematics of the thumb and the electromyographic responses of extrinsic and intrinsic muscles of the thumb while physical therapists were performing these incriminating manual therapy techniques or similar tasks. Experienced therapists usually employ alternative techniques to protect their thumbs from injury or to alleviate pain for the symptomatic thumbs. It is necessary to investigate these alternative techniques biomechanically for the ultimate benefit of this profession. We also felt that it is necessary to study the movement and EMG patterns between groups of subjects who are novice to or experienced in the techniques involved as the latter group might have developed different strategies and movement patterns due to extensive training or clinical practice. Finally, physical characteristics of an individual may affect his/her ability to exert force through the thumb tip. For these individuals alternative techniques may need to be learned and practiced from the beginning of his/her apprenticeship. Therefore, the purpose of this study was to investigate the differences in the kinematic responses of the thumb and the EMG activities of the related muscles while performing three different unilateral PA glide techniques in a group of novice and comparing to another group of seasoned physical therapists.
The ultimate goal was to seek a less stressful technique to prevent possible job related disorders of the thumb among orthopedic physical therapists.
LITURATURE REVIEW
Cromie et al.2 have showed that 33.6% of manual therapists who complained of thumb pain lasting more than three days. This study also established a definite relationship between the use of manipulative techniques and the prevalence of thumb pain.2, 3 To prevent of thumb injury for physical therapists is one of the important parts. The most common sites of thumb pain for manual therapists were the metacarpophalangeal joint (MCP) and carpometacarpal joint (CMC)
2
of the thumb with the highest prevalence (84%) occurred in the latter. Early stage degeneration of the CMC was common among these therapists and pain was aggravated by increasing daily activities. The techniques most commonly associated with the thumb pain were the unilateral (87%) and central (85%) posteroanterior (P-A) glides.3
Therapists with manipulation related thumb pain usually exhibit progressive capsular laxity and hypermobility at the joints of the thumb. Laxity and hypermobility predisposes the joint to vicious cycles of acute and chronic synovitis and further hypermobility. 4 Several studies have investigated the association between joint hypermobility and the occurrence osteoarthritis of the basal joint of the thumb5 and between hypermobility and musculoligamentous lesions.6 Jonsson et al.5investigated the association of clinical hand osteoarthritis with hypermobility according to fifteen female subjects. The prevalence of hypermobility was high in the patients with predominant 1st CMC osteoarthritis. Diaz et al.6 also studied the association between degree of joint laxity and occurrence of musculoligamentous lesions with 675 male subjects in 2 months.
The results suggest that the subject with joint hyperlaxity is more frequently prone to musculoskeletal lesions.
In case of serious chronic MCP instability, a patient usually compensates by fixing the MCP in hyperextended position4 and uses the active stabilizer (intrinsic thenar muscle) to compensate for capsuloligamentous instability. Such mechanism may precipitate these muscles to become exhausted as a result of over or prolonged loading.7
During normal pinch and grasp, forces carried by the extrinsic tendon of the thumb were four to five times the applied external force and the intrinsic tendon forces were one and half to three times as much.8 The largest joint contact force was found at CMC and decreased progressively in a proximal to distal direction as the number of muscles acting on the more distal joints decreases.8
As mentioned above, tendon force and contact force would increase the stress of the thumb joints during functional pinch or grasp tasks. Moulton et al.9 found that the magnitude of the CMC stress was dependent upon the position of MCP. Fixing the MCP in a flexed position would effectively unload the most palmar contact force of CMC even with the presence of arthritic disease.
Recently, video-based 3-D motion analysis system have been used for measuring kinematics of the thumb and digits10, 11 for determining the segmental centers of the rotation of digits 12, and evaluating finger movement loss 13, 14, or measuring the initiation, sequence and the maximal scope of digital joint motion.15-17 Chiu et al.13 evaluated the range of motion of thirty-three fingers (from twelve patients) with various injuries by goniometry and motion analysis system.
The authors reported that some cases compensated for a stiff distal joint by a proximal joint hypermobility during motion and was difficult to reveal by goniometry alone.
Several studies investigated the thumb electromyographically while performing functional tasks such as pinch and grasp. Johanson et al.18 reported that ADP and EPL were activated in unstable pinch tasks such as key and opposition pinch.Maier et al. 19 studied the contribution of 15 finger muscles to isometric force in precision grip and suggested that the intrinsic muscle is more important in the production of lower level isometric force in grip task. The EMG activities
3
of thumb muscles were also used to quantify the production of force in different directions of thumb movements while performing pinch and grasp.18, 19, 22
PART I. SURFACE EMG AND JOINT KINEMATIC AND KINETIC STUDY METHODS
Subjects
15 subjects novice to manual therapy (Group I, the Novice Group) and 15 therapists with at least 3 years experience, primarily in orthopedic settings, (Group II, the Experienced Group) were recruited for this study.
Group I included 11 female and 4 male subjects without clinical experience in manual therapy were recruited for this study. Group II included 10 female and 5 male healthy subjects with clinical orthopaedic experience at least 3 years. Those subjects who had any history of musculoskeletal, neurological disorders, or pain involving the use of thumb in the past years were excluded from this study. There was no difference in basic demographic data between Group I and Group II except age and clinical manual experience (Table 1).
Table 1 Description of the participants of both groups
Basic data
Group I (n=15) Mean (SD)
Group II (n=15) Mean (SD)
Age (years) 21.9 (2.2) 28.0 (2.1)
Gender (male / female) 4 / 11 5 / 10
Height (cm) 165.7 (6.0) 162.9 (8.0)
Weight (kg) 56.9 (8.4) 56.9 (12.1)
BMI (kg/m2) 20.6 (2.0) 21.3 (3.3)
Clinical experience (years) 0.0 (0.0) 4.3 (1.4)
*Group I: Novice Group; Group II: Experienced Group
Instruments and Procedures
Each subject read and signed an informed consent form and answered a questionnaire concerning history of the thumb pain before testing. The results of the mobility assessment (flexion, extension, abduction and adduction) and the length of proximal phalanx, distal phalanx and metacarpal bone of the thumb of each subject were recorded by using hand goniometer20 and a measuring tape. Beighton score was obtained from each subject. The Beighton criteria21 includes: (1) passive dorsiflexion of the fifth finger≧ 90°; (2) passive apposition of thumb to forearm; (3) hyperextension of elbows≧ 10°; (4) hyperextension of knees≧ 10°; (5) resting palms on the floor in forward flexion with straight knees. The numerical scores for item (1) to (4) are scored bilaterally with a possible highest score of 9.
Each retro-reflective marker cluster consisted of a T shaped plastic plate with 3 makers was
4
fixed on each thumb segment. Markers were also placed on the medial and lateral aspect of the IP and MCP joints to define the centers of the IP and MCP joints. The hand was then placed on a rigid splint to maintain the wrist and the hand in a fixed position for the recording of the resting position of the thumb. Small arc movements of thumb (adduction-abduction–flexion -extension-circumduction) were also recorded with VICON motion analysis system while holding in this position. (Fig. 2)
Figure 2 Hand was placed on a rigid splint to record the resting position of the thumb.
Surface EMG electrodes were then placed over the muscle bellies extensor pollicis longus (EPL), abductor pollicis longus (APL), extensor pollicis brevis (EPB), abductor pollicis brevis (APB), flexor pollicis brevis (FPB), adductor pollicis (ADP), flexor pollicis longus (FPL) and the 1st dorsal interosseus (1st DI) muscle bellies (Fig. 3). The muscle locations were identified by palpation and monitored the EMG activities associated with the specific movement of the muscle.
Figure 3 EMG electrodes were placed over the EPL, APL, EPB, APB, FPB, ADP, FPL and 1stDI.
The maximal EMG signal of each thumb muscle was recorded with a maximal voluntary contraction of each muscle. The following PA glide techniques were tested in a random order on the 6-axis load cell on a table while the VICON system tracks the trajectory of thumb movement.
(Fig. 4)
1. Unsupported PA glide (T1): The P-A glide of thumb is performed with the rest of digits unsupported.
5
2. PA glide with digits support (T2): The P-A glide of the thumb is performed the rest of digits supported on the table.
3. PA glide with palmar supported at the interphalangeal joint of thumb (T3).
Figure 4 PA glide techniques were performed on a load cell on the table. (From left to right were the techniques of unsupported PA glide (T1), PA glide with digits support (T2) and PA glide with IP supported by index finger (T3))
A LABVIEW program was written to calibrate the 6-axis load cell and display force levels from 0% to 100% with 25% increments. The subjects were asked to exert a maximum force on the force plate while performing PA glide technique recorded force was set as 100%. The subjects were then instructed to exert at the force level matching each of the target force level displayed on the monitor as close as possible for five seconds. The EMG signals, the trajectory of each marker and the thumb-tip force responses were recorded simultaneously. At the end of the test, the maximum voluntary contraction EMG of each muscle was recorded one more time to verify the stability of the EMG recordings.
6
PRELIMINAY RESULTS
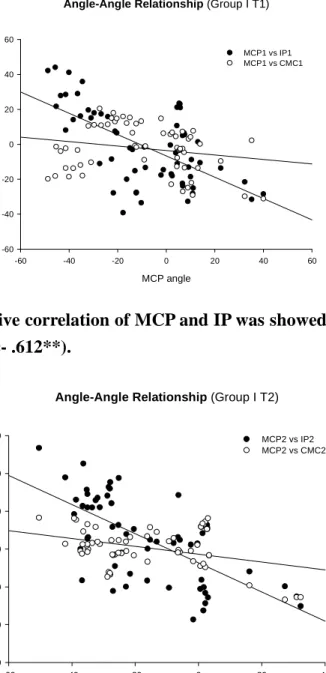
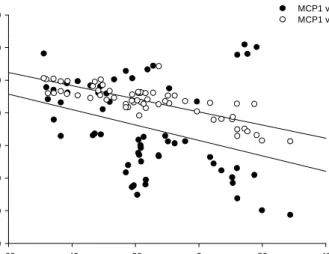
In Group I, IP and CMC joint angles were negatively correlated to the thumb-tip force (p< .05). In the other words, the more thumb-tip force, the more extension exhibited in the IP and CMC joints. MCP joint angles were negatively correlated with the IP joint angles in all three techniques (r = -.612, r = -.663, r = -.465, p< .01, respectively) and such negative linear correlation was also observed between CMC and MCP joint angle during T2 (r =-.378, p< .01).
(Fig. 5-7)
Angle-Angle Relationship (Group I T1)
MCP angle
-60 -40 -20 0 20 40 60
IP & CMC angle
-60 -40 -20 0 20 40 60
MCP1 vs IP1 MCP1 vs CMC1
Figure 5 Linear negative correlation of MCP and IP was showed during unsupported PA glide in novice group (r =- .612**).
Angle-Angle Relationship (Group I T2)
MCP angle
-60 -40 -20 0 20 40
IP & CMC angle
-60 -40 -20 0 20 40
60 MCP2 vs IP2
MCP2 vs CMC2
Figure 6 Linear negative correlation of MCP and IP was showed (r =- .663**). Such
correlation was also showed between MCP and CMC during PA glide with digits support in
novice group (r =- .378**)
7
Angle-Angle Relationship (Group I T3)
MCP angle
-40 -20 0 20 40 60
IP & CMC angle
-60 -40 -20 0 20
40 MCP3 vs IP3
MCP3 vs CMC3
Figure 7 Linear negative correlation of MCP and IP was showed during PA glide with IP supported by index in novice group (r =- .465**).
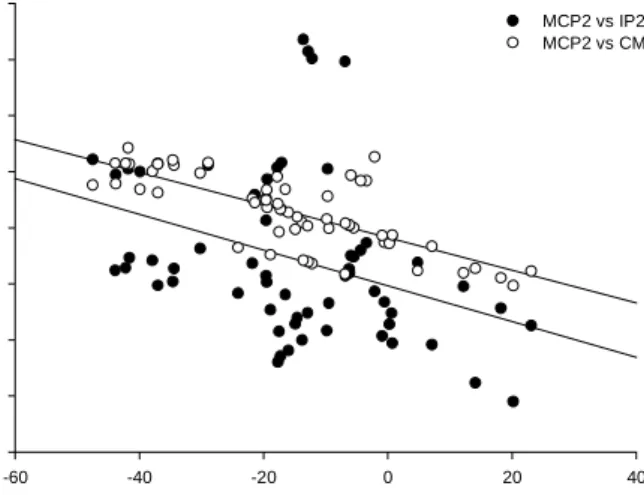
In Group II, there was a negative correlation between IP joint angle and thumb-tip force during T2 (r =-.256, p< .05). The more force generated by the thumb, the more extension of IP joint was observed during T2. Figure 8-10 showed significantly negative correlation between IP and MCP joints except T3. Such negative correlation was also revealed between MCP and CMC joint in all three techniques (p< .05) at all force levels.
Angle-Angle Relationship (Group II T1)
MCP angle
-60 -40 -20 0 20 40
IP & CMC angle
-80 -60 -40 -20 0 20 40
60 MCP1 vs IP1
MCP1 vs CMC
Figure 8 There were negative correlations between IP and MCP joint angles (r = - .339**)
and between MCP and CMC joint angles (r = - .809**) during unsupported PA glide in
experienced group.
8
Angle-Angle Relationship (Group II T2)
MCP angle
-60 -40 -20 0 20 40
IP& CMC angle
-80 -60 -40 -20 0 20 40 60 80
MCP2 vs IP2 MCP2 vs CMC2
Figure 9 There were negative correlations between IP and MCP joint angles (r = - .368**) and between MCP and CMC joint angles (r = - .746**) during PA glide with digits support in experienced group.
Angle-Angle Relationship (Group II T3)
MCP angle
-40 -30 -20 -10 0 10 20 30 40
IP &CMC angle
-80 -60 -40 -20 0 20 40
60 MCP3 vs IP3
MCP3 vs CMC3
Figure 10 There were correlations between IP and MCP joint angles (r = .269*) and negative correlation between MCP and CMC joint angles (r = - .636**) during T3 in experienced group.
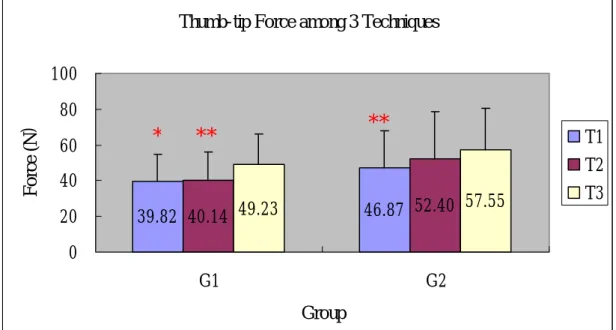
In Group I, the average thumb-tip force produced while performing T3 was greater than those of the T1 (z = -2.542, p = .011) and the T2 (z = -2.726, p = .006). However, there was no difference in the magnitude of the force produced by the T1 and T2 (Fig. 11). A negative correlation (p< .01) was found between the thumb-tip forces and the flexibility (Beighton scores) of the individuals in all three techniques in Group I (Table 2).
In Group II, the force generated by T3 was greater than by T1 (Fig. 16). Table 2 showed the relationship between thumb-tip force and general flexibility. There were negative correlation between thumb-tip force and Beighton score but only T1 reached significant difference (p= .022).
9
Thumb-tip Force among 3 Techniques
39.82 40.14 49.23 46.87 52.40 57.55 0
20 40 60 80 100
G1 G2
Group
For ce ( N )
T1 T2 T3
Figure 11 Thumb-tip forces between three techniques. (T1: unsupported PA glide; T2:
PA glide with digits supported; T3: PA glide with IP supported by index finger; G1: novice group; G2: experienced group) There was significant difference between T3 and T1 and between T3 and T2 in G1. There was also significant difference between T3 and T1 in G2 (*p< .05; **p< .01).
Table 2 Correlation of thumb-tip force and Beighton score
Group I Group II
Technique Spearman’s
Correlation
Spearman’s Correlation
Unsupported PA glide (T1)
- 0.761** -0.585*PA glide with digits supported
(T2)
- 0.747** -0.324PA glide with IP joint supported
by index (T3)
- 0.694** -0.442*p< .05; **p< .01;
Group I: novice group (N=15);
Group II: Experienced group (N=15)
The mean value of the 1stDI showed the smallest in both groups. Between two groups, there were significant differences in all muscles except ADP and 1stDI (p< .05).
Among three techniques, there was difference in EMG activities. ADP activities were larger during T3 than the other two techniques. EPB and EPL showed more activities during T1 than the other two techniques. APL also revealed more activities during T1 than T3. 1stDI showed obvious difference among three techniques (T3>T1, T3>T2, T2>T1, p< .017).
Among four force levels, all thumb muscles showed difference between any two force levels.
* ** **
10
These muscles revealed linear correlated to the different force level. When the thumb-tip forces were normalized by individual body weight the EMG of Group I subjects showed increases with thumb-tip force in all techniques except 1stDI in T1 and T2 for all muscles tested. Group II showed linear correlations between EMG and the thumb-tip force except 1stDI in T1 and T2, EPB in three techniques and APL in T2.
DISCUSSION
In the novice group, the angle of the MCP joint was highly correlated with that of the IP joint in the three techniques. Such angle-angle relationships could be explained by the
compensated movements occurring in the joints of the thumb. When a tip force is exerted through the thumb, the orientation of the reaction force and the initial position of the IP joint determine the behavior of the rest of the MCP and CMC joint. When IP is in extended position or is being pushed into extension by the reaction force, the MCP joint will be forced into flexion and the CMC joint into extension. When IP is in flexed position or being pushed into flexion by the reaction force, the reverse will be true. A relationship was also found in the experienced group between the MCP and CMC joint and between IP and MCP except that correlation between IP and MCP joints during PA glide with IP support (T3) was a positive one. In this case the angle of IP joint was greater in experienced group than in novice group. When the IP joint is fixed in a greater extension position, it will carry both IP and MCP joint into more extended positions. But the correlation between IP and MCP in experienced group will be negative while excluding the extreme range data.
In this study, IP and CMC joint angles were increasing with the magnitude of thumb tip force in novice group; but no such correlation was found in experienced group. It seems the experienced physical therapists adopted a quite different strategy in dealing with the increasing thumb tip force.
The thumb provided greater forces in PA glide with IP support position (T3). In this position, the IP joint is prevented into further extension by the counter force provided by the index finger, thus, with a greater stability for force transmission through the first ray. The stabilities of the IP, MCP and CMC joints are essential for generating greater isometric force.
The Beighton Score indicates the general flexibility of an individual. In novice group, the smaller the Beighton Score, the greater forces were transmitted through the thumb tip irrespective of stable or unstable tasks.
Novice subjects increase the joint angles in responding to increasing tip force and they also relied more on muscles for joint stability and support than the experienced subjects in all three techniques. As the joint reaction force derives primarily from the muscles crossing the joint such response will inevitably increase the reaction force, a situation that is detrimental to the health of the joint involved. The experienced physical therapists, however, were more capable of
maintaining a more constant and stable joint position and did not rely on muscles as much for
11
effective transmission of forces through the thumb as their novice counterpart. And, through adaptation, the experienced therapists were able to exert tip forces irrespective of their Beighton scores in the relatively stable tasks (T2 and T3).
The mean values of each muscle activity during three techniques in experienced group were lower than those of the non-experienced group except ADP and 1stDI. The results indicated that the experienced physical therapists perform these three PA glide techniques with greater
efficiency than the non-experienced subjects.
Johanson et al. 18 reports that in all unstable pinch or grasp conditions, APB and EPL were at a higher activation level to direct thumb-tip force accurately. Weathersby et al. 22 had also reported that the timing of EPB was similar to APL to support as a stabilizer.In this study, T1 is an unstable task compared with the other two techniques. Our results showed greater EPL, EPB and APL activation during T1 technique than the other two techniques. The EPL muscle functions as the extensor of IP and MCP joint and rotates the first metacarpal laterally, adducts the thumb and assists in wrist extension and supination. 23 However, the EPB extends and abducts the CMC joint, abduct the wrist and also contributes to IP and MCP extension.23 The tasks of present study are different from the pinch or grasp tasks reported by Johanson et al. in 2001. The PA glide techniques involve not only the thumb joint stability but also the wrist position. Both EPL and EPB contribute to wrist stability while APB does not. Long et al.24 concluded that extrinsic muscle provides gross motion and intrinsic muscle assists in power compression. Cooney et al.8 also mentioned that EPL and EPB have adduction moments at the MCP joint to assist ADP in providing stability and balancing flexion force during pinch and grasp. The extensors such as EPL and EPB balance the flexion force or the inappropriately directed force in the unstable thumb and prevent it from slipping. This unstable technique increases the co-contraction of the flexors and extensors.
In this study, more APL activities were observed during T1 than T2 or T3. Brand et al.28 mentioned that role of APL was to maintain the 1st metacarpal bone against the force from adductors. APL provides dynamic CMC joint stability and also serves as wrist stabilizer with EPB.30
So during unstable task (unsupported PA glide), more activities of the APL, EPL and EPB
were present as was expected.The 1stDI originates on the radial aspect of the second metacarpal and inserts to the 1st proximal phalanx. It contributes about 93% abduction force to the index finger and provides a distally and ulnarly directed force for 1st metacarpal base. The ADP is responsible for the adduction of thumb. 25 Previous study reported that the thumb motion during closing hands, making fists and pinching tasks involved the ADP and the 1stDI muscle.26, 27 Imaeda et
al.29mentioned that the 1stDI and ADP were oriented to act across long lever arms and generate excellent strength for pinch and grasp. In addition, the ADP provides the greatest strength by combing its large effective cross-sectional muscle mass and its long lever arm at CMC joint in power, lateral and pulp pinches. In this study, the mean values of the 1stDI activity were low in T1 and T2 but the activities were different among the three techniques. Moreover, there was no correlation between increasing forces and 1stDI activities in T1 and T2 in both groups. This may be explained by the differences in the demands required of this muscle during the performance of
12
these three techniques. There is no need for 1st DI to participate in T1 as the index finger was free and is quite incapable of exerting an effective influence on the thumb. However, while
performing T2, with the index finger firmly planted on the force plate, the 1st DI is in a more stable and effective position to maintain the stability of both thumb and the index. With the index placed on the palmar aspect of the IP, T3 position allows the 1stDI a more active role in a
maintaining the IP stability in a shorter muscle length than the T2 position. In T3, the 1stDI acts synergistically with the ADP muscle in adducting the index towards the palmar aspect of the IP joint of the thumb which may explain the greater EMG activities in these two muscles than T2 and T1. Nevertheless, during functional task such as power grip, the adductor and flexor muscle groups (ADP and FPB) pull on the base of the proximal phalanx in an ulnar and ventral direction and may contribute to the dorsal and radial subluxation of the CMC joint when the 1st metacarpal was carried into more flexion and adduction. The 1stDI, on the other hand, acts against the radial subluxating force by pulling the base of the 1st metacarpal ulnarly and distally.28 ADP and 1stDI were more active during T3. It maybe decrease the subluxating force pulled from the other muscles and maintain stability of metacarpal base in this position than the other two. In our study the ADP and 1stDI also provide force to counteract tendency for extension during T3.
CONCLUSION
Experienced subjects perform manual skill more efficiency as evidenced by lower EMG activities in the thumb muscles. EMG activities of EPL, APL and EPB revealed that they are more active during unstable task such as unsupported PA glide in both groups.
The results of this study provide physical therapists the information about less stressful method for thumb joints for different PA glide skills. PA glide with IP supported by index provide more stability of the thumb for novice or therapists with greater flexibility to generate greater force more efficiently.
PART II. INTRAMUSCULAR FINE WIRE EMG AND JOINT KINETIC STUDY
Progress Report
5 subjects with no experience in manual therapy and 5 physical therapists experienced (> 5 years) in manual therapy will be recruited for fine wire EMG study.
The instrumentations used in Part II are essentially the same as was used in Part I of the study except that a fine-wire intramuscular EMG, a 12 channel Model 15 Neurodata Amplifier System (Grass – Telefactor, Astro-Med, Inc. Product Group, 570 Liberty Street, Braintree, MA USA 02185) will be used instead of the AMT-8 EMG System used for surface EMG recording.
This fine-wire EMG system has been purchased and assembled and is in the processes of been tested for use in conjunction with the VICON Motion Analysis System. The fine-wire electrodes manufacturing and sterilization protocols have been worked out and the study is expected to finish data collection phase at the end of June 2005.
13
Reference:
1. Bork BE. Cook TM. Rosecrance JC. Engelhardt KA. Thomason ME. Wauford IJ. Worley RK. Work-related musculoskeletal disorders among physical therapists. Phys Ther.
76(8):827-35, 1996
2. Cromie JE. Robertson VJ. Best MO. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys Ther. 80(4):336-51, 2000
3. Wajon A. Ada L. Prevalence of thumb pain in physical therapists practicing spinal manipulative therapy. J Hand Ther. 16(3):237-44, 2003
4. Eaton RG. Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 55(8):1655-66, 1973
5. Jonsson H. Valtysdottir ST. Kjartansson O. Brekkan A. Hypermobility associated with osteoarthritis of the thumb base: a clinical and radiological subset of hand osteoarthritis. Ann
Rheum Dis. 55(8):540-3, 1996
6.
Diaz MA, Estevez EC, Guijo PS. Joint hyperlaxity and musculoligamentous lesions: study of a population of homogeneous age, sex and physical exertion. Br of Rheumatol.28:320,1989
7. Rotella JM. Urpi J. A new method of diagnosing metacarpophalangeal instabilities of the thumb. Hand Clinics. 17(1):45-60, v-vi, 2001
8. Cooney WP III. Chao EY. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg Am. 59(1):27-36, 1977
9. Moulton MJ. Parentis MA. Kelly MJ. Jacobs C. Naidu SH. Pellegrini VD Jr. Influence of metacarpophalangeal joint position on basal joint-loading in the thumb. J Bone Joint Surg
Am. 83-A(5):709-16, 2001
10. Rash G.S., Belliappa P.P. and Wachowiak M.P. et al., A demonstration of the validity of a 3-D video motion analysis method for measuring finger flexion and extension. J Biomech.
32:1337-1341,1999
11. Kuo LC. Su FC. Chiu HY. Yu CY. Feasibility of using a video-based motion analysis system for measuring thumb kinematics. J Biomech. 35(11):1499-506, 2002
12. Zhang X. Lee SW. Braido P. Determining finger segmental centers of rotation in flexion-extension based on surface marker measurement. J Biomech. 36(8):1097-102, 2003 13. Chiu HY. Lin SC. Su FC. Wang ST. Hsu HY. The use of the motion analysis system for
evaluation of loss of movement in the finger. J Hand Surg [Br]. 25(2):195-9, 2000
14. Fowler NK. Nicol AC. Functional and biomechanical assessment of the normal and rheumatoid hand. Clin Biomech. 16(8):660-6, 2001
15. Somia N. Rash GS. Wachowiak M. Gupta A. The initiation and sequence of digital joint motion. A three-dimensional motion analysis. J Hand Surg [Br]. 23(6):792-5, 1998
16. Su FC, K.L., Chiu HY, Hsu HY., The validity of using a video-based motion analysis system for measuring maximal area of fingertip motion and angular variation. Proc Inst
Mech Eng [H] 2002; 216(4): 257-63.
17. Coert JH. van Dijke HG. Hovius SE. Snijders CJ. Meek MF. Quantifying thumb rotation during circumduction utilizing a video technique. J Orthop Res. 21(6):1151-5, 2003
14
18. Johanson ME. Valero-Cuevas FJ. Hentz VR. Activation patterns of the thumb muscles during stable and unstable pinch tasks. J Hand Surg [Am]. 26(4):698-705, 2001
19. Maier MA. Hepp-Reymond MC. EMG activation patterns during force production in precision grip. I. Contribution of 15 finger muscles to isometric force. Exp Brain Res.
103(1):108-22, 1995
20. Norkin CC and White DJ: Measurement of joint motion: A guide to goniometry, F.A. Davis company, Philadelphia.1995
21. Beighton P. Solomon L. Soskolne CL. Articular mobility in an African population. Ann
Rheumat Dis. 32(5):413-8,1973
22. Weathersby HT. Sutton LR. Krusen UL. The kinesiology of muscles of the thumb: An electromyographic study. Arch Phys Med Rehabil. 44: 321-326, 1963
23. Von Schroeder HP. Botte MJ. Anatomy and functional significance of the long extensors to the fingers and thumb. Clin Orthop. (383):74-83, 2001
24. Long C II. Conrad PW. Hall EA. Furler SL. Intrinsic-extrinsic muscle control of the hand in
power grip and precision handling: an electromyographic study. J Bone Joint Surg. 52A:853-867, 1970
25. Chao EYS. An K-N. Cooney WP. Linscheid RL. Biomechanics of the hand. World Scientific, Singapore, 1989.
26. Johanson ME. Skinner SR. Lamoreux LW. Phasic relationships of the intrinsic and extrinsic thumb musculature. Clin Orthop. (322):120-30, 1996
27. Close JR. Kidd CC. The functions of the muscles of the thumb, the index, and long fingers.
Synchronous recording of motions and action potentials of muscles. J Bone Joint Surg Am.
51(8):1601-20, 1969
28. Brand PW. and Hollister A. Clinical mechanics of the hand. 2nd ed. St. Louis. 1993
29. Imaeda T. An KN. Cooney WP 3rd. Functional anatomy and biomechanics of the thumb.
Hand Clinics. 8(1):9-15, 1992
30. Kauer JMG. Functional anatomy of the carpometacarpal joint of the thumb. Clin Orthop.