Risk Factors of Falling among the Elderly in Taiwan:
A Longitudinal Study
Hui-Chuan Hsu1, Li-Jyun Jhan2
Abstract
Objectives: This study aimed to analyze the prevalence of falls and repeated falls of national elderly samples and to explore the risk factors of falls.
Methods: Data were obtained from the “Survey of Health and Living Status of the Elderly in Taiwan” conducted in 1996 (n=2,669) and 1999 (n=2,310). The related risk factors of falls included demographic variables, chronic diseases, disability and changes in physical function, depressive symptoms, exercise behavior, and use of assistive devices (walker/sticks or glasses). Logistic regression was used for analysis.
Results: The prevalence of falls was 19.5%, with 12.3% single fall and 7.2%
repeated falls. The risk factors of falls included being female, having disability, reduced ADL function, with depressive symptoms, using stick/walker but walking well, and not wearing glasses but not seeing clearly. Among the fallers, 73.8%
reported fear of falls, and 45.1% attributed their falls to environmental causes.
Conclusion: Physical and psychological factors as well as environmental factors may cause falls and injuries for elderly. Physicians in the fields of geriatrics or family medicine should pay more and closer attention to the possible risks of their senior patients; home safety and appropriateness of assistive devices for the elderly should be regularly evaluated and carefully maintained.
(Taiwan Geriatrics & Gerontology 2008;3(2):141-154) Key words: falls, elderly, longitudinal study, risk factors
1Department of Healthcare Administration, Asia University; 2Central-South Regional Alliance of DOH Hospital, Executive Yuan.
Correspondence to: Hui-Chuan Hsu, Associate Professor, Institute of Healthcare Administration, Asia University. 500, Lioufeng Road, Wufeng Township, Taichung, 413, Taiwan.
Email: gingerhsu@seed.net.tw
Introduction
Accidents and their adverse effects constituted the fifth cause of death in 2005, and accidental falls ranked second among accident events [1]. The prevalence of falls was 17.2-29.3% for male and 13.4-50.8% for female [2-11]. Falls is also a major health risk for the elderly. Past research has found that the fall mechanism and injury severity were related to the impact of falls. Falls happened outdoors, the vertical and horizontal displacement of body’s center-of-gravity before falls, as well as forward and sideways falls result in more severe injuries [12]. Older age, poor balance and gait were related to inability to get up after falls, and these fallers were more likely to be hospitalized or
institutionalized in nursing homes, or having functional limitation longer [13].
Risk factors to falls for the elderly include advanced age, gender (female), lower educational level, living alone, arthritis, rheumatic disorders, stroke, diabetes, foot ulcers, vision or hearing problem, dizziness, gait balance,
orthostatic hypotension, physical function, urinary incontinence, depressive
symptoms, cognitive impairment, fear of falls, sleep disturbance, use of certain medications, low fall efficacy, and sedentary lifestyle [2, 7, 9, 14-30].
Previous fall experience constitutes the risk of repeated falls [7,11,31-33].
Some studies focused on the
protective factors of falls. Exercise may reduce the incidence of falls [2,14,25].
More family networks contribute to lower incidence of falls for older community women [34].
Although many studies have explored the risk factors of falls, studies of
longitudinal risk factors with national elderly samples were scare. Furthermore, the personal risk factors are usually difficult to change in the old age, but environmental factors and appropriate use of assistive devices (such as glasses or sticks) are changeable relatively. How much falls related to such changeable factors have not been well explored. In this research, we analyzed the prevalence of falls and repeated falls using longitudinal data of Taiwan representative elderly samples and explored risk factors of falls.
We hoped to provide more evidence concerning risk factors of falls among elderly and further contribute to falls prevention
Methods
Data and samples
Data were obtained from the “Survey of Health and Living Status of the Elderly
in Taiwan”, which was first launched in 1989. Face-to-face interviews were conducted with a random sample of individuals (aged ≥ 60 in 1989) derived from the entire Taiwanese elderly
population, including those in institutions.
A three-stage proportional-to-size
probability sampling technique was used.
The first stage consisted of a stratified sample of the administrative units (townships); the second consisted of blocks in the selected townships; and the third consisted of two respondents selected systematically from the register in each selected neighbourhood. The initial
interviews were followed up by subsequent face-to-face interviews in 1993, 1996, and 1999. The lost cases were due to death or loss of follow-up. In this paper, we only used the data of 1996 (n = 2,669) and 1999 (n = 2,310). Incomplete cases were not analyzed. According to the results of the goodness-of-fit test of gender and age, the lost cases were mostly of more advanced age and of males.
Measures
The dependent variable “falls” was defined as any experience of falls in the past year (including any falls, such as falls when walking, slipped, falls due to did not sit/stand well, falls due to dizzy, or falls when lying down from bed, whether
caused injuries or not), and the times of falls in the past year. “Repeated falls” was defined as more than two falls. In 1999, those elderly who had fall experience were further asked if they were afraid of falls and if they would reduce going out owing to fear of falls. They were also asked to evaluate if their most severe fall was due to environmental factors or personal factors (such as dizzy, chest pain, frailty, etc.).
Health status examined included the following. (1) Chronic diseases: The participants self-reported if they have the following diseases: hypertension, diabetes, heart disease, stroke, cancer, bronchitis, arthritis, ulcer, liver disease, cataract, glaucoma, TB, kidney disease, gout, anemia, hip fracture, other fractures, or major injuries. The prevalence of different chronic diseases was calculated using the 1996 data. (2) Disability: Disability was measured by activities of daily living (ADL) and instrumental activities of daily living (IADL) in 1996 and 1999. ADL disability indicates any difficulties in taking bath, dressing, eating, transferring, walking indoors, or going to toilet, with the difficulty lasting for at least 3 months.
IADL disability means any difficulties in doing groceries, money management, taking public transportation alone, heavy housework, light housework, or making phone calls for at least 3 months. Changes
in ADL/IADL were measured by comparing the disability status at two waves and classified as ‘improved or no change’ and ‘worse’. (3) Depressive symptoms in 1996 and 1999 were measured by the short version of the Center for Epidemiologic Study
Depression Scale (CES-D) [35], and the cut-point of having depressive symptoms was decided by using T-score
transformation [36]. Changes in depressive symptoms were measured by comparing the depressive symptoms at two waves, and classified ‘improved or no change’ and
‘worse’.
Health behavior and using assistive devices examined included the following.
(1) Exercise behavior was defined as doing exercise 3 times a week and 30 minutes or more each time, categorized as yes/no.
Exercise behavior was measured in 1996 and 1999. Changes in exercise behavior were measured by comparing the exercise behavior at two waves and categorized as
‘improved or no change’ and ‘worse’. (2) Use of assistive devices in 1999: The participants were asked if they wore glasses (including reading glasses and contact lens) or used walkers/sticks.
Whether they wore glasses or used walkers/sticks or not, all the participants were also asked if they could see clearly (five degrees from very clear to very unclear) or walk well (five degrees from
very well to very unwell).
Demographic variables included age, gender, educational level (illiterate, elementary school, junior high school or higher), marital status (single/married), and living arrangement (living with others or alone).
Analysis
We used descriptive statistics, Chi-square test, and logistic regression models for analysis in this study. Logistic regression analysis was used to explore the odds ratio of related factors to the risk of falls. The dependent variable was any falls happened, and the independent variables included the demographics, chronic diseases, ADL/IADL disability and
change, depressive symptoms and change, using glasses or sticks/walkers and if they used it well. The chronic diseases which were significantly related to falls would be used in the full model of logistic
regression analysis. In order to reduce the full model, we also used stepwise logistic regression analysis by setting alpha of 0.05. Only the coefficients of retained variables were reported in the reduce model.
Results
Demographic characteristics for the
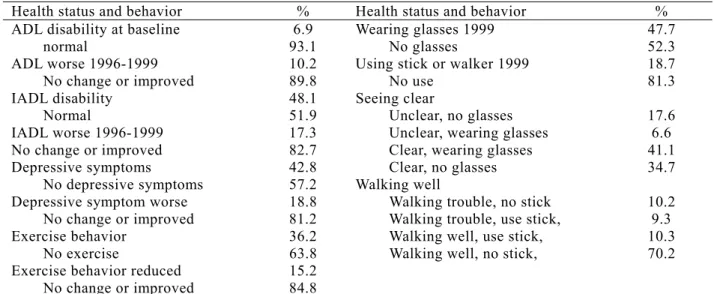
samples at baseline (in 1996) are displayed in Table 1. Table 2 shows the health status and health behaviors, including the status at 1996 and the change from 1996 to 1999.
During the three years, the health status declined rapidly: 10.2% ADLs, 17.3%
IADLs and 18.8% with more depressive
symptoms. Among the participants, 36.2%
had exercise and about 15.2% reported their exercise frequency reduced.
Regardless whether they wore glasses or used sticks/walkers, 24.2% reported they could not see clearly, and 19.5% had walking trouble.
In 1999, of the 2,157 participants, 420 (19.5%) had falls experience, 265 single fall and 155 repeated falls. Table 3 shows the falling characteristics of the fallers.
Among those who had fall experience, 73.8% reported fear of falls, 65.5%
reduced their outdoor activities and 45.1%
perceived that their most severe fall was caused by environment factors but not personal factors.
Table 4 shows the odd ratios of risk factors to falls for the elderly after three years. In the full model (including all the Table 1. Demographic characteristics of the
sample at baseline (1996)
Characteristics %
Age
67-74 63.1
75-84 32.0
85+ 4.9
Gender
Male 55.9
Female 44.1
Education Illiterate 39.3
Elementary school 41.2 Junior high school + 19.5
Marriage
No spouse 41.3
Have spouse 58.7 Living arrangement
Live with others 88.6 Living alone 11.4
Table 2. Health status and health behavior of the samples in 1996 and the change 1996-1999
Health status and behavior % Health status and behavior % ADL disability at baseline 6.9 Wearing glasses 1999 47.7
normal 93.1 No glasses 52.3
ADL worse 1996-1999 10.2 Using stick or walker 1999 18.7 No change or improved 89.8 No use 81.3 IADL disability 48.1 Seeing clear
Normal 51.9 Unclear, no glasses 17.6 IADL worse 1996-1999 17.3 Unclear, wearing glasses 6.6 No change or improved 82.7 Clear, wearing glasses 41.1 Depressive symptoms 42.8 Clear, no glasses 34.7 No depressive symptoms 57.2 Walking well
Depressive symptom worse 18.8 Walking trouble, no stick 10.2 No change or improved 81.2 Walking trouble, use stick, 9.3 Exercise behavior 36.2 Walking well, use stick, 10.3 No exercise 63.8 Walking well, no stick, 70.2 Exercise behavior reduced 15.2
No change or improved 84.8
Note: N=2,669 in 1996 and 2,302 in 1999. The samples in both 2 waves were included in change items.
independent variables), the elderly who had ADLs disability at baseline, IADLs disability at baseline, worse ADLs, using sticks or walkers, not wearing glasses but not seeing clearly, and using sticks/walkers and walking well, would have higher risk to fall after 3 years. In the reduced model by stepwise logistic regression, the risk factors included being female, ADLs disability at baseline, IADLs disability at baseline, worse ADLs, having depressive symptoms at baseline, and using sticks or walkers, were more likely to fall after 3 years.
Discussion
In this study of national elderly samples in Taiwan, the prevalence of falls was 19.5%, with 12.3% of single fall and 7.2% of repeated falls. The risk factors of falls included being female, having ADLs
and IADLs disability, reduced ADLs function, having depressive symptoms, and using sticks/walkers. The elders using sticks/walkers but walking well, and those not wearing glasses but not seeing clearly also had higher risk of falls. Among the fallers, 73.8% reported fear of falls, and 45.1% attributed their falls to
environmental causes.
Disability and changes in physical function were found to be related to the incidence of falls. This finding was consistent with results of previous studies [18,32]. In this longitudinal study we added the changes in physical function and found that dysfunction constituting higher risk of falls. If physical function of the elderly declines rapidly, that may indicate risk of falls increasing. However, the number of ADLs disability can not accurately reflect the dynamic change of physical function in our analysis. One may Table 3. Reducing characteristics of the falling in 1999
Persons (%)
Fallers 420 (100.0)
Falling times
Single fall 265 (63.1%)
Repeated falls 155 (36.9%)
Fears of falls #
No fear 109 (26.2)
Afraid 307 (73.8)
Reduce outdoor activities because fear of falls
No 107 (35.0)
Yes 199 (65.0)
Self-reported falls due to environments#
No 246 (54.9)
Yes 202 (45.1)
Note: # Only falling samples answered the question of fear of falls and environment risks, and for those reported fears of falls were asked about if reducing going out.
have different dominants of ADLs dysfunction, but still showed no change according to our definition.
Having depressive symptom was found to have higher risk of falls, that was similar to past findings [15,18,30,40].
Biderman et al. [15] suggested that there were some common risk factors shared by falls and depression, and to detect these
risks may be easier than to diagnose depression or high risk of falls. Another study showed that older people will suffer from more serious depression after fall injuries [37], indicating that depressive symptoms may be both the cause and result of falls. The elderly who are in risk of fall and depression need to be
monitored more often and more closely by Table 4. Risk of falls of the elderly by logistic regression
Variables Odds ratio of full model Odds ratio of reduced model
Age- 75-84 years old 1.007 --
Age- 85 years old+ 0.718 --
Gender- Female 1.666*** 1.641***
Education- elementary school 0.998 -- Education- primary high school or higher 0.917 -- Marital status—having spouse 1.036 --
Hypertension 0.861 --
Diabetes 0.892 --
Heart disease 1.249 --
Stroke 1.308 --
Arthritis 1.187 --
Cataract 0.798 --
Kidney disease 1.185 --
Anemia 1.151 --
ADL disability 1996 2.510* 2.986***
IADL disability 1996 1.645*** 1.761***
ADL change—worse 1.749* 1.864***
Depressive symptoms 1996 1.186 1.367*
Depressive symptom change- worse 1.149 -- Using stick/walker 1999 2.905*** 2.710***
No glasses and unclear sight 1999 1.212* -- Wear glasses and clear sight 1999 1.060 -- Wear glasses and unclear sight 1999 1.066 -- No stick/walker and walking trouble 1999 1.092 -- Use stick/walker and walking well 1999 1.306*** -- Use stick/walker and walking trouble 1999 0.987 -- -2 Log likelihood
Chi-square 1576.571
165.907 (d.f.=26) 1594.482 147.996 (d.f.=6)
Note1: N=1,809. The independent variables (reference group) included: Gender (male), diabetes (no), heart disease (no), stroke (no), bronchitis (no), arthritis (no), cataract (no), kidney disease (no), anemia (no), ADL disability (normal), IADL disability (normal), change of ADL (no change/improved), change of IADL (no change/improved), exercise (no), depressive symptoms (no), change of depressive symptoms (no change/improved), whether wearing glasses and seeing clear (no glass and seeing clear), whether using stick or walker (no use).
Note 2: Full model was applied the entered logistic regression for analysis; reduce model was applied stepwise logistic regression, which only retained variables are reported in the table.
medical professionals and their family.
It was interesting to find that elderly who did not wear glasses but could not see clearly and those who used sticks/walkers and walking well had higher risk of falls.
Using sticks and walkers should help the disabled or frail elderly walk and live independently, but those who can walk well using assistive devices were more likely to fall, indicating the danger faced by assistive devices users. The possible reasons included inappropriate assistive devices used, unfamiliar uses, paying less attention to environmental risks, or
environmental risks that cannot be avoided. Those elderly who did not wear glasses and could not see clearly had higher risk of falls. That highlight poor eyesight without assistive devices
constitutes a major risk of falls. Northridge et al. [38] found that not only the frail elderly had higher risk of falls; the
vigorous elderly who lived in homes with more hazards also more likely to fall.
Geriatricians should be more concerned with the vision problem in elderly. In addition, the illumination in the house may not be enough and has to be modified.
Previous studies reported that some chronic diseases were related to incidence of falls [8,22,28,39,40]. However, in this study, having chronic diseases were not found to be significantly related to falls in multivariate analysis, although some of the
diseases were related to falls in bivariate analysis, such as hypertension, diabetes, heart disease, stroke, arthritis, kidney disease, and anemia. Multivariate logistic regression analysis also showed no
significant relationship between the elderly who had exercise habit and lower risk of falls.
This study found that 45.1% of falls had causes related to environmental factors. A previous study reported the perceived causes of falls for the
community elderly were mainly balance and gait, which was 61.9%, followed by accident or environments, 15.8% [26]. The environmental factors leading to fall included uneven surface, objects on surface/rug, icy surface, wet surface or slippery footwear, storage problem, lack of safety features in bathroom, and having problem in transfer [26,38].
Another study conducted in Taiwan found that falls happened outdoors were not significantly more severe than those that occurred indoors [12]. For the
community-dwelling elderly, their home is the main setting of their daily lives, and these environmental risks not only result in inconvenience for the disabled elderly but may also constitute the risk of falls and further injuries. We suggest that home safety and modification should be assessed and supplemented in social welfare or long-term care policies.
In this study, 73.8% of the fallers reported their fears of fall, and 65% of them expressed that they would reduce their outdoor activities because of their fear. This proportion was much higher than previous findings, like hospital patients aged 77 years old or above (fear rate of 21.7%) [16] or community elderly women aged 72 or above (fear rate of 27.0%)[23].
The severity and impact of falls were not investigated, so we have no evidence of whether the community elderly had more serious experience of falls. Fear of falls may not constitute a direct risk of future falls, but it was found to be linked with fall-related self-efficacy, which was one of the risks of falls [16]. The fear of falls may influence the daily activity, social
function, and quality of life for the elderly.
The prevention of falls through controlling the internal risk factors and removing external environmental causes should be the basic strategy of reducing fear of falls.
Building self-efficacy for safe exercise and managing falls themselves are also
suggested [31].
There are some limitations in this study. First of all, the longitudinal data were obtained years ago in 1996 and 1999.
Since longitudinal data and national representative samples were not easy to get, this old dataset still provided some important information about the risk of falls. Second, some of the risk factors were
not included in the data, such as use and efficacy of medication, and sleep
disturbance. Third, the fall experience and related variables were only measured in 1999 but not available at baseline or between 1996 and 1999. We thus cannot analyze if previous experience of repeated falls would be related to future falls.
Moreover, the impact and severity of falls were not measured in the analysis. Fourth, the numbers of falls were according to the participants’ reported experience in the past year. Therefore, the mild falls might not be reported, and there may be recall bias in the numbers of falls. Therefore, the prevalence of falls might be
underestimated.
Personal physical and psychological risks as well as environmental risks of falls may cause falls and injuries for the elderly.
The physicians of geriatrics or family medicine should pay more attention to possible risks of their elder clients, and the home safety for the elderly should be noticed. In addition, the use of assistive devices including glasses, sticks or
walkers are common in the elderly, but the appropriateness of those devices should be examined carefully.
Acknowledgement
This study is based on data from the
“Survey of Health and Living Status of the
Elderly in Taiwan” 1996 and 1999, provided by the Population and Health Research Center, Bureau of Health Promotion. The interpretation and conclusions contained herein do not represent those of Bureau of Health Promotion.
Reference
1. Department of Health. Health statistics, 2005.
http://www.doh.gov.tw/statistic/index.h tm. [Feb 24, 2007 accessed]
2. Chan KM, Pang WS, Ee CH, Ding YY, Choo P:Epidemiology of falls among the elderly community dwellers.
Singapore Med J 1997; 38: 427-31.
3. Dargent-Molina P, Favier F, Grandjean H, et al: Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 1996; 20: 145-9.
4. Lin MR, Tsai SL, Chen SY, Tseng SJ:
Risk Factors for Elderly Falls in a Rural Community of Central Taiwan.
Taiwan J Public Health 2002;
21:73-82. [In Chinese]
5. Liu WL: The identification of fall risks among community elderly. Project research report granted by Department of Health, 1991 (No: DOH86-TD-078).
[In Chinese]
6. Nevitt MC, Cummings SR, Kidd S, Black D:Risk factors for recurrent
nonsyncopal falls.J Am Med Assoc 1989; 261: 2663-8.
7. Schwartz AV, Villa ML, Prill M, Kelsey JA, et al: Falls in older Mexican-American women. J Am Geriatrics Soc 1999; 47:1379.
8. Schwartz AV, Hillier TA, Sellmeyer DE, Resnick HE, Gregg E, Ensrud KE, et al: Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care 2002; 25:
1749-54.
9. Stalenhoef PA, Diederiks JP,
Knottnerus JA, de Witte LP, Crebolder HF: The construction of a patient record-based risk model for recurrent falls among elderly people living in the community. Fam Pract 2000; 17:
490-6.
10. Wu CS, Chen CP, Lee FC, Lee SD:
Prevention intervention to elderly fall in the community. Project research report granted by Department of Health, 1993 (No:
DOH82-HP-27-5S05). [In Chinese]
11. Yasumura S, Haga H, Nagai H, Suzuki T, Amano H, Shibata H: Rate of falls and the correlates among elderly
people living in an urban community in Japan. Age Ageing 1994; 23:323-7.
12. Leung WS, Chi HT, Hu MH, Liu MT:
Fall mechanism and injury severity in community dwelling older people.
Formosa J Phy Ther 2005; 30: 105-15.
[In Chinese]
13. Tinetti ME, Liu WL, Claus EB:
Predictors and prognosis of inability to get up after falls among elderly
persons. J Am Med Assoc 1993; 269:
65-70.
14. Carter ND, Khan K, McKay HA, Petit MA, Waterman C, Heinonen A, et al.:
Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis:
randomized controlled trial. CM A J 2002; 167: 997-1004.
15. Biderman A, Cwikel J, Fried AV, Galinsky D: Depression and falls among community dwelling elderly people: a search for common risk factors. J Epidemiol Community Health 2002; 56: 631-6.
16. Cumming RG, Salkeld G, Thomas M, Szonyi G: Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. Prospective study of the impact of fear of falling on
activities of daily living, SF-36 scores, and nursing home admission. J
Gerontol A Biol Sci Med Sc. 2000
;55:M299-305.
17. Hill EL, Cumming RG, Lewis R, Carrington S, Le Couteur DG: Sleep disturbances and falls in older people.
J Gerontol A Biol Sci Med Sci 2007;
62A: 62-6.
18. Jørgensen L, Engstad T, Jacobsen BK:
Higher incidence of falls in long-term stroke survivors than in population controls: depressive symptoms predict falls after stroke. Stroke 2002; 33:
542-7.
19. Kenneth E, Covinsky E, Kahana B, et al: History and mobility exam index to identify community-dwelling elderly persons at risk of falling. J Gerontol A Biol Sci Med Sci 2001; 56A: M253-9.
20. Koshki K, Luukinen H, Laippala P, Kivela SL: Physiological factors and medications as predictors of injuries falls by elderly people: a prospective population-based study. Age Ageing 1996; 26: 29-38.
21. Lamb Se, Ferrucci L, Volapto S, Fried LP, Guralnik JM: Risk factors for falling in home-dwelling older women with stroke: The Women’s Health and Aging Study. Stroke 2003; 34:
494-501.
22. Lawlor DA: Association between falls in elderly women and chronic women and chronic diseases and drug use:
cross sectional study. Br Med J 2003;
327: 805-7.
23. Murphy SL, Dubin JA, Gill TM: The development of fear of falling among community-living older women:
predisposing factors and subsequent fall events. J Gerontol A Biol Sci Med Sci 2003; 58A: 943-7.
24. Richardson DR, Hicks MJ, Walker RB:
Falls in rural elders: an empirical study of risk factors. J Am Board Fam Pract 2002; 15: 178-82.
25. Stalenhoef PA, Diederiks JP,
Knottnerus JA, Kester AD, Crebolder HF: A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol 2002; 55:1088-94.
26. Talbot LA, Musiol RJ, Witham EK, Metter EJ: Falls in young, middle-age and older community dwelling adults:
perceived cause, environmental factors and injury. BMC Public Health 2005;
5: 1186-1147.
27. Vellas B,Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ: Fear of falling and restriction of mobility in eldly fallers. Age Ageing 1997;
26:189-93.
28. Volpato S, Leveille SG, Blaum C, Fried LP, Guralnik JM: Risk factors for falls in older disabled women with diabetes:
The Women’s Health and Aging Study.
J Gerontol A Biol Sci Med Sci 2005;
60A:1539-45.
29. Wallace, C, Reiber G, LeMaster J, Smith DG, Suillivan K, Hayers S, Vath C: Incidence of falls, risk factors for falls, and fall-related fractures in individual with diabetes and a prior foot ulcer. Diabetes Care 2002; 25:
1983-6.
30. Whooley MA, Kip KE, Cauley JA, Ensrud KE, Nevitt MC, Browner WS:
Depression, falls, and risk of fracture in older women. Arch Int Med 1999;
159: 484-90.
31. Andresen EM, Wolinsky FD, Miller JP, Wilson MMG, Malmstrom Tk, Miller DK: Cross-sectional and longitudinal risk factors for falls of falling, and falls efficacy in a cohort of middle-aged African Americans. Gerontologist 2006; 46: 249-57.
32. Tinetti ME, Inouye, K, Gill TM, Doucette JT: Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndrome. J Am Med Assoc 1995; 273; 1348-53.
33. Wyller TB. Risk factors for serious fall related injury in elderly women living at home. Inj Pre 2004; 10: 308-13.
34. Faulkner KA, Cauley JA, Zmuda JM, Griffin JM, Nevitt MC. Is social integration association with the risk of falling in older community-dwelling women? J Gerontol A Biol Sci Med Sci 2003; 58A: 954-9.
35. Radloff LS. The CES-D scale: a self-report depression scale for
research in the general population. App Psycho Measurement 1977; 1:
385-401.
36. Kohout FJ., Berkman L, Evans DA, Huntley JC: 1993 “Two shorter forms
of the CES-D Depression Symptom Index”. J Aging Health 1993; 5:
179-93.
37. Scaf-Klomp W, Sanderman R, Ormel J, Kempen GIJ: Depression in older people after fall-related injuries: a prospective study. Age Ageing 2003;
32: 88-94.
38. Northridge ME, Nevitt MC, Kelsey JL, Link B. Home hazard and falls in the elderly: the role of health and
functional status. Am J Public Health
1995; 85: 509-5.
39. Hanlon JT, Landerman LR, Fillenbaum GG, Studenski S. Falls in African American and white community- dwelling elderly residents. J Gerontol A Biol Sci Med Sci 2002; 57:M473-8.
40. Huang SC, Chen TJ, Chou P.
Cumulative incident rate and
associated factors of falls among the elderly in Shih-Pai, Taiwan. Taiwan J Public Health 2005; 24: 136-45.
台灣老人跌倒危險因子之探討
徐慧娟1 詹莉君2
摘 要
目的:本研究目的在應用全國代表性長期追蹤樣本,分析老人跌倒盛 行率及其相關危險因子。
研究方法:資料來自國民健康局「老人生活與保健調查」1996年與1999
年長期追蹤資料,1996年為2,669人,1999人為2,310人。相關危險因子變
項包括人口變項、慢性病、身體功能障礙及其變化、憂鬱症狀、運動習 慣、使用柺杖或助行器以及是否行走正常、戴眼鏡以及是否看得清楚等
。以邏輯式迴歸進行分析。
結果:在1999年有19.5%的老人有跌倒經驗,其中7.2%為重複跌倒。
跌倒的相關危險因子包括女性、身體功能失能、身體功能惡化、有憂鬱
症狀、使柺杖或助行器但走路方便、未戴眼鏡且看不清楚等。有73.8%的
跌倒老人都害怕再次跌倒,有45.1%的跌倒老人認為是環境因素造成的。
結論:個人身體與心理因素和環境因素均可能造成老人跌倒與傷害。
老年人之家庭醫師或老年科醫師應對其可能的危險情形具有敏感性,老 年人輔具使用適當性與居家環境安全亦應注意。
(台灣老年醫學暨老年學雜誌 2008;3(2):141-154)
關鍵詞:跌倒、老人、長期追蹤、危險因子
1亞洲大學健康暨醫務管理學系副教授、2署立醫院中醫聯盟 通訊作者:徐慧娟
通訊處:413 台中縣霧峰鄉柳豐路 500 號 Email: gingerhsu@seed.net.tw