ORIGINAL ARTICLE
Changes in Quality-of-Life Following Laparoscopic
Cholecystectomy in Adult Patients with Cholelithiasis
Hen-Hui Lien&Chi-Cheng Huang&Pa-Chun Wang&
Ching-Shui Huang&Ya-Hui Chen&Tzung-Li Lin&
Meng-Chao Tsai
Received: 15 July 2009 / Accepted: 29 September 2009 / Published online: 15 October 2009 # 2009 The Society for Surgery of the Alimentary Tract
Abstract
Background The aim of this study was to evaluate changes in quality-of-life following laparoscopic cholecystectomy (LC) in adults with cholelithiasis.
Methods Patients were evaluated with the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) and the Gastrointestinal Quality of Life Index (GIQLI) preoperatively and 12 months after LC. Outcome predictors were analyzed using correlation and regression statistics.
Results Ninety-nine patients were enrolled (male/female, 32:67, age 49.8±13.7 years old). At baseline, patients performed inferiorly to general population in all SF-36 general health dimensions (p<0.0001). Postoperatively, thephysical”, “role-emotional”, and “bodily pain” dimensions of health significantly improved. There were significant improvements in GIQLI “total”, “physical well-being”, “mental well-being”, “gastrointestinal digestion”, and “defecation” subscales scores. Serum direct bilirubin level and drainage tube indwelling were significant predictors for quality-of-life improvement following LC. Conclusions LC can greatly reduce gastrointestinal symptoms to improve quality-of-life for patients with cholelithiasis. Patients with severe baseline conditions may benefit from greater quality-of-life improvement following LC.
Keywords Cholelithiasis . Laparoscopic cholecystectomy . Quality of life
Introduction
The yearly incidence of gallstone disease may range from a low of 1 in 1,000 young men to 19 in 1,000 elderly women.1An Italian longitudinal population study revealed that the overall 10-year incidence of gallstone disease was 6.3%.2The change of dietary habit with increase intake of calories and cholesterol has led to the escalation of gallbladder disease in many countries.3
The development of laparoscopic cholecystectomy (LC) in the last two decades has partly led to the increase of cholecystectomy. Urbach and Stukel reported that the adjusted annual rate of elective cholecystectomy per 100,000 population in Canada increased from 201.3 in 1988–1990 to 260.8 in 1992–2000.4
Ho et al., attributing to the improvement of nutritional status and living standard in Taiwan, reported steady increase of surgical interventions for gallstones.5
However, there are limited researches in the literatures that have reported LC quality-of-life outcomes.6–10 The quality-of-life impacts of LC and the predictors of patients’
Financial support: Cathay Medical Research Institute grant CMRI-9303.
H.-H. Lien
:
C.-C. Huang:
C.-S. Huang (*) Division of General Surgery, Department of Surgery, Cathay General Hospital,280 Sec.4 Jen-Ai Rd., 106 Taipei, Taiwan e-mail: hhlhhl@cgh.org.tw
H.-H. Lien
:
C.-C. Huang:
P.-C. Wang:
T.-L. Lin:
M.-C. Tsai School of Medicine, Fu Jen Catholic University,Taipei, Taiwan P.-C. Wang
:
Y.-H. ChenQuality Management Center, Cathay General Hospital, Taipei, Taiwan
P.-C. Wang
Department of Public Health, College of Public Health, China Medical University,
subjective outcomes remained undetermined, especially in the Asian context. The aims of this study are to use the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) and Gastrointestinal Quality of Life Index (GIQLI) surveys to report subjective quality-of-life following LC and to investigate the factors that may predict LC quality-of-life outcomes in adults with cholelithiasis.
Materials and Methods
Study Population
The study was conducted in a prospective, nonrandomized manner. A total of 99 consecutive adult patients (aged 18 years or older) who underwent abdominal sonography confirming symptomatic gallstone seeking surgical treat-ment in a tertiary referral medical center were enrolled within a 1-year period (July 2004–June 2005). Patients with stable chronic condition or at acute exacerbation of disease were both included. Approval from institutional review board of Cathay Medical Center was obtained in advance. Patients’ demographic data and health history were reviewed during initial visit. The systemic comor-bidity including diabetes mellitus, hypertension, peptic ulcer, gastroesophageal reflux disease, heart disease, and hyperlipidemia were screened and documented upon entry.
Patients all received routine blood biochemistry workup, including blood cell count, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and total and direct bilirubin. Prior to any medical or surgical intervention, all patients were administered with the International Quality of Life Assessment SF-36 Standard Taiwan version 1.011–13and the Chinese Taiwan version of GIQLI.14 Patients were asked to fill out the surveys by themselves with the assistance from research staff if needed. Patients were evaluated with the SF-36 and GIQLI again 12 months after surgery. Standard four-port LC was performed for all patients.
Quality-of-Life Measure
SF-36
The SF-36 is a widely used generic quality-of-life measur-ing instrument that divides quality of life into eight dimensions, including physical functioning (PF), role-physical (RP), bodily pain (BP), general health, vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH). Each subscale score from 0 to 100, with 100 as the most optimal health status.12,13
GIQLI
The GIQLI is a 36-item survey that evaluates the physical and mental problems associated with gastrointestinal disease on a Likert scale; each survey question has five response levels (0–4, worst to best condition). The GIQLI generates a total score and four subscale scores (physical well-being 0–40, mental well-being 0–20, gastrointestinal digestion 0–40, and gastrointestinal defecation 0–24). The physical well-being (PW) subscale reflects the limitations in physical or social activities directly related to gastrointes-tinal conditions. The remaining subscales are reflective of a patient’s mental (mental well-being, MW), digestion (gas-trointestinal digestion, GDG), and defecation (gastrointes-tinal defecation, GDF) problems. Total and subscale scores are scaled from 0 (worst) to 124 (best).15,16 The Taiwan version GIQLI was validated in previous study.14
Statistical Analysis
Results are expressed as mean±SD. Student’s t test with unequal variance is applied to compare the SF-36 subscale scores of gallstone patients (pre- and postoperative) with 6,109 age- and sex-matched Taiwanese population norms.12,13 Paired t test is used to compare preoperative and postoperative quality-of-life scores. Using the pre-/ postoperative SF-36 and GIQLI score differences as dependent variables, step-wise multiple regression analyses are applied to investigate the effects of patient character-istics, operative information, and preoperative blood bio-chemistry on the quality-of-life changes following LC.
Results
Study Population
There are 32 males and 67 females (mean age 49.8±13.7 years; range 23 to 75) in this study cohort. Comorbidities were observed in 39% of the patients, including hypertension (18), heart disease (eight), diabetes mellitus (11), GERD (seven), and others (16). There are 76 with chronic stable (biliary colic only) condition (mean age 48.95±12.30 years, male/female 25:51) and 26 with acute exacerbation (acute cholecystitis) condition (mean age 52.0±16.92 years, male/female 8:18).
Stable chronic and acute exacerbations of gallstone disease are defined as the following: Patients of known cholelithiasis for at least 3 months prior to operation with symptoms no more than biliary colic are considered as under stable chronic condition; on the other hand, patients with acute exacerbation of gallstone may suffer from elevated inflammatory serum marker, fever, jaundice, right upper abdomen tenderness, or other gastrointestinal
symp-toms related to cholecystitis. Twenty-six patients are grouped into gallstone with acute exacerbation according to the aforementioned definition, and all have GIQLI total scores less than 80. There is no significant difference regarding age and sex distributions between chronic stable and acute exacerbation disease.
Operation
The mean operation time was 55±31 min; 15 (15.2%) patients had subhepatic close suction drainage tube (Jackson–Prett type) placed after LC. The mean total length of stay was 3 days. There was no bile leak, no wound infection, and no surgical mortality. Multiple stones were identified in 57 patients. The mean size of stone was 9.7±7.4 mm. The histopathology examination showed 30 cholesterol and 69 noncholesterol stones.
There was no conversion to open surgery in this study population. The follow-up rate was 100% at 12 months after operation.
Quality-of-Life Improvement in SF-36
All eight SF-36 subscale scores from preoperative gallstone patients were significantly lower than those form Taiwanese population norms (t test, p<0.0001). Compared with preop-erative quality-of-life status, three out of eight SF subscale domain showed significant improvement (paired t test): RP 20.9% (p=0.003), BP 27.8% (p<0.0001), and RE 17.7% (p= 0.0069; Fig.1). Even after operation, gallstone patients still performed inferiorly to matched general population in seven out of eight SF-36 health dimensions except for RE (Fig.1).
Quality-of-Life Improvement in GIQLI
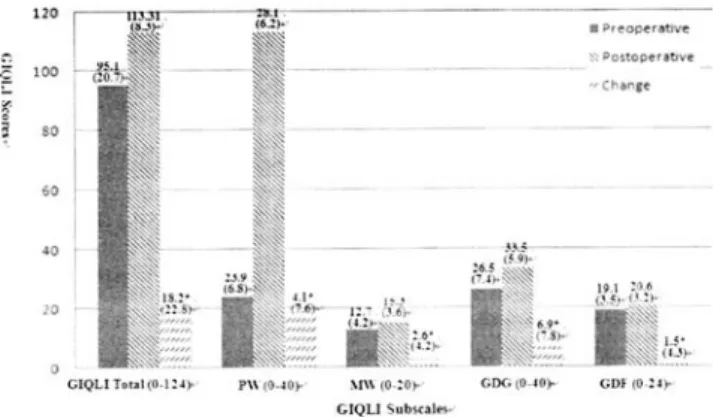
Total and all GIOLI subscale scores (PW, MW, GDG, and GDF) improved significantly (paired t test, p<0.0001) following LC surgery (Fig. 2), indicating remarkable
recovery of gastrointestinal symptoms or disabilities. Compared with preoperative GIQLI survey, the degrees of improvement were 19.1% for GIQLI total, 17.2% for PW, 20.4% for MW, 26% for GDG, and 7.8% for GDF scores.
Quality-of-Life Outcome Predictors
Step-wise multiple regression models revealed that patients’ characteristics and serum biochemistry markers had various impacts upon postoperative quality-of-life changes as compared with preoperative baseline. Direct bilirubin was a strong predictor for SF-36 PF (adjust R2=0.14,β=33.4, p < 0.01) and BP (adjust R2= 0.15, β=35.1, p<0.05) subscale scores improvements. Postoperative drain tube indwelling was predictive of BP (adjust R2=0.15,β=24.1, p<0.01), VT (adjust R2=0.10,β=16.1, p<0.01), SF (adjust R2=0.11, β=13.8, p<0.05), and MH (adjust R2=0.03,β= 12.4, p < 0.05) SF-36 dimensions scores gains 1 year following LC intervention.
Direct bilirubin was also a significant predictor in the changes of total (adjust R2=0.13,β=32.8, p<0.01), GDG (adjust R2=0.20, β=15.3, p<0.01), and GDF (adjust R2=
Figure 1 Norm and pre-/post-operative SF-36* subscales’ scores (N=99). SF-36 Medical Outcomes Study 36-Item Short-Form Health Survey. *P<0.05: t test, significant differences between preoperative and post-operative SF-36 subscale scores. †P<0.05: t test, significantly different as compared to Taiwa-nese population norm.
Figure 2 Preoperative and postoperative GIQLI scores (N=99). PW physical well-being, MW mental well-being, GDG gastrointestinal digestion, GDF gastrointestinal defecation. *P<0.0001: t test, signif-icant difference between preoperative and postoperative scores.
0.06,β=3.8, p<0.05) subscale scores in GIQLI question-naire. Patients with elevated preoperative direct bilirubin level tended to have greater symptomatic improvements after LC.
Discussion
Cholelithiasis is prevalent among general population. The change of diet habit with increasing calorie intake has led to its higher occurrences among many countries. The devel-opment of LC technique has drastically changed the principle in treating gallstone and cholecystitis; complica-tion rates have steadily declined over years.17,18 The reduced morbidity and mortality rates have made LC a safe and standard procedure to treat benign gallbladder diseases. However, quality-of-life outcomes of LC remain undetermined. It is our interest to understand the impacts of LC to a patient’s well-being and to investigate the factors that may influence the subjective quality-of-life outcomes.
There are limited studies that report the subjective patient quality-of-life outcomes following LC. Vetrhus et al. used quality-of-life and pain surveys to compare chronic gallbladder disease outcomes between observation (conser-vative treatment) and LC groups. The observation group had higher rate (31% vs. 19%) of gallstone-related events, but had similar quality-of-life outcomes with LC group.9 Using GIQLI, Planells et al. detected significant and similar quality-of-life improvements following LC in both calcu-lous and acalcucalcu-lous cholecystitis patients.6 Using both GIQLI and SF-36, Quintana et al. found that patients with symptomatic cholelithiasis and low surgical risk experi-enced the highest quality-of-life gains; patients with asymptomatic cholelithiasis or high surgical risk experi-enced least improvement. The authors concluded that LC is appropriate for patients with symptomatic gallstone and low surgical risk.7 In addition, Mentes et al. observed signifi-cant total GIQLI score improvements in both symptomatic and asymptomatic gallstone groups. The gallstone-related quality-of-life improvements are especially remarkable in symptomatic patients, indicating that gallstone patients with lower baseline GIQLI scores are more likely to benefit from LC.8
The normative Taiwan SF-36 population data provide important references to patients’ pre- and postoperative quality-of-life status in this study. Our data showed that gallstone disease indeed incurred considerable health burdens. The preoperative SF-36 scores from gallstone patients were significantly inferior to the age- and sex-matched population norms in all dimensions. Our data, in consistent with those from others,10 proved that LC can effectively reduce gastrointestinal symptoms, as can be seen from the improvement in GIQLI total, physical well-being,
mental well-being, gastrointestinal digestion, and defeca-tion subscale scores.
However, since patients still did not regain full GIOLI subscales scores after LC, we speculate that some residual gastrointestinal problems may continue to bother patients. This explains the persistent, measurable decrements in many of the SF-36 health dimensions at 12 months following surgery.
Many serum markers have been used to evaluate patients with gallstone. For example, erythrocyte sedimentation rate, C-reaction protein, andα-1 and α-2 globulin were elevated even in asymptomatic gallstone patients.19 Mild to moder-ate hyperbilirubinemia is frequently seen in patients with cholecystitis; around one third of patients may show elevated serum bilirubin level at time of admission.20,21 Preoperative alkaline phosphatase were reported to associ-ate with surgical outcomes by some authors.22–25In current study, we found that both generic SF-36 and digestive system-specific GIQLI survey score improvements in some quality-of-life dimensions can be predicted by preoperative direct bilirubin level and by the placement of drainage tube intraoperatively. This indicates that patients with worse preoperative health condition may benefit from greater quality-of-life improvements following LC surgery.
Conclusion
LC can greatly reduce gallstone-related gastrointestinal symptoms and proves to be an effective therapy to enhance quality-of-life. Serum direct bilirubin is a good predictor for post-LC quality-of-life outcomes. This study suggests that patients with severe cholelithiasis can benefit from greater quality-of-life gains following LC.
Acknowledgment The project is sponsored by Cathay Medical Research Institute grant CMRI-9303.
References
1. Lowenfels AB, Velema JP. Estimating gallstone incidence from prevalence data. Scand J Gastroenterol 1992;27:984–986. 2. Angelico F, Del Ben M, Barbato A et al. Ten-year incidence and
natural history of gallstone disease in a rural population of women in central Italy. The Rome Group for the Epidemiology and Prevention of Cholelithiasis (GREPCO). Ital J Gastroenterol Hepatol 1997;29:249–254.
3. Rahman GA. Cholelithiasis and cholecystitis: changing prevalence in an African community. J Natl Med Assoc 2005;97:1534–1538. 4. Urbach DR, Stukel TA. Rate of elective cholecystectomy and the
incidence of severe gallstone disease. CMAJ 2005;172:1015–1019. 5. Ho KJ, Lin XZ, Yu SC et al. Cholelithiasis in Taiwan. Gallstone characteristics, surgical incidence, bile lipid composition, and role of beta-glucuronidase. Dig Dis Sci 1995;40:1963–1973.
6. Planells RM, Bueno LJ, Sanahuja SA, Garcia ER. Quality of life (GIQLI) and laparoscopic cholecystectomy usefulness in patients with gallbladder dysfunction or chronic non-lithiasic biliary pain (chronic acalculous cholecystitis). Rev Esp Enferm Dig 2004;96:442–451.
7. Quintana JM, Arostegui I, Cabriada J et al. Predictors of improvement in health-related quality of life in patients undergo-ing cholecystectomy. Br J Surg 2003;90:1549–1555.
8. Mentes BB, Akin M, Irkorucu O et al. Gastrointestinal quality of life in patients with symptomatic or asymptomatic cholelithiasis before and after laparoscopic cholecystectomy. Surg Endosc 2001;15:1267–1272.
9. Vetrhus M, Soreide O, Eide GE et al. Quality of life and pain in patients with acute cholecystitis. Results of a randomized clinical trial. Scand J Surg 2005;94:34–39.
10. Johansson M, Thune A, Blomqvist A et al. Impact of choice of therapeutic strategy for acute cholecystitis on patient’s health-related quality of life. Results of a randomized, controlled clinical trial. Dig Surg 2004;21:359–362.
11. New England Medical Center Hospital. IQOLA SF-36 Taiwan Standard Version 1.0. Boston: The Health Institute, New England Medical Center, 1996.
12. Lu JR, Tseng HM, Tsai YJ. Assessment of health-related quality of life in Taiwan (I): development and psychometric testing of SF-36 Taiwan version. Taiwan J Public Health 2003;22:501–511. 13. Tseng HM, Lu JR, Tsai YJ. Assessment of health-related quality
of life (II): norming and validation of SF-36 Taiwan version. Taiwan J Public Health 2003;22:512–518.
14. Lien HH, Huang CC, Wang PC et al. Validation assessment of the Chinese (Taiwan) version of the Gastrointestinal Quality of Life Index for patients with symptomatic gallbladder disease. J Lapa Adv Tech 2007;17:429–434.
15. Eypasch E, Williams JI, Wood-Dauphinee S et al. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg 1995;82:216–222.
16. Neiveen van Dijkum EJM, Terwee CB, Oosterveld P et al. Validation of the gastrointestinal quality of life index for patients with potentially operable periampullary carcinoma. Br J Surg 2000;87:110–115. 17. Hannan EL, Imperato PJ, Nenner RP, Starr H. Laparoscopic and
open cholecystectomy in New York State: mortality, complica-tions, and choice of procedure. Surgery 1999;125:223–231. 18. Steiner CA, Bass EB, Talamini MA et al. Surgical rates and
operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med 1994;330:403–408.
19. Tarocco R, Quaranta LM, Bernal MA et al. Asymptomatic cholelithiasis: indications for cholecystectomy based on the levels of acute phase proteins. Chir Ital 1999;51:207–213.
20. Edlund G, Kempi V, van der Linden W. Jaundice in acute cholecystitis without common duct stones. Acta Chir Scand 1983;149:597–601.
21. Dumont AE. Significance of hyperbilirubinemia in acute chole-cystitis. Surg Gynecol Obstet 1976;142:855–857.
22. Kouroumalis E, Hopwood D, Ross PE, Bouchier IA. Mucosal alkaline phosphatase and bile lipids in the gallbladder in cholecystitis. J Pathol 1983;141:169–179.
23. Choi JW, Pai SH. Serum lipid concentrations change with serum alkaline phosphatase activity during pregnancy. Ann Clin Lab Sci 2000;30:422–428.
24. Huang CS, Lein HH, Tai FC, Wu CH. Long-term results of major bile duct injury associated with laparoscopic cholecystectomy. Surg Endosc 2003;17:1362–1367.
25. Jacobs JK, Cebul RD, Adamson TE. Acute cholecystitis. Evaluation of factors influencing common duct exploration. Am Surg 1986;52:177–181.