Psychiatry and Clinical Neurosciences (2007), 61, 105–111 doi:10.1111/j.1440-1819.2007.01618.x
Correspondence address: Dr Chih-Ken Chen, MD, PhD, Depart-ment of Psychiatry, Chang Gung Memorial Hospital, 222 Mai-Chin Road, Keelung, 204 Taiwan. Email: kenchen@cgmh.org.tw
Received 13 June 2006; revised 8 September 2006; accepted 15 September 2006.
Regular Article
Psychiatric comorbidity and gender difference among
treatment-seeking heroin abusers in Taiwan
SHU-CHUAN CHIANG, md, ms,1,2 HUNG-YU CHAN, md,1 YUAN-YING CHANG, md,3
HSIAO-JU SUN, md,1 WEI J. CHEN, md, scd4 AND CHIH-KEN CHEN, md, phd5,6,7
1Tao-Yuan Psychiatric Center, Department of Health, Executive Yuan, 3Tzu-Li Clinic, 6Chang Gung University
School of Medicine, Taoyuan, 2Chia Nan University of Pharmacy and Science, Tainan, 4Institute of
Epidemiology, College of Public Health, National Taiwan University, 7Division of Mental Health and Drug Abuse Research, National Health Research Institutes, Taipei and 5Department of Psychiatry, Chang Gung Memorial Hospital, Keelung, Taiwan
Abstract The objectives of the present study were to estimate the psychiatric comorbidity of Taiwanese
her-oin users seeking treatment and to identify the gender differences in psychiatric comorbidity and drug use behavior. Subjects were interviewed using a structured questionnaire on drug use behav-ior and the Mini International Neuropsychiatric Interview for psychiatric disorders. Of the sub-jects, 58.5% of the male and 62.5% of the female subjects had at least one non-substance-use axis I psychiatric disorder or antisocial personality disorder. Compared to male subjects, female sub-jects were younger, were less educated, had higher rates of unemployment and had earlier onset of illicit drug use. Female subjects were 11-fold more likely than male subjects to exhibit suicidal behavior. Among heroin abusers in the present study, female subjects were more widely exposed to unfavorable social factors and had substantially higher incidence of suicidal behavior than male subjects. Drug treatment centers should be aware of these gender differences and pay particular attention to comorbid depressive disorders and suicidal behavior of female heroin abusers.
Key words comorbidity, gender, heroin, substance abuse.
INTRODUCTION
Heroin dependence is a lifelong disease associated with high rates of health problems, mental health prob-lems, and involvement with the criminal justice sys-tem.1 Hser et al. showed that after a 33-year follow-up,
40.5% of heroin users studied had used heroin within the previous year.1 Those with drug use disorders
typ-ically have other mental disorders with reported comorbidity rates of 53%. Major depressive disorder, alcoholism and antisocial personality are comorbid psychiatric disorders common among substance abus-ers.2 Studies have shown that at least 46–86.9% of
patients with heroin dependence have at least one comorbid psychiatric disorder.2–4 Khantzian and Treece
reported that 77% of narcotic addicts met criteria for one or more diagnoses on axis I, and 65% met the cri-teria for a personality disorder on axis II.4 In total, 93%
of users met the criteria for one or more psychiatric disorders other than substance abuse.2 Chen et al.
examined psychiatric comorbidity among hospitalized and incarcerated male heroin addicts in Taiwan, con-cluding that the most prevalent coexisting axis I disor-ders were additional substance use disordisor-ders and mood disorders, and antisocial personality disorder was the most frequent axis-II diagnosis.5 Chen et al. also
deter-mined that 83% of hospitalized users were diagnosed with at least one coexisting axis I or II disorder.5 High
psychiatric comorbidity confounds the treatment course for drug dependence, typically leading to poor prognosis. For example, among opioid addicts, depres-sion is the predominant risk factor for continued drug use.6–8
Women were previously perceived as subject to pro-portionally fewer substance abuse problems than men, and numerous studies of both alcoholism and drug
abuse focused exclusively on male subjects. In the United Kingdom, the male to female ratio for illicit drug use is approximately 3:1.9 In the Epidemiological
Catchment Area study conducted in the early 1980s, 1-month prevalence rates for drug use disorders in male subjects were two- or threefold higher than for women.2 However, recent studies showed that gender
differences in prevalence rates for drug use disorder are lower than expected.10 The National Comorbidity
Study identified lifetime prevalence of drug depen-dence as 9.2% for men and 5.9% for women.11 The
National Household Survey on Drug Abuse showed that lifetime illicit drug use for women is approxi-mately 30%, whereas that in men is 40%.12 Moreover,
although drug abuse in women is less common than that in men, female addicts have higher rates of psy-chiatric comorbidity than male addicts.2,3,13
Differences between male and female subjects in many aspects (e.g. etiological consideration and psychi-atric comorbidity) of substance use disorders have received increasing attention over the past decade. Female opiate addicts have been shown to be fre-quently unemployed, have high rates of depression and anxiety disorders, and more severe medical problems than men.14 Heroin and methamphetamines are the
principal illicit drugs used in Taiwan.15 Compared with
male methamphetamine abusers, more female meth-amphetamine abusers in Taiwan reported having mental disturbances and suicidal behaviors.16 Previous
studies of female heroin addicts in Taiwan have focused primarily on demographics and drug use behavior. No systemic assessment of gender differ-ences in psychiatric comorbidities exist for heroin addicts in Taiwan. The primary aims of the present study were to characterize demographic and psychoso-cial features, drug-related experiences, clinical mani-festations, and comorbid disorders in relation to heroin use; and to determine gender differences in psychoso-cial characteristics, drug use behavior and psychiatric comorbidity.
METHODS Study participants
Study subjects were heroin abusers who visited the outpatient department at Tao-Yuan Psychiatric Center (TYPC) in Northern Taiwan from March to September 2002. The eligibility criteria were: (i) males or females, aged more than 15; and (ii) meeting the DSM-IV criteria for heroin abuse or heroin dependence. One hundred and fifty-five subjects were recruited consec-utively. Subjects were guaranteed that all personal information was strictly confidential. Informed consent
was obtained from each subject. This investigation was approved by the institutional review boards at TYPC.
Measurements
Subjects were interviewed using a structured question-naire on drug use behavior, which was previously used to assess illicit drug use behavior17 and the Mini
Inter-national Neuropsychiatric Interview (MINI).18 All
interviews were conducted by a well-trained psycholo-gist who had received a 30-day training program in TYPC and was supervised by the first author, a senior psychiatrist specializing in treatment of substance use disorders.
The structured questionnaire for drug use behavior was designed to assess severity of illicit drug addiction. This questionnaire consisted of three sections: (i) per-sonal history (demographic data, history of physical illness, developmental history, sociodemographic back-ground, and family history); (ii) substance use history (age at initial use, duration and frequency of using a variety of substances, including alcohol and illicit drugs, such as heroin, methamphetamines, marijuana, and glue; glue sniffing is prohibited by the Social Order Maintenance Law in Taiwan); and (iii) criminal history (both previous criminal records and off-the-record ille-gal behaviors).
The MINI is a short structured diagnostic interview for DSM-IV or ICD-10 psychiatric disorders.18 It has
been shown to have good reliability and has been widely used in international clinical trials and epidemi-ological studies.19,20 The MINI was translated into
Mandarin by the Taiwan Society of Psychiatry; its inter-rater reliability was approximately 0.75 in previous studies.21,22
Data analysis
Group comparisons of categorical variables between male and female heroin users were analyzed using Fisher’s exact test, and comparison of continuous variables were done with the Student’s t-test. All continuous variables are presented as means ± SD. A two-tailed value of P < 0.05 was considered statistically significant. All statistical analyses were done with SPSS version 11 (SPSS, Chicago, IL, USA).
RESULTS Demographics
Of 155 subjects enrolled, 123 were male and 32 were female. The mean age was 30.8 ± 7.7 years. The women were significantly younger than the men (Table 1). Women also had fewer years of formal education than
men. No significant gender differences were found for employment status, criminal records, or marital status. Compared with the male subjects, female heroin users were more likely to have a family history of alcohol use disorders, while there was no significant between-gender difference in rates of family history of illicit drug use or in rates of living with substance abusers.
Drug use patterns
Mean age at first heroin use was 25.4 ± 6.7 years and mean duration of heroin use was 5.4 ± 4.6 years.
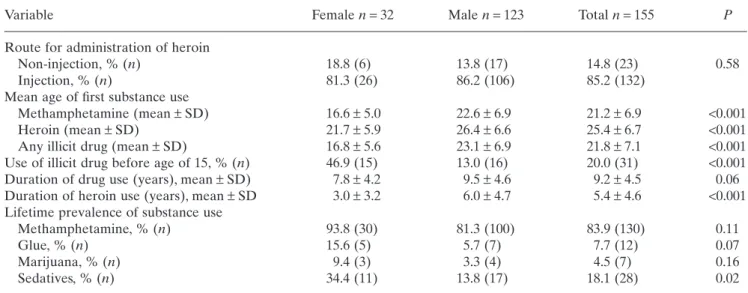
Table 2 presents the results for heroin use patterns and drug use history between male and female subjects. Compared with the men, women were significantly younger at first heroin use, and younger at first use of any illicit drug, whereas the men used heroin for longer periods than the women. Two methods of heroin use were found: smoking of heroin mixed with tobacco in cigarettes, and injecting of heroin. Twenty-three sub-jects smoked heroin (without prior experience of injecting heroin), and 132 injected heroin. No signifi-cant gender differences were noted for administration methods. In addition to heroin, the most frequently Table 1. Demographic characteristics of opiate addicts by gender
Variables Female n = 32 Male n = 123 Total n = 155 P-value
Age (years), mean ± SD 24.7 ± 6.0 32.4 ± 7.3 30.8 ± 7.7 <0.001
Year of education, mean ± SD 9.2 ± 2.7 10.6 ± 1.8 10.3 ± 2.1 0.001
Employment status 0.09 Employed, % (n) 53.1 (17) 70.7 (87) 67.1 (104) Unemployed, % (n) 46.9 (15) 29.3 (36) 32.9 (51) Marital state 0.38 Single, % (n) 71.9 (23) 58.5 (72) 61.3 (95) Married, % (n) 18.8 (6) 29.3 (36) 27.1 (42) Divorced, % (n) 9.4 (3) 12.2 (15) 11.6 (18)
Family history of illicit drug use 12.5 (4) 10.6 (13) 11.0 (17) 0.75
Family history of alcohol use disorders 43.8 (14) 21.1 (26) 25.8 (40) 0.01
Living with alcohol/drug abusers 34.4 (11) 17.1 (21) 20.6 (32) 0.05
Criminal record
Any conviction, % (n) 62.5 (20) 71.5 (88) 69.7 (108) 0.39
Illicit drug use, % (n) 62.5 (20) 63.4 (78) 63.2 (98) 1.0
Violent crime†, % (n) 6.3 (2) 17.1 (21) 14.8 (23) 0.17
Other crime, % (n) 0 (0) 8.9 (11) 7.1 (11) 0.12
† Violent crimes included crimes against persons, property crimes; other crimes included prostitution and sex offense.
Table 2. Drug use history of opiate addicts by gender
Variable Female n = 32 Male n = 123 Total n = 155 P
Route for administration of heroin
Non-injection, % (n) 18.8 (6) 13.8 (17) 14.8 (23) 0.58
Injection, % (n) 81.3 (26) 86.2 (106) 85.2 (132)
Mean age of first substance use
Methamphetamine (mean ± SD) 16.6 ± 5.0 22.6 ± 6.9 21.2 ± 6.9 <0.001
Heroin (mean ± SD) 21.7 ± 5.9 26.4 ± 6.6 25.4 ± 6.7 <0.001
Any illicit drug (mean ± SD) 16.8 ± 5.6 23.1 ± 6.9 21.8 ± 7.1 <0.001
Use of illicit drug before age of 15, % (n) 46.9 (15) 13.0 (16) 20.0 (31) <0.001 Duration of drug use (years), mean ± SD) 7.8 ± 4.2 9.5 ± 4.6 9.2 ± 4.5 0.06 Duration of heroin use (years), mean ± SD 3.0 ± 3.2 6.0 ± 4.7 5.4 ± 4.6 <0.001 Lifetime prevalence of substance use
Methamphetamine, % (n) 93.8 (30) 81.3 (100) 83.9 (130) 0.11
Glue, % (n) 15.6 (5) 5.7 (7) 7.7 (12) 0.07
Marijuana, % (n) 9.4 (3) 3.3 (4) 4.5 (7) 0.16
Table 3. Axis I non-substance use psychiatric disorders of opiate addicts by gender Category Female n = 32 % (n) Male n = 123 % (n) Total n = 155 % (n) OR (95%CI) P
Any axis I disorder 50.0 (16) 30.1 (37) 34.2 (53) 2.3 (1.1–5.1) 0.04
Mood disorder 37.5 (12) 11.4 (14) 16.8 (26) 4.7 (1.9–11.6) 0.001
Major depressive disorder 28.1 (9) 8.9 (11) 12.9 (20) 4.0 (1.5–10.7) 0.006
Dysthymic disorder 25.0 (8) 5.7 (7) 9.7 (15) 5.5 (1.8–16.7) 0.002
Bipolar disorder 0 0 0
Anxiety disorder 34.4 (11) 26.8 (33) 28.4 (44) 1.4 (0.6–3.3) 0.4
General anxiety disorder 28.1 (9) 25.2 (31) 25.8 (40) 1.2 (0.5–2.8) 0.74
Obsessive-compulsive disorder† 0.8 (1) 0.6 (1) – 1.0
Panic disorder 3.1 (1) 0 0.6 (1) – 1.0
Agoraphobia 3.1 (1) 0 0.6 (1) – 1.0
Specific phobia† 10.0 (3) 1.6 (2) 3.3 (5) 6.7 (1.1–41.9) 0.04
Social phobia 0 0 0 –
Post-traumatic stress disorder 0 0 0
Eating disorder 3.1 (1) 0 0.6 (1) – 1.0
Psychotic disorder 0 0.8 (1) 0.6 (1) – 1.0
Psychotic disorder, lifetime 3.1 (1) 2.5 (3) 2.6 (4) 1.3 (0.1–12.8) 0.83
Antisocial personality disorder† 26.7 (8) 43.0 (52) 39.7 (60) 0.5 (0.2–1.2) 0.11 Conduct disorder before age of 15† 54.8 (17) 50.0 (61) 51.0 (78) 1.2 (0.6–2.7) 0.63
Current suicidal risk 68.8 (22) 33.3 (41) 40.6 (63) 4.4 (1.9–10.2) 0.001
Low or moderate risk 40.9 (9) 90.2 (37) 73.0 (46) <0.001
High risk 59.1 (13) 9.8 (4) 27.0 (17)
Suicide attempts, lifetime 46.9 (15) 4.1 (5) 12.9 (20) 20.8 (6.7–64.6) <0.001 OR, odds ratio; CI, confidence interval.
† Missing data.
used illicit drug was methamphetamine. Compared with the men, more women abused sedatives, while there was no between-gender difference in lifetime prevalence of abusing methamphetamine, glue, or marijuana.
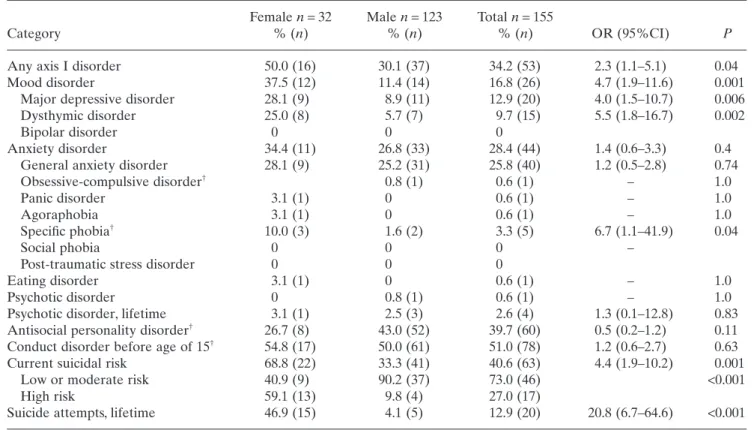
Psychiatric comorbidity
Both the male and the female subjects had high comor-bid rates for psychiatric illnesses. Of the 155 subjects, 58.5% of the male and 62.5% of the female subjects had at least one non-substance use axis I psychiatric disorder or antisocial personality disorder. The most frequently diagnosed comorbidity was mood disorder for the women and antisocial personality disorder for the men (Table 3). When all axis I psychiatric diagnoses were considered, more than one-third of participants had at least one psychiatric disorder other than a sub-stance use disorder. Compared with male subjects, the women had a substantially higher rate of axis I psychi-atric diagnosis other than substance use disorder. Of these 155 subjects, anxiety and mood disorders were the most frequently diagnosed comorbidities. Female subjects had significantly higher rates of mood
disorders than the men. Women had a higher rate of specific phobia than male subjects, while there was no between-gender difference in prevalence of other anx-iety disorders, eating disorder, or psychotic disorders. Four patients had lifetime experiences of psychotic dis-orders, and all of them had a history of methamphet-amine abuse. For personality-related disorders, 40% of subjects met the criteria for antisocial personality dis-order, whereas no appreciable gender differences were identified for rates of antisocial personality disorder or conduct disorder before the age of 15. Female subjects had a considerably higher rate of suicide attempts than men. Upon initial assessment, women were more likely than the men to be at risk for suicide. On logistic regression analysis, suicidal attempts were significantly associated with gender (OR, 23.2; 95% confidence interval [CI], 5.9–91.7, P < 0.001) and major depressive disorder (OR, 19.6; 95%CI, 4.5–85.8, P < 0.001), but not with methamphetamine abuse (P = 0.617).
DISCUSSION
This study demonstrated that heroin abusers in Taiwan who seek treatment have high psychiatric morbidity.
Compared with male subjects, female heroin users more frequently had a DSM-IV axis I psychiatric dis-order other than a drug use disdis-order. Female subjects had a markedly higher rate of mood disorders than the men, and were 11-fold more likely than the men to exhibit suicidal behavior. Furthermore, compared to the men, women were younger, had less education and had earlier onset of illicit drug use. Methamphetamine was the most commonly used concomitant illicit drug. Approximately 85% of heroin abusers in the present study had tried methamphetamine at least once.
Complicating treatment of heroin users is that comorbidity is common. Approximately one-third of subjects in the present study were diagnosed with at least an axis I psychiatric disorder other than a sub-stance use disorder (anxiety and mood disorders were predominant). Prevalence of mood disorders, anxiety disorders and antisocial personality disorders in the present study was 16.8%, 28.4% and 39.7%, respec-tively, and higher than those previously reported in community surveys of the general population in Taipei, Taiwan.23 The association of heroin abuse and those
aforementioned psychiatric disorders is in large part consistent with the findings of psychiatric comorbidity in use disorders of other psychoactive drugs.2,5 In
examining gender differences in comorbidity with substance-use disorders, physicians should bear in mind the gender differences in psychiatric disorders in the general population.24 Epidemiological surveys
indicated that in the general population, anxiety and mood disorders are more common in women, whereas antisocial personality disorder is more common in
men.10,11,25
From an epidemiological perspective,26 a number of
possible explanations exist for the observed association between heroin abuse and these comorbid conditions. First, heroin abuse and these comorbid psychiatric ill-nesses may share common etiologies. Second, heroin abuse may cause some psychiatric disorders, or reveal a previously latent psychiatric illness. Third, certain psy-chiatric disorders may lead to heroin use disorder; this could occur through self-medication.27 If comorbid
psychiatric disorders resulted in heroin abuse, appro-priate treatments of these comorbid disorders can reduce heroin use. Even when comorbid psychiatric disorders result from heroin use, appropriate treat-ments can also improve the relationship between heroin users and medical service personnel. As such, treating illicit drug users for their comorbid psychiatric disorders is critical, regardless of whether the comor-bid psychiatric disorders were caused by or were consequences of heroin use. Drug use prevention strategies should focus on those with a psychiatric dis-order.25 Previous studies found that joint treatment for
opiate dependence and a comorbid mental disorder, such as major depression, improved treatment out-comes.28,29 A recent survey further showed that
associ-ations between most substance use disorders and independent mood and anxiety disorders were over-whelmingly positive and significant, indicating that treatment for a comorbid mood or anxiety disorder should not be withheld from individuals with substance use disorders.30
That as many as 46.9% of female heroin abusers in the present study reported suicidal behaviors warrants special attention to suicide risk in treating female her-oin abusers. A study in Taiwan reported that 35.9% of the female methamphetamine abusers in the detention center exhibited suicidal behaviors.16 Heroin users are
14-fold more likely than the general population to die from suicide.31 The prevalence of attempted suicide
among heroin users is also many orders of magnitude greater than that reported in community surveys. Darke and Ross concluded that the principal risk fac-tors for suicide in the general population also apply to heroin users (gender, psychopathology, family dysfunc-tion and social isoladysfunc-tion), and that heroin users are more likely to be exposed to these factors.31 The
present study identified that female heroin users had been exposed to numerous risk factors reportedly asso-ciated with suicide. For example, compared with male subjects, female heroin users in the present study had less education, high rates of unemployment and comorbid depression, and had earlier onset of heroin and other illicit drug use.
Thie present study also identified a number of social factors that differentiate male and female heroin abus-ers. Compared to men, more female substance abusers are separated or divorced32 and have less frequent
criminal problems.33 Griffin et al. demonstrated that
men are more likely to be employed, have higher level jobs, and to be self-supporting.34 Gender differences
for marital, legal and employment status of subjects in the present study were generally consistent with those in previous reports, although some differences did not reach a level of significance. The present findings also showed that criminal behavior other than illicit drug use was common among heroin abusers. Approxi-mately 11.0% of subjects reported a family history of illicit drug use. Of female heroin users, 34.4% reported living with drug or alcohol abusers. Having sexual part-ners who abused drugs has been previously reported to significantly influence female drug use; most female subjects who inject heroin were given their first injec-tion by a male sexual partner.35 In the present study,
women were significantly younger and had significantly earlier onset of heroin use and illicit drug use than men. This analytical finding is consistent with gender
differences for onset time among heroin abusers or methamphetamine abusers reported previously in Taiwan.16,36
With regard to mode of use, an alarming 85.2% of heroin users in the present study currently injected heroin. One likely reason for this large proportion is that unlike Western countries, needles can be bought without a prescription in Taiwan and, hence, needles for injection are easily obtained. The danger in sharing needles should be underscored, because the number of acquired immunodeficiency (AIDS) virus carriers has increased substantially in Taiwan. Powis et al. reported that among heroin users in the community, women use smaller amounts of heroin for a shorter duration, and are less likely to inject than male users.35 However, in
the present study, the majority of the heroin users, both the male and the female subjects, injected heroin. Her-oin injection is often associated with herHer-oin overdose, viral infection, abnormal liver function, severe drug use pattern and poly drug use.37–39
Some other study limitations might have affected interpretation of the results. First, this cross-sectional design does not permit elucidation of the temporal relationship between time-varying factors, such as the duration of experiencing psychiatric disorders. Another limitation is that all data were self-reported and can be affected by recall and observer bias. Such biases, which could not be excluded, were minimized by using highly structured interviews and trained researchers. Third, heroin users seeking treatment were not a probabilistic sample and many characteris-tics identified in the present sample may not be gener-alizeable to all heroin users. Fourth, the MINI does not assess all personality disorders. Among personality dis-orders, borderline personality disorder should not be overlooked. Indeed, many of the subjects reported risk-taking behaviors, self-destructive behaviors and depressive episodes. It would be interesting to study their personality in further detail using some personal-ity inventories. The MINI does not either specifically classify drug-induced mood disorders or drug-induced psychotic disorders. Studies in the future should pay particular attention to differentiating drug-induced mood or psychotic disorder from functional mood or psychotic disorders.
To summarize, both the men and the women among treatment-seeking heroin abusers had high comorbid rates for psychiatric illnesses. Among heroin abusers in Taiwan, certain gender differences exist for rate of comorbid psychiatric illnesses, particularly depressive disorders. Among heroin users, female subjects were exposed more widely to unfavorable factors and had an overwhelmingly higher incidence of exhibiting sui-cidal behavior than male subjects. Drug treatment
cen-ters should be aware of these gender differences and pay particular attention to comorbid depressive disor-ders and suicidal behaviors of female heroin users.
ACKNOWLEDGMENTS
This study was supported by the Tao Yuan Psychiatric Center, Taiwan. Additional support was obtained from the National Science Council, Taiwan (NSC93-2314-B-182A-210) for Dr C. K. Chen. Staff and participants at the Tao Yuan Psychiatric Center are appreciated for their assistance.
REFERENCES
1. Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch. Gen. Psychiatry 2001; 58: 503–508.
2. Rounsaville BJ, Weissman MM, Kleber H, Wilber C. Heterogeneity of psychiatric diagnosis in treated opiate addicts. Arch. Gen. Psychiatry 1982; 39: 161–168. 3. Brooner RK, King VL, Kidorf M, Schmidt CW Jr,
Big-elow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch. Gen. Psychiatry 1997; 54: 71–80.
4. Khantzian EJ, Treece C. DSM-III psychiatric diagnosis of narcotic addicts. Recent findings. Arch. Gen. Psychia-try 1985; 42: 1067–1071.
5. Chen CC, Tsai SY, Su LW, Yang TW, Tsai CJ, Hwu HG. Psychiatric co-morbidity among male heroin addicts: Differences between hospital and incarcerated subjects in Taiwan. Addiction 1999; 94: 825–832.
6. Kosten TR, Rounsaville BJ, Kleber HD. A 2.5-year follow-up of depression, life crises, and treatment effects on abstinence among opioid addicts. Arch. Gen. Psychi-atry 1986; 43: 733–738.
7. Rounsaville BJ, Kosten TR, Weissman MM, Kleber HD. Prognostic significance of psychopathology in treated opiate addicts. A 2.5-year follow-up study. Arch. Gen. Psychiatry 1986; 43: 739–745.
8. Rounsaville BJ, Weissman MM, Crits-Christoph K, Wilber C, Kleber H. Diagnosis and symptoms of depres-sion in opiate addicts. Course and relationship to treat-ment outcome. Arch. Gen. Psychiatry 1982; 39: 151–156. 9. Home Office. Statistics of Drug Addicts Notified to the Home Office, United Kingdom, 1991. Home Office Statistical Bulletin. Home Office, London, 1992. 10. Regier DA, Farmer ME, Rae DS et al. Comorbidity of
mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990; 264: 2511–2518.
11. Kessler RC, McGonagle KA, Zhao S et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comor-bidity Survey. Arch. Gen. Psychiatry 1994; 51: 8–19. 12. Brady KT, Grice DE, Dustan L, Randall C. Gender
dif-ferences in substance use disorders. Am. J. Psychiatry 1993; 150: 1707–1711.
13. Luthar SS, Cushing G, Rounsaville BJ. Gender differ-ences among opioid abusers: Pathways to disorder and profiles of psychopathology. Drug Alcohol Depend. 1996; 43: 179–189.
14. Kosten TR, Rounsaville BJ, Kleber HD. Ethnic and gen-der differences among opiate addicts. Int. J. Addict. 1985; 20: 1143–1162.
15. Chou P, Liou MY, Lai MY, Hsiao ML, Chang HJ. Time trend of substance use among adolescent students in Tai-wan, 1991–1996. J. Formos. Med. Assoc. 1999; 98: 827– 831.
16. Lin SK, Ball D, Hsiao CC, Chiang YL, Ree SC, Chen CK. Psychiatric comorbidity and gender differences of persons incarcerated for methamphetamine abuse in Tai-wan. Psychiatry Clin. Neurosci. 2004; 58: 206–212. 17. Chiang SC, Chen SJ, Sun HJ, Chan HY, Chen WJ.
Her-oin use among youths incarcerated for illicit drug use. Psychosocial environment, substance use history, psychi-atric comorbidity, and route of administration. Am. J. Addict. 2005; 15: 233–241.
18. Sheehan DV, Lecrubier Y, Sheehan KH et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998; 59 (Suppl. 20): 22–33.
19. Nascimento I, Nardi AE, Valenca AM et al. Psychiatric disorders in asthmatic outpatients. Psychiatry Res. 2002; 110: 73–80.
20. Ritchie K, Artero S, Beluche I et al. Prevalence of DSM-IV psychiatric disorder in the French elderly population. Br. J. Psychiatry 2004; 184: 147–152.
21. Kuo CJ, Tang HS, Tsay CJ, Lin SK, Hu WH, Chen CC. Prevalence of psychiatric disorders among bereaved sur-vivors of a disastrous earthquake in Taiwan. Psychiatr. Serv. 2003; 54: 249–251.
22. Chou FH, Chou P, Su TT et al. Quality of life and related risk factors in a Taiwanese Village population 21 months after an earthquake. Aust. NZ J. Psychiatry 2004; 38: 358–364.
23. Hwu HG, Yeh EK, Chang LY. Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule. Acta Psychiatr. Scand. 1989; 79: 136– 147.
24. Brady KT, Randall CL. Gender differences in substance use disorders. Psychiatr. Clin. North Am. 1999; 22: 241– 252.
25. Turner RJ, Gil AG. Psychiatric and substance use disor-ders in South Florida: racial/ethnic and gender contrasts in a young adult cohort. Arch. Gen. Psychiatry 2002; 59: 43–50.
26. Murray RM, Grech A, Phillips P, Johnson S. What is the relationship between substance abuse and schizophre-nia? In: Murray RM, Jones P, Susser E, van Os J, Cannon M (eds). The Epidemiology of Schizophrenia. Cam-bridge University Press, CamCam-bridge, 2002; 317–342. 27. Khantzian EJ. The self-medication hypothesis of
addic-tive disorders: Focus on heroin and cocaine dependence. Am. J. Psychiatry 1985; 142: 1259–1264.
28. Woody GE, O’Brien CP, Rickels K. Depression and anx-iety in heroin addicts: A placebo-controlled study of dox-epin in combination with methadone. Am. J. Psychiatry 1975; 132: 447–450.
29. Nunes EV, Quitkin FM, Donovan SJ et al. Imipramine treatment of opiate-dependent patients with depressive disorders. A placebo-controlled trial. Arch. Gen. Psychi-atry 1998; 55: 153–160.
30. Grant BF, Stinson FS, Dawson DA et al. Prevalence and co-occurrence of substance use disorders and indepen-dent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry 2004; 61: 807–816. 31. Darke S, Ross J. Suicide among heroin users: Rates, risk
factors and methods. Addiction 2002; 97: 1383–1394. 32. Lex BW. Gender differences and substance abuse. Adv.
Alcohol Subst. Abuse 1991; 4: 225–296.
33. Lancaster FE. Gender differences in the brain: Implica-tions for the study of human alcoholism. Alcohol Clin. Exp. Res. 1994; 18: 740–746.
34. Griffin ML, Weiss RD, Mirin SM, Lange U. A compari-son of male and female cocaine abusers. Arch. Gen. Psy-chiatry 1989; 46: 122–126.
35. Powis B, Griffiths P, Gossop M, Strang J. The differences between male and female drug users: Community sam-ples of heroin and cocaine users compared. Subst. Use Misuse 1996; 31: 529–543.
36. Chen CK, Shu LW, Liang PL, Hung TM, Lin SK. Drug use patterns and gender differences among heroin addicts hospitalized for detoxification. Chang Gung Med. J. 1998; 21: 172–178.
37. Gossop M, Griffiths P, Powis B, Williamson S, Strang J. Frequency of non-fatal heroin overdose: Survey of her-oin users recruited in non-clinical settings. BMJ 1996; 313: 402.
38. Chen CK, Su LW, Lin SK. Characteristics of hospitalized heroin smokers and heroin injectors in Taiwan. Chang Gung Med. J. 1999; 22: 197–203.
39. Carpenter MJ, Chutuape MA, Stitzer ML. Heroin snort-ers vsnort-ersus injectors: Comparison on drug use and treat-ment outcome in age-matched samples. Drug Alcohol Depend. 1998; 53: 11–15.