The effectiveness and barriers of implementing a workplace health promotion program to improve metabolic disorders in older workers in Taiwan
Introduction
Like many economically developed countries, Taiwan's general population and workers are ageing rapidly. Older workers usually have higher prevalence of ageing-related metabolic disorders especially abdominal obesity, hypertension, hyperglycemia and dyslipidemia. Roughly 90% of older Taiwanese have at least one metabolic disorder and 45% have metabolic syndrome (1). These disorders increase the risk for diabetes mellitus, heart disease, chronic renal
insufficiency, and some cancers, a group of lifestyle-related chronic diseases known as the non-communicable diseases (NCDs). Lifestyle factors such as improper diet, physical inactivity, cigarette-smoking and stressful life are among the major causal factors (2). Studies have shown that the risk of these metabolic disorders or NCDs can be reduced through lifestyle interventions, especially with planned strictly enforced health-promoting programs (3, 4).
In Taiwan, 93% of the enterprises (≥50 workers) and 49% of workers belong to small- and medium-scale enterprises (SMEs) with 50-500 workers (5). The proportion of workers aged over 50 years increased from 10.6% in 1997 to 17.9% in 2011 (6). Theoretically, workplace is where employees spend a considerable amount of time and hence, where there are many opportunities to enable behaviour change and could be as an ideal place to implement these programs. The workers are likely to have similar background and are more likely to have similar schedules, or even similar health issues. In addition, the workplace itself impacts on health directly, i.e. through stress, so there are opportunities to create healthy and supportive environments in the workplace. Finally, there are opportunities for key messages to be disseminated back to the families of the employees, thus achieving further reach in the intervention. Although the government has made considerable efforts to improve workplace health promotion activities in recent years, little attention has been paid to health issues specifically related to aging workers (7, 8). There were efforts to promote self-certification of healthy workplace programs, but the impact of such programs to older workers in SMEs is questionable (9).
Given that company cultural and regulatory factors can greatly influence the
implementation and effectiveness of health promotion programs, most SMEs in Taiwan lack the 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
desire or capability to carry out health promotion activities by themselves (10). Thus, workers of SMEs are often at great risk of metabolic disorders or other aging-related health conditions. Although there is a growing recognition of the importance of occupational health services (OHS) to promote workers' health across the life course (11), older workers are often the least addressed groups in OHS (9). Older workers are also more likely to have long-accustomed lifestyles that are more difficult to change (12, 13). Besides,health conditions and metabolic disorders vary considerably among individuals, we were not sure about the availability of time for the project, implementing strictly enforced programs would seem impractical or impossible. Further, decisions about adopting workplace health promotion (WHP) initiatives are likely to be associated with increasing pressure for productivity or profits.
Therefore, facing an aging workforce, health promotion measures that motivate older workers to improve lifestyle at their own time appear to be a viable and practical choice. Besides, cultural and regulations differ country to country, or even businesses business, thus, there is a need to determine the appropriate strategy for each specific condition to ascertain the
effectiveness and appropriateness of a specific health promotion strategy (14). Thus, our
objective was to conduct a study to evaluate the effectiveness and usefulness of a WHP program to reduce the risk of metabolic disorders in older workers in Taiwanese.
Methods
Workplaces and subjects
With the purpose of developing a practical model for reducing the risk of metabolic syndrome in older workers in mind, we conducted a two-arm quasi-experiment (15). We purposely made the intervention program flexible, multi-choice, individualized, non-strictly enforced, and practical. The study sites were limited to central-southern Taiwan where relatively ageing and more industries are traditional, non-technology SMEs. These traditional SMEs are generally less receptive to external changes or interventions, and have high proportions of older workers. We identified and approached six sites, two declined to participate for no occupational health nurses and one only 6% employees were grouping as ageing, three showed interest in allowing us to conduct the study. All three sites had no prior experience in carrying out WHP to reduce the risk of workers' metabolic disorders. We first explained to them about the objective and procedure of 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
this government-supported study. After getting the managers interested in the study and winning their trust, we were allowed to enter the sites, and we finally got the approval to conduct the study on their workers and their commitments of support.
The three sites had a total of 1,245 workers. Among them, 438 (35.2%) met our inclusion criteria of ≥50-year old and with full-time employment. Of the 438, 264 showed interest in participating in the study and completed a prescreening questionnaire. Of the 264, 108 agreed to participate in the study and signed the study consent. We could not get any information of those who have no interested in the study, but there are no differences between the characteristics of those did and did not take part in the project (table 1). Participants included assembly line workers, office clerks and managerial staff. Although we try to allocate on workplace, there were significant differences in the type of work and style of management among the sites, especially between factory A and factory C. Finally, those who had more flexible work schedule and were more likely to take part in the group activities were assigned to the intervention group (n=58, A=36 & C=22), others were assigned to the reference group (n=50, A=5, B=21 &C=24) (Figure 1). The number of subject per group met the number of subjects (n = 49) estimated according to Noordzij et al. (16) by assuming a mean intervention effect of a by 3.85cm (SD=6.5 cm)
decrease in waist circumference, α = 0.05, power 0.8 and 10% dropout.
Each qualified worker was interviewed, face to face, with a structured questionnaire by a trained interviewer for eliciting food intake, lifestyle, time use and stress status, and taken an over-night fasting blood specimen for determining blood biochemical indicators. These values also served as baseline data for those who participated in the study. The study protocol was approved by an institutional review board and the study was conducted according to the ethical standards set forth in the Helsinki Declaration.
Procedure
The 24-week trial period was divided into two phases. Phase I (4 weeks) emphasized on
educating the workers about healthy living especially in understanding the impact of the lifestyle on the NCDs, and the concept of managing one's own health. Participants were explained about the importance of healthy eating, routine physical activity and weight control. Each participant in the intervention group was also analyzed for unhealthy health behavior and was provided with 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
guidance to set personal goals for improving health behavior and to outline an intervention program according to their work and personal schedules. We also helped the participants (in the intervention group) to organize into groups of 5-8 persons according to their job schedules and location. Each group met biweekly to share experiences and give mutual support and
encouragements, and at the same time to cultivate leadership.
Phase II (the next 20 weeks) emphasized on cultivating team spirit, removing obstacles, reinforcing the goal or reaching higher goals. Each group was gradually transformed from workplace occupational health nurse (OHN)-led to group leader-led discussions emphasizing experience-sharing, removal of obstacles and achieving higher goals. The main emphasis was to increase daily physical activity and to improve diet. Each participant was asked to record his/her food consumption and daily exercise activity. The records were reviewed by the workplace nurse and awarded with points. Participants were later rewarded for prizes and publicly praised in group meetings.
During the study, the researchers provided the study protocol and worked closely with the OHN at each site but served mainly on an advisory role, providing guidance and support. In order to avoid causing a bias due to frequent contact (of the researcher) with the participants, most intervention activities were delivered or led by OHN or the group leader. The involvement of the OHN to carry out the intervention activities is a necessary and important feature because it made the trial more in line with the real world conditions. The researcher worked closely with the OHN at all times during the course of the study.
As a health promotion project, all workplace workers were allowed to participate in activities that discuss about the basic health knowledge but only participants in the intervention group were organized to have group activities. Otherwise, workers in the reference group continued their daily routine. However, on ethical consideration, they were provided with free health promotion reading materials at each worksite. They could also have observed group activities or even talked with coworkers who were enrolled in the intervention group. No efforts were made (by the researcher or OHN) to influence their activities.
Outcome measures 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29
The major outcome measures were changes in lifestyle, anthropometric and blood biochemical variables. Each subject was independently interviewed, face-to-face, with a structured
questionnaire by a trained interviewer, measured for weight, height and waist circumference by a clinical nurse, and had an over-night fasting blood sample taken for determining biochemical indicators at the same time during the day for collection at both baseline (week-0) and endpoint (week-24) of the study.
Subjects were measured in light clothing without shoes. Height was measured to the nearest 0.1 cm and BW to the nearest 0.1 kg with a calibrated scale. Body mass index (BMI) was
calculated according to kg/m2. Waist circumference (WC) was measured at midpoint between the
lowest rib and the iliac crest without clothing cover during natural breathing. Arterial blood pressure (BP) was measured with a mercury sphygmomanometer. The average of two
measurements taken at 2- or 3-minute intervals with the workers in a seated position after resting for at least 10 minutes was used. An overnight fasting blood sample was taken from all
participants. Serum total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG) and glycosylated haemoglobin (HbA1c) concentrations were measured in a certified clinical laboratory. Low-density lipoprotein cholesterol (LDL-C) was calculated according to the equation of LDL-C = TC (mg) - HDL-C (mg) - [TG (mg)/5].
Statistical methods
Data were analysed using the PASW® Statistics 18.0 (SPSS Inc., Chicago, IL, USA). Descriptive
data were expressed with simple statistics. Chi-square test, Fisher’s exact test and independent t test were used to determine the homogeneity of the general characteristics between the
intervention and the reference groups. The significance of changes over time within each group was evaluated with paired-t test.Linear mixed-effects models were used to examine the
intervention effects by taking the within-workplace correlation as a random effect, and time, group and their interactions as fixed effects, adjusted for gender, age and job category. Statistical significance for all tests was set at α = 0.05.
Results 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29
Fifty-six of 58 subjects in the intervention group and 43 of 50 subjects in the reference group completed the study (Figure 1). Those who discontinued were mainly due to retirement and out-of-office job assignments.
Table 1 shows the characteristics of participants. The intervention group averaged 54.5 ± 3.8 years old and the reference group 55.7 ± 4.0 years old. The two groups were homogeneous in all socio-demographic characteristics, except cigarette-smoking. All participants had at least one metabolic disorder and the .
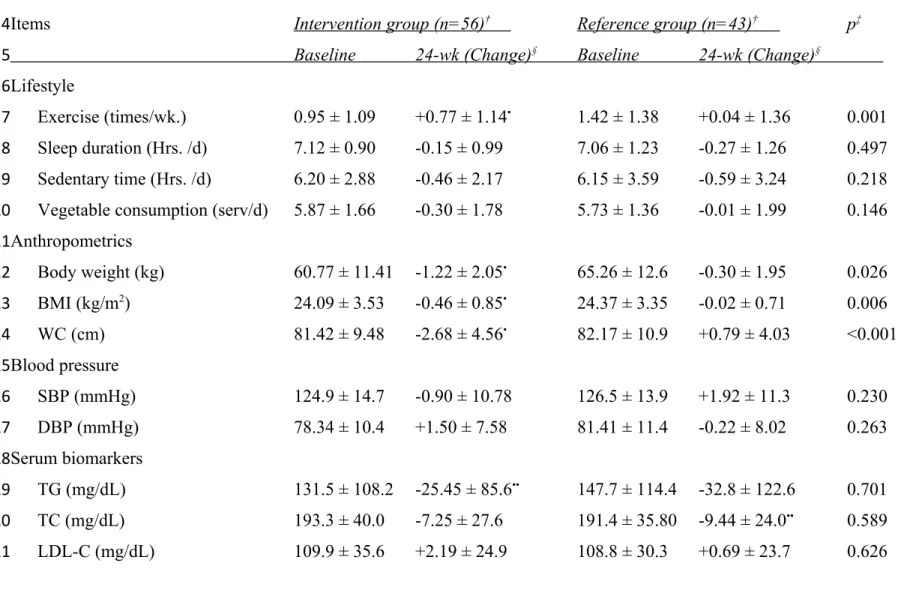
Table 2 shows the results at the end of 24-week trial. The intervention group had significantly higher frequency of exercise (p= 0.001), but no difference in vegetable
consumption, sleep duration or sedentary time. The intervention group had also significantly lower WC (3.44 cm, p <0.001) and BMI (0.44 kg/m2, p = 0.006) and significantly lower body
weight (0.92 kg, p = 0.026) compared to the reference group. However, there were no differences in blood pressure or serum biochemical parameters. There were significant time effects in both groups. In the reference group there were significant time-related decrease in total cholesterol and HDL-C concentrations. In the intervention group, there was a significant increase in the frequency of exercise and significant decreases in weight, BMI, WC, TG and HDL-C at end-point compared to the baseline values.
Discussion
Our study suggests that a flexible, individualized, non-enforced worksite-based health promotion program can be an effective and useful strategy to achieve some level of lifestyle changes to reduce the risk of the aging-associated metabolic disorders in older SME workers in Taiwan. The intervention group significantly reduced WC, body weight and BMI. However, the intervention did not improve sedentary time, sleep duration, vegetable consumption, blood pressure, or serum lipid and HbA1c levels. These results are consistent with earlier studies that lifestyle intervention is generally easier to have improvements in weight indicators especially waist circumference than blood biochemical indicators (4).
Our program seems to impact exercise frequency more than other aspects of lifestyle. The treatment nearly doubled the frequency of exercise but did not significantly change vegetable consumption, sleep duration or sedentary time. These findings are consistent with the findings of 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
others that lifestyle intervention can produce significant change in physical activity, reduce body weight and other weight-related indicators especially waist circumference (17, 18). The program affected more on body fat or weight than biochemical indicators. We observed a decrease of 3.47cm in WC, a change comparable to results observed by others (19-22). Atlantis et al. (19) observed a reduction of 3cm in a 24-week study that combined supervised moderate-to-high intensity exercise and dietary restriction to 30-year old healthy but sedentary Australian casino workers. Christensen et al. (20) observed a 3.3cm reduction in >45 year-old overweight Danish healthcare workers with an intervention program that involved individual dietary plan, physical exercise and behavioral training for 3 months. Murphy et al. (21) observed a 1 cm difference between walking and control groups in an 8-week walking program (twice/week for 45 minutes at 62% HRmax). Freak-Poli et al. (22) reported an improvement of 1.6cm in a study involving 762
participants in a four-month, pedometer-based walking. All these studies involved more structured intervention programs than the present study.
The present study also observed a significant decrease in BMI (-0.44kg/m2) and significant
net reduction in BW (-0.92kg, P = 0.026). These results are comparable with results observed by Muto and Yamauchi (23) who observed a 1.7kg reduction in body weight and 0.5 kg/m2 in BMI
in a 6-month instructor-led multi-component education program in workers of a building maintenance company in Japan.
It is probable that the increase in physical activity is the major reason for the observed decrease in WC, BMI and body weight in the present study. However, it does not affect sedentary time. The intervention appears to have little impact on the frequency of intake of the major food items. It is probably easier to increase physical activity than to change food pattern because changing food choice involves food preparation for other members of the family, or foods might be prepared by other members of the family. Other studies have suggested that it is easier to change physical activity than dietary pattern (17, 24).
Although there were some significant time-related within-group changes in serum biochemical indicators, our intervention appears to be inadequate to have sufficient impact on biochemical indicators. Generally speaking, non-supervised intervention was probably not sufficient to cause a significant improvement in dietary pattern or biochemical changes (25). The length of intervention could be another reason. A 24-week intervention is probably not long 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
enough to show significant improvement in blood biochemical indicators, especially for non-supervised intervention. There are also other possible reasons. We undertook the study as a health promotion project and conducted it under a real-world condition and as such we accepted all workers who met age and full employment criteria regardless of their health conditions (having any metabolic disorder or not). We also made no attempt to avoid self-initiated lifestyle changes by subjects who were assigned to the reference group. Subjects in the reference group could have observed or discussed with coworkers in the intervention group and initiated lifestyle changes. These actions could have partially offset some of the intervention effects.
In the present study, neither the intervention nor the study time had any significant effect on BP, or TC, LDL-C and HbA1c concentrations. These results are consistent with those observed in some earlier studies (4, 26). Generally speaking, studies that implemented more strict dietary changes have achieved significant improvement in blood lipid indicators while studies that placed greater emphasis on smoking cessation showed significant changes in BP. Since dietary modifications and smoking cessation were voluntary in the present study (and there were few smokers in the study sample), the behavioral changes were probably not enough to cause a significant change in these parameters.
The special feature of the present study is that we took a pragmatic approach and applied a flexible program to allow subject to choose their own activities and set their own goals. We tried to encourage or motivate subjects to improve their lifestyle but we did not try to enforce strict actions. We also made no attempt to discourage or restrict the workers in the reference group from self-initiated lifestyle changes. Furthermore, study subjects had diverse metabolic disorders. Not everyone was overweight/obese, hypertensive, hyperglycemic or having dyslipidemia. For example, only about 50% of subjects were over-weight/obese, 40% had excessive waist circumference, and 20% had low HDL-C. Thus, those who had no need to improve will dilute the intervention effect.
The study has limitations. This study is a quasi-experiment, not a randomized controlled trial. Interest-based group assignment could have selection bias. Additionally, the 24-week study period might not be long enough to have many of the expected improvements. Moreover, all intervention actions were voluntary; therefore the intensity and adherence were not enforced. On the other hand, self-initiated lifestyle changes were not prevented. Improving social support 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
could have resulted as a by-product of hosting presentations, group sessions and providing phone and email contact. Although attempted, we found participants had difficulty keeping record of daily physical activity or dietary records. Thus, we could not analyze their food patterns or dietary intakes. Their physical activities also fluctuated according to their work schedules and work demand. Their availability to participate group activities was also greatly influenced by work scheduling. Some workers were unable to carry out activities as planned. These limitations are the reality of WHP. As a result, we encountered many difficulties during the study. There was a lack of consistent support from the management. Although we were promised of support and making time available for workers to take part in study activities from the top management, the lower level management often failed to keep those promises. As a result, many of the planned activities were forced to cut short.
Overall, we observed a lack of incentive for the business to invest in employee's health and the reason seems obvious. Under the current universal healthcare policy in Taiwan, the employer pays a fixed share of employee's health insurance premium regardless of worker's healthcare cost or health condition. Most employers also appear to be unconvinced that health promotion will translate into better productivity or profit for the business. We observed few business-initiated health promotion activities at the sites studied. We also observed no obvious structural or
organizational changes regarding workers health promotion activities by the management during the course of the study or after the completion of the study as a result of this study. Lastly, the workplace health service units did not seem to play an active role in initiating or implementing health promoting activities.
Conclusion and implications
Despite the difficulties and because of these difficulties, it is imperative to carry out this and more studies. We have shown that worksite-based health promotion can achieve considerable success in workers' health by improving WC, BMI and BW. Finally, we got positive feedback collected from the participants that some ask for continuation of program and expand to other factory. Given that older SME workers have high health risks and are probably one of the most neglected groups in Taiwan, our study can serve as a basic model for WHP in Taiwan. We also believe that greater success is possible, but it is much dependent on government's actions and 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
employer's incentive to invest in workers' health. 1
Conflict of Interests
The author(s) declare(s) that there is no conflict of interests regarding the publication of this article. 1 2 3 4 5
References
1. Chen MM, Tsai AC. The Effectiveness of IDF and ATP-III in identifying metabolic
syndrome and the usefulness of these tools for health-promotion in older Taiwanese. J Nutr Health Aging. 2013; 17: 413-416.
2. Kvaavik E, Batty GD, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom health and lifestyle survey. Arch Intern Med. 2010; 170: 711-718.
3. Varekamp I, Krol B, van Dijk FJ. Empowering employees with chronic diseases: process evaluation of an intervention aimed at job retention. Int Arch Occup Environ Health. 2011; 84: 35-43.
4. Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease – a systematic review. Scand J Work Environ Health. 2010; 36: 202-215.
5. The Directorate General of Budget, Accounting and Statistics of Executive Yuan, Taiwan “2006 Commerce and Service Census Report,” Taipei: The Directorate General of Budget, Accounting and Statistics (DGBAS) of Executive Yuan, Taiwan. 2008.
6. Council of Labor Affairs. Labor Statistics, 2012 , Http://Statdb.Cla.Gov.Tw/Statis/Stmain.Jsp?
Sys=210&Kind=21&Type=1&Funid=Q02024&Rdm=Ujt4drgq (accessed 25 June 2012) 7. Health Promotion Administration, Taiwan. Self-Certification of Healthy Workplace, 2012,
http://www.bhp.doh.gov.tw/BHPnet/English/ClassShow.aspx?No=200806230002 (accessed 3 July 2012).
8. Naumanen P. Opinions of ageing workers on relative importance of health promotion. Int J Nurs Pract. 2006; 12: 352-358.
9. McDermott HJ, Kazi A, Munir F, Haslam C. Developing occupational health services for active age management. Occup Med. 2010; 60: 193-204.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26
10. Fan KT, Yen LL. Health promotion in the workplace: comparison of the experiences of Taiwan and other countries. Taiwan J Pub Health. 2008; 27: 271-278.
11. Ilmarinen J. The ageing workforce--challenges for occupational health. Occup Med. 2006; 56: 362-364.
12. Kim SH. Older people's expectations regarding ageing, health-promoting behaviour and health status. J Adv Nurs. 2009; 65: 84-91.
13. Bonnie LH, van den Akker M, van Steenkiste B, Vos R. Degree of solidarity with lifestyle and old age among citizens in the Netherlands: cross-sectional results from the longitudinal SMILE study. J Med Ethics. 2010; 36: 784-790.
14. Donovan R, Nelson T, Peel J, Lipsey T, Voyles W, Israel RG. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med. 2009; 59: 487-492.
15. Robroek SJ, van Lenthe FJ, van Empelen P, Burdorf A. Determinants of participation in workplace health promotion programmes: a systematic review. IntJ Behav Nutr Phys Act. 2009; 6:26.
16. Noordzij M, Dekker FW, Zoccali C, Jager KJ. Sample Size Calculations. Nephron Clin Pract. 2011; 118: c319-c323.
17. Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, et al. Efficacy of a workplace-based weight loss program for overweight male shift workers: the Workplace POWER (Preventing Obesity Without Eating like a Rabbit) randomized controlled trial. Prev Med. 2011; 52: 317-325.
18. Robroek SJ, Lindeboom DE, Burdorf A. Initial and sustained participation in an internet-delivered long-term workplace health promotion program on physical activity and nutrition. J Med Int Res. 2012; 14: e43.
19. Atlantis E, Chow CM, Kirby A, Fiatarone Singh MA. Workplace intervention effects on physical health: a randomized controlled trial. Health Promot Int. 2006; 21: 191-200. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25
20. Christensen JR, Faber A, Ekner D, Overgaard K, Holtermann A, Sogaard K. Diet, physical exercise and cognitive behavioral training as a combined workplace based intervention to reduce body weight and increase physical capacity in health care workers - a randomized controlled trial. BMC Public Health. 2011; 11: 671.
21. Murphy MH, Murtagh EM, Boreham CA, Hare LG, Nevill AM. The effect of a workplace based walking programme on cardiovascular risk in previously sedentary civil servants [NCT00284479]. BMC Public Health. 2006; 6: 136.
22. Freak-Poli R, Wolfe R, Backholer K, de Courten M, Peeters A. Impact of a pedometer-based workplace health program on cardiovascular and diabetes risk profile. Prev Med. 2011; 53: 162-171.
23. Muto T, Yamauchi K. Evaluation of a multicomponent workplace health promotion program conducted in Japan for improving employees' cardiovascular disease risk factors. Prev Med. 2001; 33: 571-577.
24. Vengiau G, Umezaki M, Phuanukoonnon S, Siba P, Watanabe C. Diet and physical activity among migrant Bougainvilleans in Port Moresby, Papua New Guinea: association with anthropometric measures and blood pressure. Am J Hum Biol. 2012; 24: 716-718.
25. Kant AK. Dietary patterns: biomarkers and chronic disease risk. Appl Physiol Nutr Metab. 2010; 35: 199-206.
26. Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W. The effectiveness of workplace physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med. 2003; 13: 106-117.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24
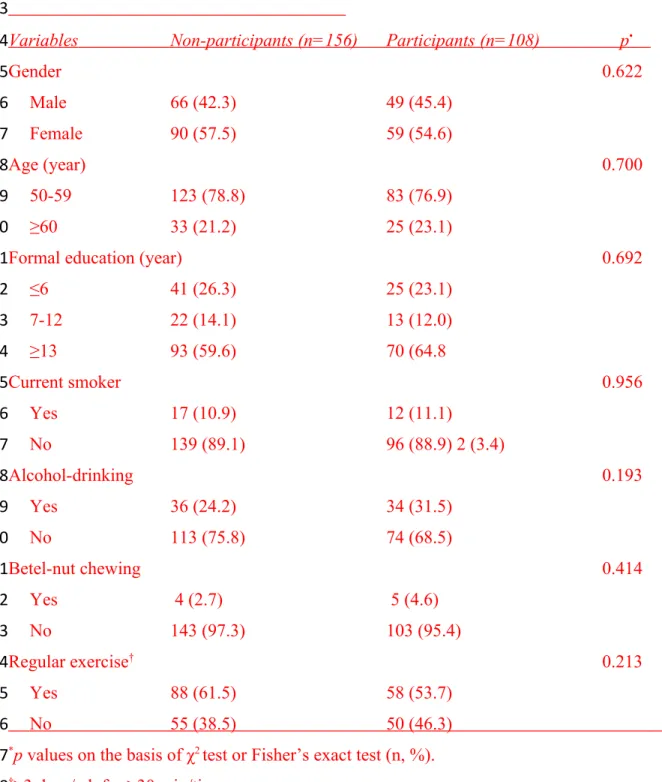
Table 1. Demographic characteristics of the subjects who completed a prescreening questionnaire
Variables Non-participants (n=156) Participants (n=108) p •
Gender 0.622 Male 66 (42.3) 49 (45.4) Female 90 (57.5) 59 (54.6) Age (year) 0.700 50-59 123 (78.8) 83 (76.9) ≥60 33 (21.2) 25 (23.1)
Formal education (year) 0.692
≤6 41 (26.3) 25 (23.1) 7-12 22 (14.1) 13 (12.0) ≥13 93 (59.6) 70 (64.8 Current smoker 0.956 Yes 17 (10.9) 12 (11.1) No 139 (89.1) 96 (88.9) 2 (3.4) Alcohol-drinking 0.193 Yes 36 (24.2) 34 (31.5) No 113 (75.8) 74 (68.5) Betel-nut chewing 0.414 Yes 4 (2.7) 5 (4.6) No 143 (97.3) 103 (95.4) Regular exercise† 0.213 Yes 88 (61.5) 58 (53.7) No 55 (38.5) 50 (46.3) *p values on the basis of χ2 test or Fisher’s exact test (n, %).
†≥3 days/wk for ≥30 min/time. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
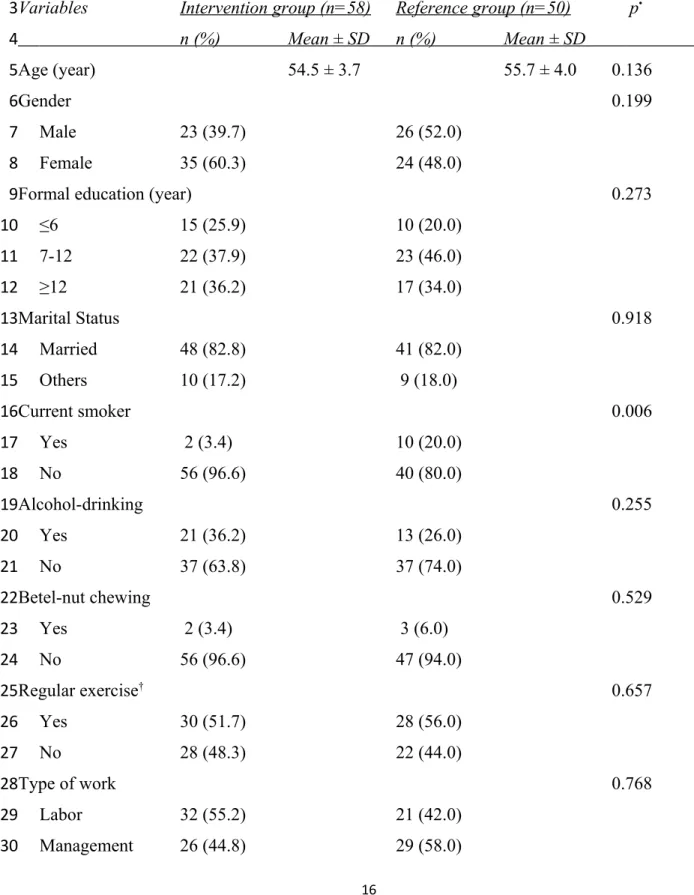
Table 1. Socio-demographic characteristics of the study subjects
Variables Intervention group (n=58) Reference group (n=50) p•
n (%) Mean ± SD n (%) Mean ± SD Age (year) 54.5 ± 3.7 55.7 ± 4.0 0.136 Gender 0.199 Male 23 (39.7) 26 (52.0) Female 35 (60.3) 24 (48.0)
Formal education (year) 0.273
≤6 15 (25.9) 10 (20.0) 7-12 22 (37.9) 23 (46.0) ≥12 21 (36.2) 17 (34.0) Marital Status 0.918 Married 48 (82.8) 41 (82.0) Others 10 (17.2) 9 (18.0) Current smoker 0.006 Yes 2 (3.4) 10 (20.0) No 56 (96.6) 40 (80.0) Alcohol-drinking 0.255 Yes 21 (36.2) 13 (26.0) No 37 (63.8) 37 (74.0) Betel-nut chewing 0.529 Yes 2 (3.4) 3 (6.0) No 56 (96.6) 47 (94.0) Regular exercise† 0.657 Yes 30 (51.7) 28 (56.0) No 28 (48.3) 22 (44.0) Type of work 0.768 Labor 32 (55.2) 21 (42.0) Management 26 (44.8) 29 (58.0) 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
Working years 22.6 ± 9.3 25.5 ± 9.9 0.111
Sleep duration (hr/d) 7.09 ± 0.90 7.16 ± 1.78 0.737
Sedentary time (hr/d) 6.15 ± 3.02 6.30 ± 3.71 0.818
*p values on the basis of t-test (mean, SD), or χ2 test or Fisher’s exact test (n, %). †≥3 days/wk for ≥30 min/time.
1 2 3 4 5 6
Table 2. Effects of a 24-week lifestyle intervention on lifestyle, anthropometric, blood pressure and serum biochemical variables (mean ± SD) in ≥50-year old workers in Taiwan
Items Intervention group (n=56)† Reference group (n=43)† p‡
Baseline 24-wk (Change)§ Baseline 24-wk (Change) §
Lifestyle
Exercise (times/wk.) 0.95 ± 1.09 +0.77 ± 1.14• 1.42 ± 1.38 +0.04 ± 1.36 0.001
Sleep duration (Hrs. /d) 7.12 ± 0.90 -0.15 ± 0.99 7.06 ± 1.23 -0.27 ± 1.26 0.497 Sedentary time (Hrs. /d) 6.20 ± 2.88 -0.46 ± 2.17 6.15 ± 3.59 -0.59 ± 3.24 0.218 Vegetable consumption (serv/d) 5.87 ± 1.66 -0.30 ± 1.78 5.73 ± 1.36 -0.01 ± 1.99 0.146 Anthropometrics Body weight (kg) 60.77 ± 11.41 -1.22 ± 2.05• 65.26 ± 12.6 -0.30 ± 1.95 0.026 BMI (kg/m2) 24.09 ± 3.53 -0.46 ± 0.85• 24.37 ± 3.35 -0.02 ± 0.71 0.006 WC (cm) 81.42 ± 9.48 -2.68 ± 4.56• 82.17 ± 10.9 +0.79 ± 4.03 <0.001 Blood pressure SBP (mmHg) 124.9 ± 14.7 -0.90 ± 10.78 126.5 ± 13.9 +1.92 ± 11.3 0.230 DBP (mmHg) 78.34 ± 10.4 +1.50 ± 7.58 81.41 ± 11.4 -0.22 ± 8.02 0.263 Serum biomarkers TG (mg/dL) 131.5 ± 108.2 -25.45 ± 85.6•• 147.7 ± 114.4 -32.8 ± 122.6 0.701 TC (mg/dL) 193.3 ± 40.0 -7.25 ± 27.6 191.4 ± 35.80 -9.44 ± 24.0•• 0.589 LDL-C (mg/dL) 109.9 ± 35.6 +2.19 ± 24.9 108.8 ± 30.3 +0.69 ± 23.7 0.626 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
HDL-C (mg/dL) 57.07 ± 14.4 -4.35 ± 7.70• 49.81 ± 12.8 -3.34 ± 5.63• 0.417
HbA1c (%) 6.26 ± 0.96 -0.01 ± 0.28 6.43 ± 1.67 +0.06 ± 0.79 0.497 WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; HDL, high-density
lipoprotein cholesterol; BMI, body mass index; BW, body weight; HbA1c, glycosylated hemoglobin; TC, total cholesterol; LDL, low-density lipoprotein cholesterol;
†Seven subjects in the reference group and 2 subjects in the intervention group did not complete the end-point tests. ‡p-values of the interaction (time*group) in the linear mixed models, adjusted for gender, age, job category and worksite. •Significant time effect on the basis of Student's paired t-test, p < 0.05, ••p < 0.001
§Net change from the value at baseline.
1 2 3 4 5 6 7 8 9 10 11
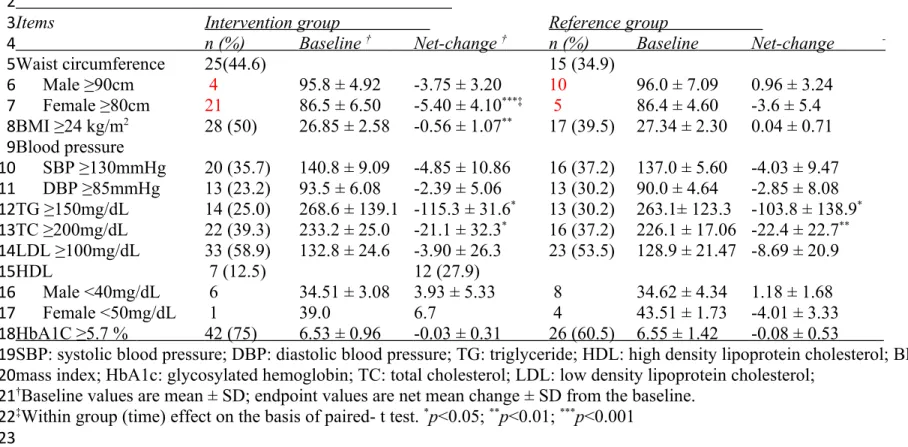
Table 3. Effect of lifestyle intervention on the status of metabolic disorders (this table was added on 07-18-14)
Items Intervention group Reference group
n (%) Baseline † Net-change † n (%) Baseline Net-change
-Waist circumference 25(44.6) 15 (34.9) Male ≥90cm 4 95.8 ± 4.92 -3.75 ± 3.20 10 96.0 ± 7.09 0.96 ± 3.24 Female ≥80cm 21 86.5 ± 6.50 -5.40 ± 4.10***‡ 5 86.4 ± 4.60 -3.6 ± 5.4 BMI ≥24 kg/m2 28 (50) 26.85 ± 2.58 -0.56 ± 1.07** 17 (39.5) 27.34 ± 2.30 0.04 ± 0.71 Blood pressure SBP ≥130mmHg 20 (35.7) 140.8 ± 9.09 -4.85 ± 10.86 16 (37.2) 137.0 ± 5.60 -4.03 ± 9.47 DBP ≥85mmHg 13 (23.2) 93.5 ± 6.08 -2.39 ± 5.06 13 (30.2) 90.0 ± 4.64 -2.85 ± 8.08 TG ≥150mg/dL 14 (25.0) 268.6 ± 139.1 -115.3 ± 31.6* 13 (30.2) 263.1± 123.3 -103.8 ± 138.9* TC ≥200mg/dL 22 (39.3) 233.2 ± 25.0 -21.1 ± 32.3* 16 (37.2) 226.1 ± 17.06 -22.4 ± 22.7** LDL ≥100mg/dL 33 (58.9) 132.8 ± 24.6 -3.90 ± 26.3 23 (53.5) 128.9 ± 21.47 -8.69 ± 20.9 HDL 7 (12.5) 12 (27.9) Male <40mg/dL 6 34.51 ± 3.08 3.93 ± 5.33 8 34.62 ± 4.34 1.18 ± 1.68 Female <50mg/dL 1 39.0 6.7 4 43.51 ± 1.73 -4.01 ± 3.33 HbA1C ≥5.7 % 42 (75) 6.53 ± 0.96 -0.03 ± 0.31 26 (60.5) 6.55 ± 1.42 -0.08 ± 0.53
SBP: systolic blood pressure; DBP: diastolic blood pressure; TG: triglyceride; HDL: high density lipoprotein cholesterol; BMI: body mass index; HbA1c: glycosylated hemoglobin; TC: total cholesterol; LDL: low density lipoprotein cholesterol;
†Baseline values are mean ± SD; endpoint values are net mean change ± SD from the baseline. ‡Within group (time) effect on the basis of paired- t test. *p<0.05; **p<0.01; ***p<0.001
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23
56 completed the study 43 completed the study 2 retired, 5 dropped out 2 dropped out
Intervention group (N=58) Reference group (N=50)
330 declined to join the study 1245 total workers in 3 worksites and 438 ≥50 years old (35.2%)
108 agreed to take part in the study and were assigned to the reference or intervention group according to their availability to take part in activities
Figure 1. Study flowchart 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19